You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Nerve pain
Also called neuropathic pain
Key points about nerve pain
- Nerve pain happens when damage or changes to your nerves through disease or injury causes them to send pain signals to your brain.
- It can happen anywhere in your body, but nerve pain in your legs and feet is very common.
- Nerve pain can be very unpleasant and may impact on your daily activities and sleep.

Nerve pain is the unpleasant feeling you experience when disease or injury damages your nerves. This could be in your:
- central nervous system (CNS) – your spinal cord or your brain, or
- peripheral nervous system (PNS) – the nerves in your arms, legs and organs.
The image below labels your central nervous system and some of the nerves in your peripheral nervous system.
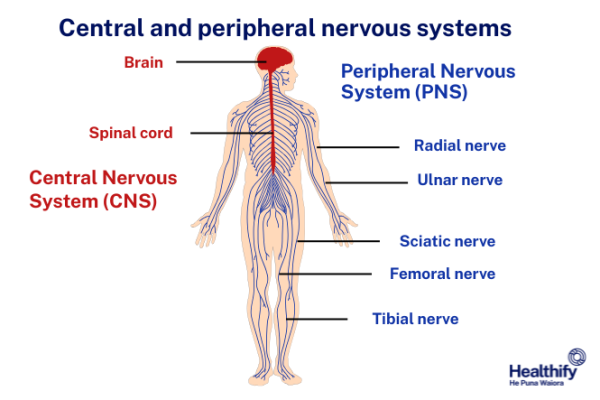
Image credit: Healthify He Puna Waiora
Nerve pain is most common in your legs and feet because these are the ends of the longest nerves in your body.
Nerve pain happens because of damage or changes to your nerves. Common causes of nerve pain include:
- diabetes
- multiple sclerosis
- stroke
- Parkinson's disease
- brain injury
- trigeminal neuralgia – a type of nerve pain in your face
- sciatica – a type of nerve pain in your leg coming from your back
- surgery or amputation
- vitamin B12 deficiency
- excess alcohol consumption
- cancer pressing on a nerve
- chemotherapy
- carpal tunn
- shingles – a rash caused by a virus infecting your nerve
- spinal cord injury
- peripheral nerve injury, such as carpal tunnel syndrome – a type of nerve pain in your hands
- complex regional pain syndrome after an injury.
Sometimes nerve pain can happen without any obvious cause.
Nerve pain can be described as:
- burning
- sharp
- shooting
- stabbing
- pricking
- electric sensations
- pins and needles
- feeling pain from something that shouldn't be painful, such as very light touching, brushing your skin or cold temperatures.
The pain may be constant and ongoing, or it may come and go (intermittent). It can be mild, moderate or severe. Your symptoms may vary depending on the time of day (it may be worse at night) or what you are doing at the time. Nerve pain may sometimes be accompanied by other symptoms such as:
- numbness
- weakness
- itching
- sweating
- muscle spasm.
Your healthcare provider will ask you questions about how your pain started and what it feels like, and they will examine you. Nerve pain can usually be diagnosed by its symptoms. Then your healthcare provider will try to find out the cause. This is what will decide whether you need further tests such as a blood test.
There are many ways to manage nerve pain. The first step is to see your healthcare provider and treat the underlying cause if there is one. For example, better control of diabetes can also help to improve pain from diabetic neuropathy.
The main aim of treatment is to keep you active and doing your daily activities. Treatment may include a combination of medicine and non-medicine options.
Non-medicine approaches
- Have a plan for how to manage your daily activities. If you have long-term pain you probably get tired quickly and planning your activities can give you a greater sense of control over your condition. You may want to get the important tasks done early in the day or when you have the most energy.
- Try to get enough sleep. Poor sleep can make pain worse, but pain can disrupt your sleep. Talk to your healthcare provider if you're having problems sleeping.
- Keep active. Keeping active is very important – simply being inactive can make pain worse. A physiotherapist can help you with suitable exercises and advise you on how to become more active without aggravating your pain.
- Learn about mindfulness. Mindfulness reduces stress, tension and anxiety. It can help you to avoid focusing too much on your pain as well as directing your thoughts in a way that is helpful to manage your pain.
- Seek support. Sharing your experience with trusted whānau, friends and peer support groups are all good ways to help you manage your pain.
- Acupuncture or transcutaneous electrical nerve stimulation (TENS) may be useful but evidence is lacking.
- Psychological approaches, such as cognitive-behavioural therapy (CBT), may help some people to adapt to living with pain. However, there is little evidence to suggest it reduces the neuropathic pain itself.
Read more about non-medication approaches to managing pain.
Regular pain relief medicines don't usually work for nerve pain. These include paracetamol, NSAIDs such as ibuprofen and diclofenac and opioids such as codeine.
Other medicines have been found to be more effective in relieving nerve pain, including:
These medicines often need to be taken for a few weeks before they start to work properly. If your pain doesn't respond to one option, your healthcare provider may suggest changing it. You'll be started on a low dose which will gradually be increased until it starts to work for you. Higher doses may be more effective, but are also more likely to cause side effects. The most common side effects are tiredness, dizziness, feeling drowsy and lack of concentration. If you get these, it may be necessary to reduce your dose.
Another treatment option is capsaicin cream. A small amount of cream is rubbed on the painful area of skin 3 or 4 times a day. This is useful if your pain is in a particular area of your body, or if you can't take the medicines above. Capsaicin is the substance that makes chilli peppers hot and is thought to work for neuropathic pain by stopping the nerves sending pain messages to your brain. Read more about capsaicin cream.
Pain can affect you in many ways and can stop you doing the things you want to do. If you have ongoing, or chronic, pain it's normal to feel frustrated about the impact this has on you. The good news is there are different ways of managing chronic pain to improve your wellbeing.
Learn more about living with chronic pain.
Apps reviewed by Healthify
You may find it useful to look at some pain management apps.
Brochures
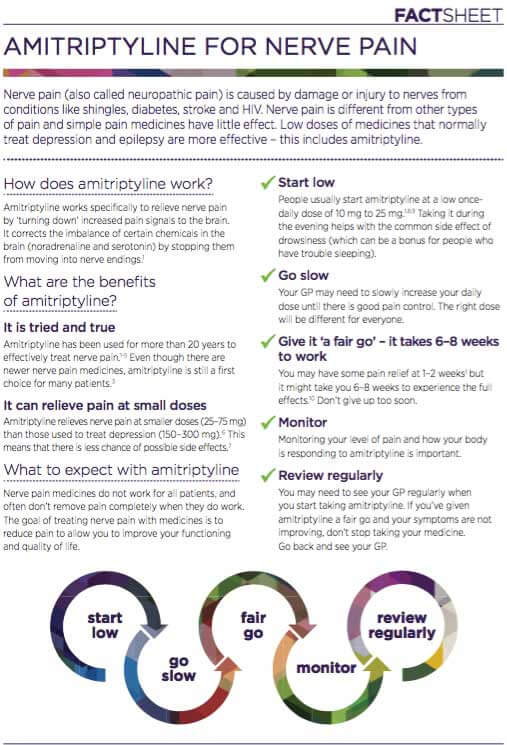
Amitriptyline for nerve pain [PDF, 150 KB] NPS MedicineWise, Australia, 2018
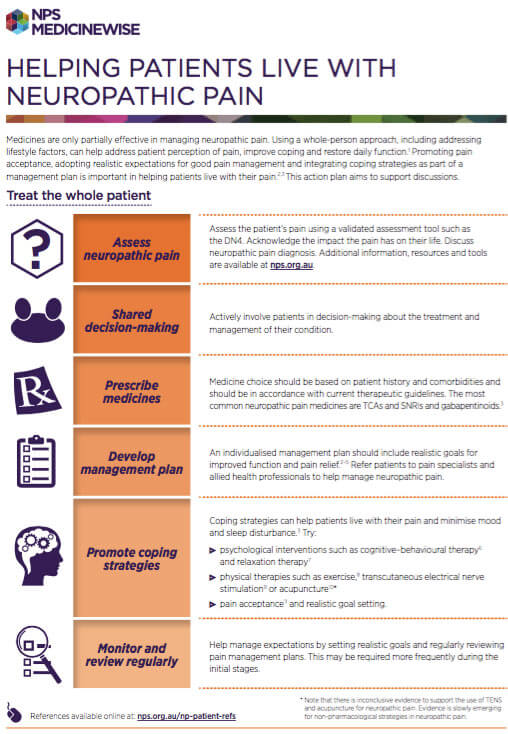
Helping patients with neuropathic pain NPS MedicineWise [PDF, 168 KB] NPS MedicineWise, Australia, 2018
Diabetes and how to care for your feet(external link) Diabetes New Zealand, 2023
Apps
References
- Managing patients with neuropathic pain(external link) BPAC, NZ, 2016
- Neuropathic pain in adults – pharmacological management in non-specialist settings(external link) NICE, UK, 2020
- Chronic non-cancer pain(external link) Auckland Community HealthPathways, NZ, 2025
- Gibson W, Wand BM, Meads C, et al. Transcutaneous electrical nerve stimulation (TENS) for chronic pain – an overview of Cochrane reviews(external link) Cochrane Database Syst Rev. 2019 Apr 3;4(4):CD011890
Leeds Assessment of Neuropathic Symptoms and Signs (LANSS)(external link) a diagnostic tool designed to distinguish neuropathic from non-neuropathic pain. A LANSS score of 12 or more has a sensitivity ranging from 82 to 91% and specificity ranging from 80 to 94% when compared with diagnosis in a pain clinic.
Managing patients with neuropathic pain(external link), BPAC, NZ, 2016
Brochures
NPS MedicineWise, Australia, 2018

Diabetes and how to care for your feet
Diabetes New Zealand, 2023
NPS MedicineWise, Australia, 2018
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed:





