You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Pain relief medicines for short term pain
Also called pain relievers or analgesics
Key points about pain relief medicines for short-term pain
- Pain relief medicines for short-term pain are commonly used for injuries, infections or after surgery.
- They’re usually only needed while the injury, infection or surgery is healing.
- The choice of pain relief medicine can depend on many things, including the type, severity and cause of your pain, other medicines you take and any other health conditions you have.

The content on this page covers medicines for short-term pain. For information about medicines for pain that continues for 3 months or longer, see pain relief medicines for chronic pain. Read more about the difference between acute pain and chronic pain.
What is short-term pain?
Short-term pain is also commonly called acute pain. Acute pain usually occurs because of surgery, injury or infection, such as a dental infection or bone fracture (break). It often comes on quickly, lasts for a short time and goes away as the underlying cause gets better. Pain relieving treatments usually only need to be given for a short time while the injury is healing.
- Paracetamol and NSAIDs are commonly used.
- Opioids are useful and usually only need to be given for a few days. The dose of opioid should be reduced as healing occurs.
- Read more about acute pain.
Severity of the pain
Pain is usually grouped into mild pain, moderate pain or severe pain. The step-wise or ladder approach to managing pain is based on the severity of your pain. It's a 3-step approach.
- Step 1: Mild-to-moderate pain – this type of pain is best treated with paracetamol, ibuprofen and other NSAIDs. Read more about paracetamol and NSAIDs.
- Step 2: Moderate-to-severe pain – more intense pain is treated with mild opioid pain relievers such as codeine and tramadol. These may be used together with paracetamol or NSAIDs.
- Step 3: Severe pain – severe pain is treated with strong opioids such as morphine and oxycodone. These may be used together with paracetamol or NSAIDs. Read more about opioids.
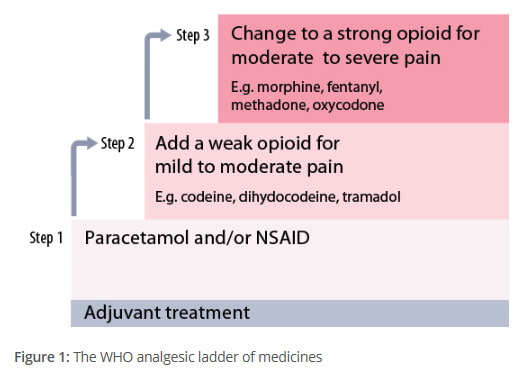
Image credit: The principles of managing acute pain in primary care(external link), BPAC
Paracetamol
Paracetamol is used to treat mild-to-moderate pain.
- It acts mainly in your brain and has an effect on many different ways you feel pain.
- If it's taken at the correct dose it's a safe and useful medicine, and can be effective for many different types of pain.
- For most types of acute or short-term pain you only need to take paracetamol when you feel the pain.
- It can be combined in the same tablet with caffeine or codeine for added benefit.
- Paracetamol can be bought over-the-counter but paracetamol and codeine needs to be prescribed by a healthcare provider.
- Read more about paracetamol and paracetamol and codeine.
Non-steroidal anti-inflammatories (also called NSAIDs)
NSAIDs are used to reduce mild-to-moderate pain and inflammation (swelling).
- Some common ones are:
- Ibuprofen(external link) (Nurofen®, Advil®, Brufen®)
- Diclofenac(external link) (Voltaren®)
- Celecoxib(external link) (Celebrex®)
- Naproxen(external link) (Noflam®, Naprosyn®, Naprogesic®)
- Mefenamic acid (Ponstan®)
- Tenoxicam(external link) (Tilcotil®).
- They work by blocking and reducing enzymes involved in making a hormone-like substance called prostaglandin that causes pain and swelling in your body.
- NSAIDs can be used for short-term pain such as when you have an injury or a flare-up of symptoms (eg, a gout attack).
- They're often used together with paracetamol to improve pain relief.
- NSAIDs aren’t suitable if you’re pregnant or have asthma, heart, liver, kidney or stomach problems (because they may cause stomach bleeding). You may be prescribed another medicine while taking NSAIDs to protect your stomach, eg, omeprazole.
- Before taking NSAIDs, check with your healthcare provider whether they're suitable for you.
- NSAIDs are also available as gels or creams that can be bought over the counter for massaging into the painful area.
- Some NSAIDs, eg, ibuprofen and Ponstan can be bought over the counter but stronger ones need to be prescribed by a healthcare provider.
- Read more about NSAIDs and NSAID gels.
Opioids
Opioids can be used for moderate-to-severe short-term pain such as after an injury or surgery.
- Some common ones are codeine, tramadol, morphine, oxycodone.
- Codeine, dihydrocodeine and tramadol are weaker opioids for moderate pain, while morphine and oxycodone are used for more severe pain.
- For some people they can cause unpleasant side effects, such as constipation, nausea (feeling sick), dizziness and sleepiness. You may be prescribed other medicines for nausea and constipation to help with these side effects.
- Opioids reduce the pain but don’t take it away completely.
- Only use opioids at the lowest dose that helps with your pain and for the shortest time possible.
- If you think your pain is manageable, stop taking them. Ongoing use can lead to dependency and addiction.
- Opioids need to be prescribed by a healthcare provider.
Steroids
Some steroids, eg, prednisone are used for pain relief by reducing swelling and inflammation when other pain relievers are not effective alone or are not suitable.
- They may provide short-term pain relief, but don't improve joint function or stiffness.
- They are most useful for treating flare-ups of pain, eg, with gout or asthma.
- Steroids need to be prescribed by a healthcare provider.
Muscle Relaxants
- Orphenadrine is also called Norflex®. It can provide pain relief for pain related to muscle spasms.
- Hyoscine is also called Buscopan® or Gastrosoothe®. It can provide pain relief related to stomach muscle spasms.
- These muscle relaxants shouldn’t be used on an ongoing basis due to their side effects.
Medical conditions
Some pain medicines can worsen some medical conditions and should be avoided. For example, NSAIDS can make stomach ulcers worse, so if you have a history of stomach ulcers, you should avoid them. NSAIDs must also be used with caution by older adults and people with heart disease, type 2 diabetes or kidney problems.
Medicines you are taking
Before taking medicine for pain relief, it’s important to ask if they might interact with medicines that you’re already taking for another condition, eg, codeine and gabapentin shouldn’t be taken together. If you’re unsure, check with your doctor or pharmacist.
Allergies
Some allergies may prevent you from taking certain types of pain relief medicines. For example, NSAIDs can cause allergic reactions in some people. Soon after taking the medicine, you may develop flushing, itchy rashes (hives), blocked and runny nose, and asthma (sometimes severe). If you have had hives (urticaria), nasal polyps or asthma, your risk of NSAID allergy is much higher than it is for people without these conditions.
All medicines have side effects and risks. Sometimes the risks may be small and the benefit to your health may outweigh the risks, while in other cases the risks may be a problem and other medicines may be safer. The best choice depends on your situation and the advice of your healthcare provider. Below is a list of the benefits and risks of different pain relief medicines.
Paracetamol
| Benefits and risks |
Benefits
|
Non-steroidal anti-inflammatory drugs (NSAIDs)
Such as ibuprofen, diclofenac, naproxen and celecoxib.
| Benefits and risks |
Benefits
|
Opioids
Such as morphine, codeine, tramadol and oxycodone.
| Benefits and risks |
Benefits
|
Steroids
Such as prednisone tablets.
| Benefits and risks |
Benefits
|
The following links provide further information on short-term pain relief medicines. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
Resources
Managing pain poster(external link) Waitematā DHB, NZ
Allergic reactions to aspirin and other pain killers(external link) Australasian society of clinical immunology and allergy
Opioid medicines for short-term pain [PNG, 145 KB] Healthify He Puna Waiora, NZ, 2023 English [PNG, 145 KB], te reo Māori [PDF, 126 KB]
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ English(external link), te reo Māori(external link)
References
- The principles of managing acute pain in primary care(external link) BPAC, NZ, 2018
- Acute low back pain(external link) BPAC, NZ, 2022
Brochures

Managing pain poster Waitematā DHB
Waitematā DHB, NZ, 2016
Opioid medicines for short-term pain
Healthify He Puna Waiora, NZ, 2023 English, te reo Māori

Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Stephanie Yee, Pharmacist, Auckland
Last reviewed:





