You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Bladder control problems
Key points about bladder control problems
- Over 600,000 adult New Zealanders, both men and women, don't have full bladder control, but with the right advice and treatment the majority of those affected can have significant improvement.
- About 1 in 3 women who have had a child and 1 in 10 men will have some form of bladder control problem.
- For women, problems are associated with pregnancy, childbirth, menopause and ageing.
- For men, problems are most commonly related to ageing.

The production of urine is not under our voluntary control. However, as adults, we are able to recognise when our bladder is full, and can hold urine in until we reach a toilet. This means we have control over when and where we will pass urine (pee).
This control is possible because of messages passing between the brain and the bladder, and our ability to interpret these messages. We can learn to use this mechanism to delay passing urine.
The bladder and the urethra
Two structures that help keep urine in your bladder are the pelvic floor muscles and the urethral sphincter.
The pelvic floor muscles help hold all of the pelvic organs in place. When the pelvic floor muscles are strong, the urethra and bladder can't move out of place. This helps keep the urethra closed, so urine can't leak from your bladder.
The urethral sphincter is a band of muscles around the urethra. When these muscles are strong, they squeeze tightly and keep urine in your bladder. When you want to urinate you can relax these muscles.
The image below shows the male and female pelvic anatomy related to bladder control.
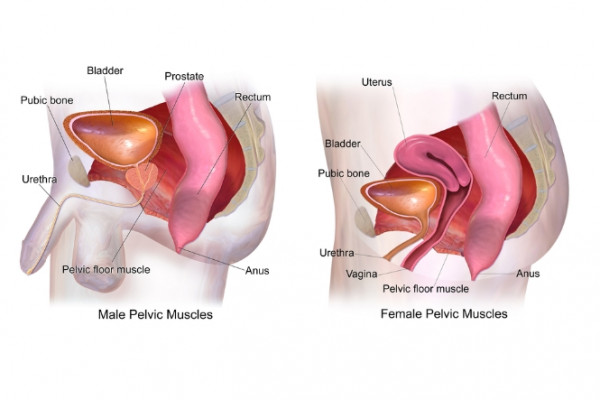
Image credit: Bruce Blaus(external link) via Wikimedia Commons
- Stress incontinence – this is urine leakage during physical exertions that raise abdominal pressure (eg, coughing, sneezing, exercising or lifting). If you have weak pelvic floor and urethral muscles this can force urine out of your urethra.
- Urge incontinence – also known as overactive bladder. This produces a sudden, strong urge to urinate if bladder emptying is delayed, and results in uncontrolled leakage. This is often due to involuntary (out of your control) bladder overactivity.
- Overflow incontinence – this occurs when your bladder can't empty properly. This causes it to become too full, overflow and then leak regularly in small amounts, with no real trigger or warning.
Some people can have a combination of these different types of incontinence.
Some symptoms need urgent treatment as they could be due to an infection, prostate cancer or kidney failure.
Call Healthline (0800 611 116) or see your healthcare provider urgently if you have any of the following symptoms:
- You can't pass urine at all.
- Burning discomfort or pain while passing urine (pee/mimi).
- Blood in your urine.
- Pain or discomfort in your lower abdomen (belly).
- Any other change in your normal urine pattern that lasts more than 1 to 2 days.
Things that can contribute to bladder control problems include:
- pregnancy and childbirth
- constipation
- some medicines, eg, diuretics and antipsychotic medicines
- chronic cough
- urinary infection
- diseases that affect your nervous system and muscular control
- diabetes
- body size and health
- reduction in hormones after menopause (when your period stops).
- Urgency – the feeling of needing to pee right now.
- Incontinence – leakage of pee.
- Frequency – peeing more often than usual.
Ageing
As you get older, your body changes. The muscles in your bladder change and can become weaker so your bladder may not be able to hold pee in. Your prostate gets bigger which can sometimes affect the flow of urine from your bladder. Also, with older age, the body tends to store fluid during the day and get rid of it at night while you're lying flat. This results in extra urine production at night.
Your prostate gland
The prostate is a small gland found in men. It's about the size of a walnut and sits just below your bladder. Its job is to secrete a milky fluid that becomes part of the semen and nourishes the sperm. Because the prostate gland is located close to the bladder, it can affect the flow of urine from your bladder. This causes a condition called benign prostatic hyperplasia (BPH), also called prostate enlargement. The prostate often gets blamed for many bladder problems but it’s not always at fault.
Other causes of prostate-related urinary conditions include prostatitis, infection or prostate cancer. Read more about common prostate conditions.
If you have a prostate problem you may have one or more of these symptoms:
- Difficulty starting the flow of urine.
- A slow urine stream once urination has started.
- The need to urinate (pee) more often than usual during the day (frequency).
- Having to wake during the night to pee multiple times (nocturia).
- Dribbling after urinating, or between visits to the toilet.
- Feeling the urgent need to pee (urgency).
- A sensation that emptying isn't complete.
- Having to urinate again within a short time of having just urinated.
How can prostate conditions lead to incontinence?
Partial blockage of the urethra by the prostate
- As the urethra narrows, the bladder has to contract more forcefully to push urine out through the urethra.
- Over time, the increased effort required to empty your bladder makes your bladder muscles grow stronger and more sensitive. Your bladder begins to contract even when it contains only a small amount of urine, creating the need to urinate more frequently and urgently. Sometimes urine leaks before you have time to get to the toilet (urge incontinence).
- The narrowed urethra may also prevent your bladder from emptying completely when you urinate. This can cause a build up of urine and lead to leakage between trips to the toilet (overflow incontinence) – it requires medical attention.
Nerve and muscle damage
- Surgery for prostate problems can sometimes damage the muscles and nerves of the sphincter (the muscle that helps hold urine in your bladder) resulting in short- or long-term incontinence.
- The potential for damage depends on the extent of the surgery.
Other causes of incontinence
- Medical conditions, eg, urinary tract or bladder infection.(external link)
- Surgery, eg, spinal surgery or prostate surgery.
- A bladder tumour or stone.
- Medicines, eg, diuretics (water tablets).(external link)
- High intake of alcohol and caffeine.
- Smoking.
Most symptoms of bladder control problems are due to the flow or storage of urine. Some men get a mixture of symptoms. Most symptoms are usually not serious but sometimes they can be due to a serious condition, eg, prostate cancer.
It’s important to see a healthcare provider if you have any of the following symptoms – even if they're mild:
- Struggling to start peeing (called hesitancy).
- Producing a slow stream of pee.
- Taking a long time to pee.
- Wetting the bed.
- Peeing more often than usual (urinary frequency).
- After-discharge of pee.
- A feeling of incomplete bladder emptying.
- Having a sudden urge to pee (urinary urgency).
- Leakage of pee before getting to the toilet (urinary incontinence or overactive bladder).
- Leakage from coughing, sneezing, laugh or exercising (stress incontinence).
Your healthcare provider will ask about your symptoms. They'll take your blood pressure, examine you and will probably ask you to collect a urine sample.
They may ask you to keep a bladder diary, recording how often you pee, and how much urine you pass.
Tips for improving your bladder control
- Try to ‘be the boss’ of your bladder, not the other way around. Adults usually pass urine 4 to 6 times in a day and maybe once during the night. Bladder retraining techniques can help people with urge incontinence to lengthen the time between toilet visits and ‘buy more time’ when the urge strikes.
- Assess how how much fluid (eg, water, juice, coffee, tea, fizzy drinks) you drink in total each day. Usually 5 or 6 drinks a day in total is enough. There's no ‘right amount’ to drink – frequently people think they should drink a lot more than they need. Reduce drinking in the evening if going to the toilet at night is a problem.
- As your bladder and bowel are next to each other, a full bowel affects bladder function. Eat a diet with plenty of fibre to help avoid constipation (and consequent straining during bowel motions).
- Avoid bladder irritants (eg, alcohol and caffeine-containing beverages) if they irritate your bladder.
- Check all of your medicines with your doctor or nurse prescriber – some can affect bladder control.
- Keep to a healthy body weight – it puts less strain on your pelvic floor muscles.
- If you smoke, get support to quit smoking. Research suggests that smokers are more likely to experience urinary incontinence and urinary stress. This is due to the excessive strain that repeated coughing puts on your pelvic floor.
- Do exercises to strengthen your pelvic floor muscles.
- For men: If you have find there's a bit more urine trickling out after you've finished peeing, try shaking the end of your penis. Try sitting to pee or peeing twice.
Daily pelvic floor muscle exercises
Men and women can strengthen their pelvic floor muscles. Over weeks or months this can improve bladder control. To activate these muscles, while sitting, tighten the muscles of the bladder outlet (urethra) and anus (not buttocks) as if trying not to pass wind, ‘lift up’ inside and hold. Contract these muscles strongly while sitting, lying or standing (don't strain by bearing down), hold for 5 to 10 seconds (keep breathing), rest, then repeat several times – perform this a few times a day.
If you're still unsure which muscles to use, try to stop or slow your urine midstream; this engages the right muscles, but don't make this a regular exercise. Try to get into the habit of tightening your pelvic floor muscles immediately prior to any activity such as lifting, leaning forward or laughing.
Read more about pelvic floor training for men and women. The best results will come from meeting with a pelvic health physiotherapist or continence advisor as sometimes muscles need to be relaxed rather than strengthened. Find a continence service provider.(external link)
Bladder training
The aim of bladder training is to improve bladder control and increase the amount or urine your bladder can comfortably hold – without urgency or leakage. Learn more about bladder training.
Incontinence pads
Try using pads inside your underwear to soak up any leaks. You can find these in the supermarket or pharmacy.
Apps reviewed by Healthify
You may find it useful to look at some Pelvic floor exercise apps and Quit smoking apps.
Incontinence can usually be stopped or improved by treatments including pelvic floor muscle exercises, bladder training, medicines and surgery. Exercising and eating/drinking to prevent constipation are also important.
How the problem affects you depends on what's causing it. So, it's important to get help from your healthcare provider or continence adviser to find out what's causing it and what can be done to treat it.
Treatment for women
Medicines
If you have ongoing problems with urinary incontinence, even after trying the self-care tips described above, your healthcare provider may prescribe medicine.
Bladder problems that develop around the time of menopause may improve with oestrogen. This can be in the form of a vaginal cream or pessary or as menopausal hormone therapy.
Anticholinergic medicines such as oxybutynin or solifenacin, act on your bladder muscles to help improve bladder control.
Surgical treatment options
If non-surgical treatment options haven't worked, a surgical option may be considered. Think about what you would like to ask your surgeon before you see them. Finding a credentialed surgeon with experience in these procedures is essential.
Not everyone will undergo the same procedure. Your doctor or surgeon may recommend a specific procedure for clinical reasons. Talk to your doctor or surgeon about which procedure is most suitable for you. They will consider all relevant issues, including your previous surgical history and your wishes.
Surgical treatment can be further divided into procedures that use surgical mesh(external link) and those that don't. The procedures described below are those not involving mesh that are currently recommended by Health New Zealand | Te Whatu Ora.
- Colposuspension: An operation that's carried out through open or keyhole surgery through your abdomen (belly). Permanent synthetic sutures (stitches) are used to lift your vagina and support your urethra (the pipe through which your bladder empties).
- Natural or biological tissue sling: Open surgery through your abdomen to lift your urethra using a sling from your own abdominal wall. Type of slings that are used include:
- natural sling, eg, fascia
- biological sling, eg, biological material of animal origin.
- Urethral bulking agents: A vaginal operation where a synthetic ‘bulking’ material is injected in or around your urethra to improve the seal. This material may be permanent or absorbed by your body.
Procedures involving surgical mesh implants: The term ‘surgical mesh’ refers to a permanent synthetic implant that's made from a non-absorbable polypropylene (plastic) material. It's known by multiple names including tape, sling, TVT, patch, ribbon, graft or hammock. From August 2023 all surgical mesh procedures have been paused while steps are taken to minimise harm.
Treatment for men
Read about treatment of bladder problems caused by prostate enlargement in men.
Continence NZ was established to provide a service to people with continence problems, caregivers, health professionals and the general public by providing information and education on continence topics.
Continence helpline 0800 650 659 for friendly advice
Continence service providers for adults and children(external link) Continence NZ
Continence information – adults(external link) NZ Continence Association
Promoting good bladder and bowel health(external link) NZ Continence Association
Can't wait card order form(external link) NZ Continence Association
Brochures
Stress urinary incontinence(external link)(external link) RANZCOG, Australia
Promoting and managing continence for people living with dementia mate wareware(external link) University of Auckland, NZ, 2024
Apps
References
- Considering surgical mesh to treat urinary stress incontinence(external link) Ministry of Health, NZ, 2019
- Continence information – adults(external link) Continence NZ
Urinary incontinence – te mimi wewete(external link) HQSC, NZ, 2019
Continence screening form for residential care(external link) Deakin University, Continence NZ
Continence assessment and care plan(external link) Continence NZ
See our page Men's health for healthcare professionals
Apps
Brochures

Stress urinary incontinence
RANZCOG Australia and NZ, 2022

Promoting and managing continence for people with dementia mate wareware
University of Auckland, NZ, 2024

Can't wait card
Order a card Continence NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed:
Page last updated:





