If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Sciatica | Mate haiataka
Key points about sciatica
- Sciatica is pain in your buttock and leg that’s caused by pressure on a spinal nerve in your lower back.
- It can be caused by a prolapsed (slipped) disc, pinched nerve or some forms of arthritis.
- Symptoms include pain, numbness, tingling, and weakness in your leg and affects one side only.
- You may also have pain in your back, but the leg pain is normally worse than the back pain.
- There are things you can do yourself to help manage your sciatica.
- Rarely, injections and/or surgery may be recommended.
Call 111 and ask for an ambulance if you experience the following:
- tingling or numbness in both legs and around your buttocks or genitals
- weakness in both legs
- loss of bladder or bowel control, or both (incontinence)
- symptoms of sciatica in both your legs.
These symptoms can be a sign of a serious condition called cauda equina syndrome. This condition is very rare but if you have it, emergency surgery is needed to prevent paralysis.
Sciatica
Sciatica refers to pain in your leg that’s caused by a problem in your lower back that affects the sciatic nerve. The sciatic nerve is a large nerve made up of several spinal nerves that branch from your lower spine in your back through your hips and buttocks and down each leg. If you have sciatica, you usually feel pain along the path of the sciatic nerve, and it usually affects only one side of your body. Sometimes you might also have numbness, tingling or muscle weakness in part of your leg.
Sciatica is more common if you:
- are male
- are 30 to 50 years of age
- drive or sit for more than 2 hours a day
- carry heavy loads at work.
Other minor risk factors include smoking, having a stressful occupation and doing too little or too much physical activity.
Video: What is sciatica? | Patient explainers
Your spine is made up of bones which are called vertebrae, and intervertebral discs (discs for short) that act as cushions between the bones.
The most common cause of sciatica is a prolapsed or herniated disc (also known as a ‘slipped disc’). This is when a disc bulges into 1 or more spinal nerves, or when there is a tear in the outer layer of the disc and the gel-like filling oozes out and irritates a spinal nerve.
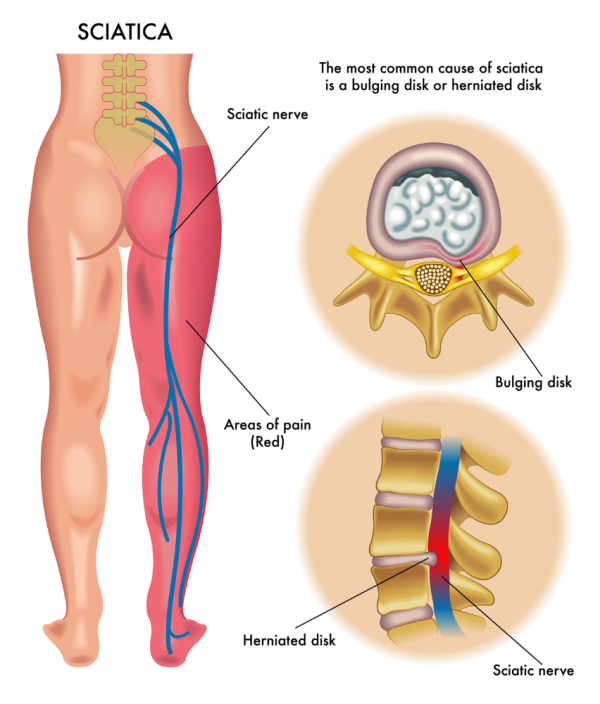
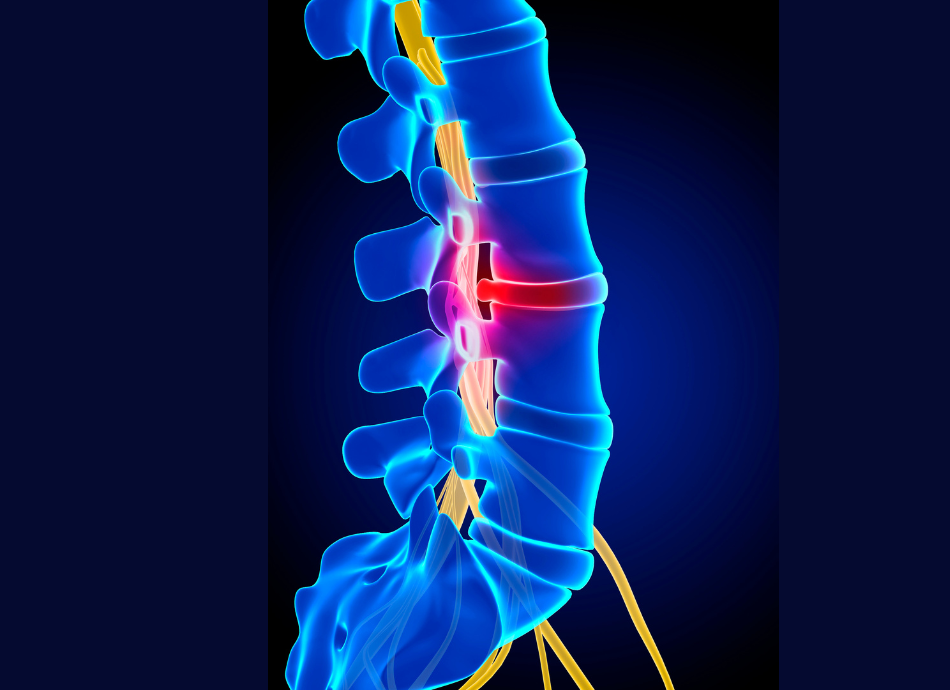
Image credit: Depositphotos
Spinal stenosis is another common cause of sciatica. This is related to getting older and slowly gets worse over time. The parts of your spine that the nerves pass through become narrower, which can irritate or compress 1 or more of your spinal nerves.
Disc herniations and spinal stenosis don’t always cause symptoms. Many people have these conditions and don’t know about it. They’re only a problem if symptoms develop.
Less common causes of sciatica are:
- spondylolisthesis – this is when a vertebra slips out of position and irritates or compresses a nerve root
- a spinal or back injury or infection
- a growth within your spine, such as a tumour
- cauda equina syndrome, a rare but serious condition caused by compressed and damaged nerves in your spinal cord.
The most common symptoms of sciatica are:
- shooting, stabbing, electric shock pain which usually starts in your lower back and buttock and runs down one leg past your knee and sometimes into your calf and foot
- numbness, weakness or pins and needles in a part of your buttock, leg and foot
- lower back pain.
If you only have lower back pain, or if the pain in the leg is in a large area, then it's probably not sciatica.
The most common pattern of pain is down your buttocks and the back of your leg, and into your foot. The pain in your leg is normally worse than the pain in your back or you mightn’t have any back pain at all.
The pain can be mild or severe, and it can start suddenly or gradually. Sneezing, coughing or sitting for a long period of time may make it worse.
See your healthcare provider if you have any of the following:
- severe, ongoing or worsening pain
- weakness or difficulty lifting your foot when walking
- bowel or bladder problems, eg, loss of control or incontinence
- fever or other symptoms that are worrying you.
Your healthcare provider will ask you questions about your symptoms and examine your back and parts of your nervous system. This may include looking at how you walk, how your back and leg move, testing the strength and reflexes in your legs and feet and testing for numbness, tingling or reduced feeling in your leg.
Scans aren’t needed to diagnose sciatica. Most people will get better on their own. Having a scan doesn’t change your treatment and isn’t needed.
Your healthcare provider may arrange an X-ray or an MRI scan if:
- your symptoms or examination suggest:
- you have a different problem
- a cause for your sciatica which needs different treatment.
- your symptoms are not getting better after 6 weeks.
It's common to find a bulging or prolapsed disc on an MRI scan, especially as you get older. They often don't cause any problems, so finding one on a scan doesn't necessarily mean it's causing your symptoms.
Sciatica can improve without specific treatment so your healthcare provider may suggest a watch and wait approach to give your body time to heal naturally. During this time there are things you can do yourself to manage your sciatica.
Painkillers, such as anti-inflammatories (NSAIDs) and paracetamol can help. Read more about pain relief medicines for short term pain. Talk to your healthcare provider about nerve pain medications eg, nortriptyline or amitriptyline, which can also help.
See your healthcare provider if the pain hasn’t improved after trying home treatment for a few weeks, or if it's getting worse or stopping you from doing your normal activities.
You should try and stay as active as possible as this will help your recovery. If you’re worried that movement or activity will make your pain worse, or cause more damage, talk to your healthcare provider. They can help relieve any anxiety or fear you may have so you can continue with your daily activities.
If your symptoms are severe, your healthcare provider may talk to you about seeing a specialist doctor to discuss the following options:
- Steroid injection – these are done using a scanning machine to safely guide the needle into the problem area in your spine where the steroid medicine is injected to reduce swelling and inflammation.
- Surgery – this might be considered if you have severe symptoms or if your symptoms continue for more than a few months. However, it’s uncommon to end up needing surgery for sciatica.
Because the cause of sciatica is often in your back, the treatment is often similar. Read more about back pain treatment.
Sciatica can be a real pain in the backside … and leg, and foot.

Image credit: Canva
There are things you can do yourself to help you manage your sciatica:
- Carry on with your normal activities as much as possible.
- Gentle exercise – regular, gentle exercise and stretching can help your sciatica get better faster.
- Make sure your posture is good when sitting and standing to help speed up your recovery and to prevent problems developing in the future.
- See a physiotherapist – a physiotherapist can help you with treatment and exercises to help your sciatica.
- Heat/cold packs – some people find warm baths or heat/cold packs can help relieve their pain.
- Reduce time spent sitting and lying – try to reduce the amount of time you spend sitting or lying down. Moving and changing positions regularly is the best thing you can do to help get better faster.
- Avoid lifting anything heavy.
- Use a cushion – when you’re lying on your side, put a small firm cushion between your knees to help relieve your pain. If you’re lying on your back, put several firm pillows under your knees.
- Practise relaxation techniques such as yoga, meditation or mindfulness, and do things you enjoy to distract you from the pain.
Because the cause of sciatica is often is your back, self-care is often the same. Read more about back pain self-care.
Apps reviewed by Healthify
You may find it useful to look at some Pain management apps, Physiotherapy and exercise apps, Mediation and mindfulness apps or Breathing apps.
There's no proven way to prevent sciatica. However, the following things may help reduce your chance of getting it:
- Stay physically fit and keep a healthy body weight.
- Take regular breaks if you have a job that involves sitting for longer than 2 hours at a time.
- Do exercises to keep your back and tummy muscles strong and flexible.
- Practise good posture when you’re sitting, standing, exercising or lifting heavy things.
- Avoid lifting heavy loads if you don’t have the strength for it.
- Breathe with your stomach not your chest. You might find a breathing app useful.
- Maintain a healthy lifestyle – stop smoking if you smoke, reduce alcohol intake, eat a healthy diet and exercise regularly.
If your sciatica is caused by a disc herniation, there’s a 50% chance that your leg pain will be better after 4 weeks whether you have any treatment or not. However, the pain can last for several months or longer. Normally leg pain gets better faster than back pain.
Mild sciatica can get better by itself over time. However, if you’re in a lot of pain, if your symptoms get worse, if you have weakness or difficulty lifting your foot when walking, or if your bowel or bladder isn’t working properly, contact your healthcare provider immediately.
Sciatica(external link) Better Health, Australia
Sciatica(external link) NHS, UK
Exercises for sciatica(external link) NHS, UK
Apps
Pain management apps
Physiotherapy and exercise apps
Breathing apps
Meditation and mindfulness apps
References
- Sciatica(external link) NHS, UK, 2020
- Kos BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica(external link) BMJ 2007;334;1313–1317
- Leg pain (sciatica)(external link) Iowa Clinic, US, 2023
- Management of non-specific back pain and lumbar radicular pain(external link) BPAC, NZ, 2009
- Acute low back pain(external link) BPAC, NZ, 2022
- Sciatica(external link) Better Health, Australia, 2015
- Exercises for sciatica problems(external link) NHS, UK, 2022
- Warm up, cool down and stretch(external link) ACC, NZ, 2002
- Tubach F, Beauté J, Leclerc A. Natural history and prognostic indicators of sciatica(external link) Journal of Clinical Epidemiology 2004;57(2):174–179
- Bed rest for acute low back pain and sciatica(external link) Cochrane Database Syst Rev. 2000;(2):CD001254
Cauda equina syndrome(external link) Patient Info, UK, 2016
Lower back pain and sciatica(external link) Patient Info, UK, 2016
Management of non-specific back pain and lumbar radicular pain(external link) BPAC, NZ, 2009
Acute low back pain(external link) BPAC, NZ, 2022
Dahm KT, Brurberg KG, Jamtvedt G, et al. Advice to stay in bed versus advice to stay active or acute low back pain and sciatica(external link) Cochrane Database Syst Rev. 2010;(6):CD007612
Di Mattia F, Tejani S, Hall T. Bed rest for sciatica – a closer look at the evidence(external link) J Orthop Sports Phys Ther. 2018 Jun;48(6):436–438
New Zealand acute low back pain guide(external link) ACC, NZ, 2004
Webinar
Lower back pain – conservative or surgical treatment(external link) Mr John Fergusin and Dr Giresh Kanji, Goodfellow Unit, NZ, 2022
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Ian Martin, Emergency Physician, Waikato
Last reviewed:





