You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
What is pain?
Key points about pain
- Pain is an uncomfortable feeling that tells you that something may be wrong somewhere in your body. It works to protect you from physical damage but ongoing pain is hard to live with.
- Acute pain is pain that starts suddenly and lasts for a short time. It’s usually due to tissue damage or inflammation, eg, from an injury or illness.
- Chronic or long-term pain lasts for months or years and it can be difficult to manage.
- Everyone experiences pain differently, so there are many ways to feel and describe it.
- Treatment for pain may include medicines or non-medicine treatments, depending on the type of pain you have, what has caused it and where it is.

Pain is an unpleasant feeling that tells you something may be wrong somewhere in your body.
When tissues in your body are damaged, nerves send messages along your spinal cord to your brain and you react by feeling pain. You can then do something about the pain and stop more tissue damage, such as when you pull your hand away from a hot surface and prevent burns to your skin.
The pain response works well for acute (short-term) pain, but sometimes it can go wrong. Pain messages can get confused in your brain. This can lead to chronic or persistent pain, which often has no useful purpose.
Pain is always a personal experience and is influenced by physical, mental and social factors. It’s helpful when it protects you from getting hurt, but it can also have negative effects on your day-to-day function and wellbeing.
Video: Pain explained by Central London Community Healthcare NHS Trust (6 minutes, 19 seconds)
(Central London Community Healthcare NHS Trust, UK, 2012)
We all experience pain in our own way because it’s an experience which comes from our brain and each of our brains is different. Your brain makes pain from a mixture of messages from your body (most but not all of the time), your thoughts and your emotions.
- Messages from your body come from tissue damage, which activates nerve endings called nociceptors.
- The messages travel in your peripheral nerves to a part of your spinal cord called the dorsal horn, where they pass to another nerve.
- The messages pass up your spinal nerves to your brainstem, the oldest part of your brain which is called white matter or ‘lizard brain’. Here there are many connections to other nerves from parts of your brain that process your emotions, your thoughts, your memories and your beliefs.
- All of these messages combine and reach your conscious mind, in a part of your grey matter called your somatosensory cortex. This is your experience of pain.
- Your brain then decides what to do. It might send messages back down your spinal cord to your muscles to move you away from danger. Messages can also go back down your spinal cord to quieten down the nociceptor messages coming up from your body.
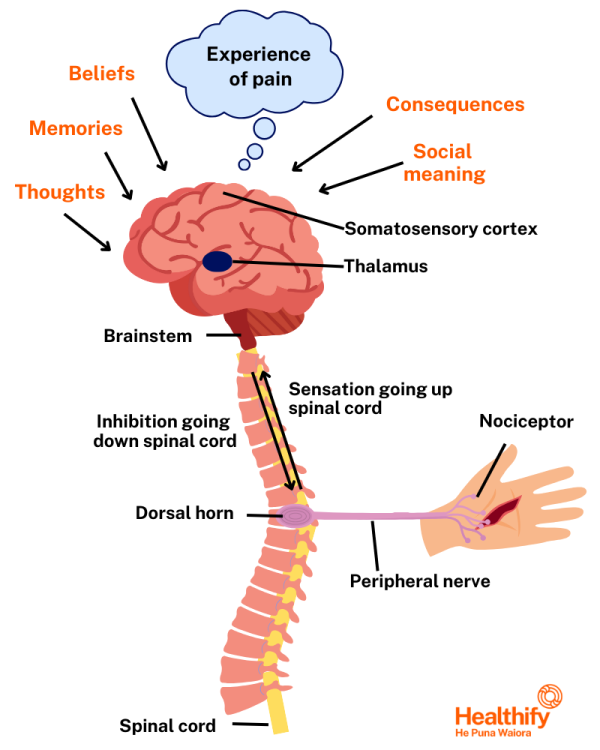
Image credit: Healthify He Puna Waiora
This is why if you feel angry, depressed or anxious, hungry or tired your pain can seem worse. If you’re feeling positive and happy, your pain can seem less intense, and you’re able to cope better.
The sensitivity of your nervous system also affects how you feel and respond to pain. People have different pain sensitivities because each person’s brain is different and that’s why some people experience more or less pain than others.
You learn about pain through our own life experiences and the community you live in. What you believe about pain affects how you experience it. If it reminds you of a severe pain you’ve had before or if you fear you won’t be able to work and you'll be useless to your family it may feel worse.
Pain is never 'all in your mind' or 'just in your body' – it’s a mix that involves your whole being and how your brain interprets the pain messages.
Video: How does your brain respond to pain? (4 minutes 57 seconds)
Things that can affect your experience of pain
Your body, mind and mood all play a part in how you experience pain. This means that your pain levels can be affected by things such as:
- the amount and quality of sleep you get
- activity/exercise levels
- stress levels
- your diet
- lifestyle choices
- medicines you’re taking
- your thoughts, moods, and emotions.
Addressing these things can help you and your healthcare provider manage your pain.
- how long it lasts – acute versus chronic pain
- location – where you can feel it, eg, back pain
- the mechanism – what’s happening in your pain system to start your pain or keep it going.
How long you've had your pain
Pain can start suddenly and last for a short time (this is called acute pain), or it can be ongoing and persistent, lasting for months or years (chronic pain).
Video: Acute vs chronic pain
Read more about acute pain and chronic pain.
Where your pain is
Pain can also be grouped according to its location, that is, where you're feeling the pain. For example you may be feeling pain in your muscles, joints, chest, or stomach.
Read more about the causes of pain in different parts of your body. Where you experience pain is a clue to what might be causing it.
Mechanisms of pain
Pain can be grouped according to what’s happening in your pain system.
- Nociceptive pain is pain that comes from actual or possible tissue damage in your body. It can be pain you feel in your skin, muscles, joints or bones. This is called somatic pain. It can be a deeper pain that comes from organs in your body, such as your heart or gut. This is called visceral pain. Nociceptors are pain receptors, nerve endings that sense possible tissue damage.
- Neuropathic (nerve ) pain happens when there is damage or changes to nerves in your body because of a disease or injury. It can be anywhere in your body, but nerve pain in your legs and feet is very common. Nerve pain can be very unpleasant and may impact your daily activities and sleep. Read more about nerve pain.
- Nociplastic pain is changed pain perception without tissue damage to your body. It can be pain felt after damage has healed, or pain felt without tissue damage. This type of pain comes from your spinal cord and brain (your central nervous system) not the pain receptors of your peripheral nervous system like nociceptive pain does. It’s also called central sensitisation. Chronic low back pain, , complex regional pain syndrome, and irritable bowel syndrome are examples of nociplastic pain. Noci means ‘pain’ and plastic means ‘can be shaped.’
You can have more than 1 type of pain. It’s common for nociplastic pain to start from nociceptive or neuropathic pain from an illness or injury.
- Cancer pain can be nociceptive pain. As the cancer grows or spreads, it can cause pain by pressing on surrounding tissues, such as your bones, or body organs. If it presses on your nerves or spinal cord it can cause neuropathic pain. If it affects your mood and thoughts it can cause nociplastic pain. Read more about cancer pain.
It can be difficult to find the exact cause of your pain.
The treatment for pain will depend on the type of pain you have and may involve medicines or a range of non-medicine treatments.
Describing your pain accurately can help your healthcare provider make the right diagnosis and develop the best treatment plan with you. It's fine to describe things in your own words – you don't need to use medical terms. Read more about describing your pain to find words you can use to describe your pain.
Treatment of acute pain
The sort of treatment that you’ll need will depend on the cause of your pain. For example, treatments for sprains and strains include pain relief medicines, R.I.C.E.R (Rest, Ice, Compression, Elevation, Referral) or a support such as a brace or a cast.
Medicines for acute pain usually work on your peripheral nerves or spinal cord. Read more about pain relief medicines for acute pain.
Treatment of chronic pain
Medicines alone aren’t an effective way to manage chronic pain because they work don’t work well for nociplastic pain. They can have harmful side effects when used for a long time. Instead, non-medication treatments are more effective. Read more about non-medicine approaches to managing pain.
Some types of chronic pain can be improved by medicines. They usually work on your spinal cord or brain. Read more about pain relief medicines for chronic pain.
Video: Understanding pain – what to do about it in less than five minutes (5 minutes)
(Painaustralia, Australia, 2012)
Brochures
Understanding and managing long-term pain(external link) The British Pain Society, UK, 2015
Knowing about managing your persistent pain(external link) ACC, NZ
The Pain Toolkit(external link) Pete Moore (UK) and Dr Frances Cole (NZ)
Tools/apps
Pain management apps
The Pain Toolkit(external link) Pete Moore, UK
References
- What is pain?(external link) British Pain Society, UK
- What is pain, and how do you treat it?(external link) Medical News Today, UK, 2020
- What is pain?(external link) Healthline, US, 2019
- Understanding and managing long-term pain(external link) The British Pain Society, UK, 2015
- Pain management(external link) WebMD
- What is pain?(external link) Pain Australia
- What is pain?(external link) Reach For The Facts, Australia
- Yam MF, Loh YC, Tan CS, et al. General pathways of pain sensation and the major neurotransmitters involved in pain regulation(external link) Int J Mol Sci. 2018;19(8):2164
- Andrews N. What's in a name for chronic pain?(external link) International Association for the Study of Pain, 2018
See our page Pain (chronic) for healthcare providers
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed:





