You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Multiple sclerosis | Wharanga uwhi iaia
Commonly called MS
Key points about multiple sclerosis
- Multiple sclerosis (MS or wharanga uwhi iaia) is a condition that affects the nerves of your brain and spinal cord.
- Symptoms vary depending on which areas of your brain and spinal cord are affected, so it’s difficult to know how MS will progress in each person.
- About 1 in 1000 New Zealanders has MS and some people are at greater risk of developing it than others.
- There's no cure for MS, but treatment aims to prevent relapses, ease symptoms and minimise disability.
- Maintaining a healthy lifestyle will give you the best chance of living well.

Multiple sclerosis (MS) is a condition that damages the nerves that connect your brain and spinal cord to the rest of your body.
In MS, your immune system attacks the protective layer around your nerve fibres. This causes scarring of your nerve fibres, so your nerves can’t send normal electrical signals throughout your body anymore.
The effects of MS depend on where the scarring is. Common symptoms are weakness, problems with your vision, and sensation problems such as numbness and electrical shocks.
MS can be diagnosed at any age, but first symptoms typically occur between 20 to 50 years of age and it's more common in women than men.
There are different types of MS depending on whether you have relapses (acute attacks), with or without periods with no symptoms (remission), and how your disease progresses.
Video: What is MS?
The exact cause of multiple sclerosis (MS) isn’t known. It’s thought to be an autoimmune condition which means your body's immune system attacks itself, without any known cause or reason.
In people with MS, something triggers the destruction of myelin, which is a fatty substance that coats and protects nerve fibres in your brain and spinal cord. The damaged myelin forms scar tissue (sclerosis). Often the nerve fibre is also damaged.
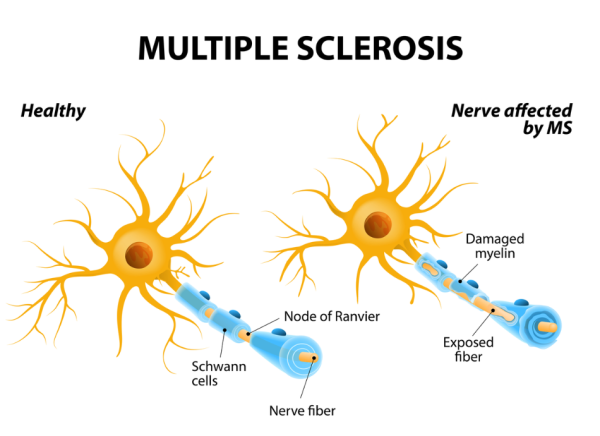
Image credit: Depositphotos
Normally, your nerve fibres transmit electrical signals throughout your body, enabling you to control your movements and functions as desired. However, when the myelin coating or the nerve fibres are damaged, these signals can no longer travel properly between your brain and spinal cord. This disruption leads to a decline and impairment in various bodily functions.
In Aotearoa New Zealand, about 1 in every 1,000 people has multiple sclerosis. It’s more common in certain groups:
- Young adults: MS can affect anyone at any age, but most people with MS have their first symptoms and are diagnosed between the ages of 20 and 40 years (usually around the age of 30).
- Women: MS is approximately 3 times more common in women than men.
- Ethnicity: MS is more common in Caucasians (people with ancestry from Northern Europe) than any other racial group. It’s less common in Māori, Pacific and Asian people.
- Close relatives: MS is not strictly a hereditary condition, but if you have a close relative with MS, you have an increased chance of developing it. Having a mother, father or sibling with MS increases the chances of developing it to 30 in every 1,000.
- Smokers: Smoking is associated with an increased risk of MS, and people who smoke appear to be at greater risk for relapse and progression of MS.
The symptoms of multiple sclerosis are unpredictable and vary from person to person. The symptoms can also vary in the same person from time to time as different areas of the brain and spinal cord become affected.
Common early symptoms
MS typically begins with an episode of neurological (nervous system) symptoms. You can experience more than 1 symptom but not necessarily all of them. Symptoms that can occur in MS include:
- problems with vision, such as blurred or double vision
- pain in one eye that’s worse when you move your eye
- muscle spasms
- muscle or nerve pain such as tingling, stabbing or burning pains over parts of your skin
- weakness or lack of coordination of your limbs
- extreme tiredness or fatigue that can affect balance and concentration.
Your symptoms may last several days or weeks and then improve.
Your symptoms may get worse due to:
- increased body temperature from fever, exercise, hot baths, sun exposure
- infection
- trauma
- new medicines
- other medical conditions, such as hyperglycaemia
- stress
- fatigue.
Later common symptoms
Other common symptoms that progress over time include:
- bladder and bowel problems such as urinary retention (when your bladder doesn’t empty completely) and constipation
- problems with sexual performance
- speech and swallowing problems
- mood swings and depression
- thinking, concentration and memory problems.
Read about managing your MS symptoms(external link) for advice on when to see your healthcare provider.
Clinically Isolated Syndrome (CIS)
If you have a single episode of the neurological symptoms that are typically seen in people with MS, it’s hard to predict what will happen in the future. This is known as clinically isolated syndrome (CIS). If you have CIS, you may not have any further episodes or you may go on to develop one of the other types of MS.
Relapsing-remitting MS
This is seen in about 85% of people with early-stage multiple sclerosis. It involves recurrent acute episodes (relapses), when symptoms suddenly increase, or new symptoms develop. This is followed by periods in which symptoms improve or even disappear altogether – these are called remissions.
Secondary progressive MS
This develops within 15 years of diagnosis in 2 out of 3 people who have relapsing-remitting MS. There is a gradual worsening of symptoms with or without acute relapses.
Primary progressive MS
This occurs in 1 out of 10 people with MS. Symptoms increase steadily from the beginning, usually with slowly increasing lower limb weakness.
Progressive Relapsing MS (PRMS)
This is the least common type, affecting only 5% of people with MS. With PRMS there is clear progression of your MS but you also have acute attacks with or without full recovery.
Multiple sclerosis can be difficult to diagnose because symptoms can come and go. Also, other brain and spinal cord conditions cause some of the same symptoms. A complete neurological exam and history of symptoms are needed to diagnose MS.
If your healthcare provider thinks you may have MS, they will refer you to a neurologist (a specialist doctor who treats conditions of the brain and nervous system). The neurologist will arrange for tests and then start treatment if they find that you do have MS.
There is no single test for MS, but the following tests help to confirm, or rule out, the diagnosis:
- Blood tests can rule out other conditions with similar symptoms.
- MRI (magnetic resonance imaging) of your brain and spinal cord can show areas that indicate that the protective covering of certain nerve fibres has been damaged.
- A lumbar puncture(external link) involves removing a small amount of the fluid that surrounds your brain and spinal cord. The fluid is analysed to see if there are changes in certain protein levels.
- Evoked potential (EP) tests are used to identify any slowing, or other abnormal pattern, in the electrical signals of certain nerves.
Currently, there’s no cure for multiple sclerosis, but there are medicines that can slow down the progression and help to ease symptoms when you have them.
Preventing relapses (disease-modifying therapies)
Disease modifying therapies (DMTs) can reduce the number and severity of relapses in some people with MS. They can slow down how fast your MS gets worse. DMTs only work if there’s active inflammation in your brain or spinal cord. By changing how your immune system behaves, DMTs can make it less likely to attack the nerves in your brain and spinal cord, so there’s less inflammation and less new damage to your nerves. However, DMTs can’t repair nerves that have been permanently damaged.
The following are examples of DMTs that are available in Aotearoa New Zealand. These medicines are currently funded by Pharmac:
- Fingolimod capsules (Gilenya®)
- Teriflunomide tablets (Aubagio®)
- Dimethyl fumarate capsules (Tecfidera®)
- Natalizumab injection (Tysabri®)
- Glatiramer acetate injection (Copaxone®).
- Ocrelizumab injection (Ocrevus®).
- Beta interferon injections (Avonex®, Betaferon®).
These DMTs are used to treat relapsing-remitting MS. Ocrelizumab is the only DMT that’s also funded for the treatment of primary progressive MS.
If you have relapsing MS, it’s best to start DMTs early. The sooner you start a DMT, the less your brain and body are likely to suffer damage. Damage caused by MS builds up over time and can happen between relapses. DMTs can reduce the risk of developing MS if you have clinically isolated syndrome (CIS).
Only a neurologist (a specialist doctor who treats brain and nervous system conditions) can start you on a DMT. They will consider factors such as how active your MS is, how many relapses you’ve had in the last year or two, how bad they were and if you’ve tried another DMT that didn’t work for you.
Treating relapses
A steroid medicine, such as methylprednisolone, may be used to treat acute flare-ups. This can be taken either orally (by mouth) or intravenously (into a vein) and is usually given as a high dose for a few days. Steroids can shorten the length of an attack, however they don't change the outcome. Steroids are usually only used for severe and disabling relapses. Steroids work by reducing inflammation.
Easing symptoms
With MS you may experience a variety of symptoms, and these are treated as they appear. Treatment will depend on how severe the symptoms are. Examples are:
- anti-spasm medicines to ease any muscle spasms
- painkillers, eg, for nerve pain.
- medicines to help with bowel and bladder problems
- antidepressant medicines which are sometimes advised if you develop depression
- medicines which can help with erectile problems.
Rehabilitation
Rehabilitation aims to improve function that you’ve lost, usually after an acute attack of MS.
During remission periods, it's best to take part in a maintenance programme to achieve and maintain your best physical condition. This may involve:
- physiotherapy
- stretching
- coordination exercises
- speech and swallowing instruction.
It may also include medication, good nutrition and counselling, and you may also need to make some lifestyle changes.
Maintaining a healthy lifestyle will help your body cope with MS and give you the best chance of living well.
- Keep active but rest when you need to. There’s good evidence that regular exercise improves overall health and energy levels.
- Eat a balanced diet to stay healthy and keep your energy levels up. There’s no evidence that any particular diet changes the course of MS.
- If you smoke, stop smoking as it can make your MS worse.
- Keep your mind active by doing activities such as puzzles, reading or playing cards.
- Keep working if you can, as this can help your physical and mental well-being.
- Talk to your healthcare provider about getting vaccinated against influenza and COVID-19. Viral infections can cause temporary worsening of MS symptoms, so doing your best to reduce your risk of infections is a good idea. Also some disease modifying therapies (DMTs) can increase the risk of having a more severe infection so seasonal flu and COVID-19 vaccinations are recommended.
- Have a management plan that includes who you should contact if your symptoms get worse.
See also these tips for managing MS(external link)
Apps reviewed by Healthify
You may find it useful to look at some Self-management and healthy living apps and Nutrition and exercise apps.
Most people with multiple sclerosis (MS) have a normal or near-normal lifespan, but MS symptoms can impact your quality of life.
Because MS affects people in different ways, it’s difficult to predict the outlook for each person. There are currently no tests to predict how MS will progress in a particular person.
- Most people with MS will be able to continue to walk and function at work for many years after their diagnosis.
- About 1 in every 5 people with MS have no symptoms or develop only mild symptoms after an initial event.
- Another 1 in every 5 people experience a rapid progression of symptoms.
- Research has shown that 20 years after diagnosis, about two-thirds of people with MS continue to walk and do not need a wheelchair, although many of them may use a cane or crutches for walking assistance. Some people use an electric scooter or wheelchair to help cope with fatigue or balance problems.
If you’re a woman with MS, you may be considering starting a family or having another child. Pregnancy doesn’t have a major effect on your MS, but you need to talk to your neurologist before getting pregnant if you’re taking DMTs. You’re less likely to have a relapse while you’re pregnant, but there’s an increased risk of relapse in the 3 to 6 months after your pregnancy. There’s a small increased risk that your child will develop MS. Talk to your healthcare provider if you’re considering becoming pregnant.
It can be difficult to adjust to a diagnosis of MS, partly because of its unpredictable nature. Talk to your whānau, friends and healthcare provider about how you're feeling. You can also get support from a counsellor or therapist(external link)
Multiple Sclerosis New Zealand(external link) has lots of information for people with MS, their whānau and carers. They can put you in touch with a community support staff member who can provide one-on-one support and information. The range of services offered varies between regional MS societies.
Video: Multiple sclerosis awareness – life with MS
(Multiple Sclerosis Society, NZ, 2016)
Video: 'MS does not define who I am' – MS Awareness Video
(Multiple Sclerosis Society, NZ, 2016)
Video: Overcoming MS – Dr White's personal journey towards better health with MS | Episode 8 of 15
(Multiple Sclerosis Society, NZ, 2020)
Watch more videos from Multiple Sclerosis New Zealand(external link).
The following links provide further information on multiple sclerosis. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
Multiple Sclerosis New Zealand(external link) has a comprehensive resource page(external link) which includes information for people with MS, parents of children with MS, children and teenagers who have a parent with MS, students and teachers, carers and employers.
Multiple sclerosis(external link) NHS, UK
Multiple sclerosis(external link) Patient Info, UK
MS and pregnancy(external link) Multiple Sclerosis Auckland, NZ (includes slides from a webinar held in May 2022)
Brochures
What is multiple sclerosis?(external link) Multiple Sclerosis New Zealand
Living well with MS – a resource for anyone impacted by MS(external link) Multiple Sclerosis New Zealand
Preparing for your neurologist appointment(external link) Multiple Sclerosis New Zealand
Courses
Multiple sclerosis(external link) Free online courses about understanding MS, deciding about DMTs, and mental health and MS. Menzies Institute for Technical Research, University of Tasmania, Australia
Apps
Self-management and healthy living apps
Nutrition and exercise apps
References
- About multiple sclerosis(external link) Multiple Sclerosis Society, NZ
- Multiple sclerosis (MS)(external link) Auckland Community HealthPathways, NZ, updated 2022
- Multiple sclerosis(external link) Health New Zealand | Te Whatu Ora, NZ
- Multiple sclerosis in adults – management(external link) NICE Guideline, UK, 2022
- Decision to fund treatment earlier for relapsing remitting multiple sclerosis(external link) Pharmac, NZ, 2022
- Pharmac funds first treatment for primary progressive multiple sclerosis(external link) Pharmac, NZ, 2023
- Clinically isolated syndrome (CIS)(external link) Multiple Sclerosis News Today, US, 2022
- MS and pregnancy(external link) Multiple Sclerosis Auckland, NZ
Resources
Multiple sclerosis in adults – management(external link) NICE Guideline, UK, 2022
GP guide for MS relapse management(external link) Auckland District Health Board, NZ
Brain health in multiple sclerosis – a nursing resource(external link) MS Brain Health, 2017
Leadbetter R, MacAskill M, Myall DL,et al. Multiple sclerosis mortality in New Zealand – a nationwide prospective study(external link) J Neurol Neurosurg Psychiatry. 2023;94(7):511-517.
Decision to fund treatment earlier for relapsing remitting multiple sclerosis(external link) Pharmac, NZ, 2022
Pharmac funds first treatment for primary progressive multiple sclerosis(external link) Pharmac, NZ, 2023
Updated McDonald Criteria expected to speed the diagnosis of MS and reduce misdiagnosis(external link) National Multiple Sclerosis Society, US, 2017
Living well with MS(external link) Multiple Sclerosis New Zealand, 2024
Continuing professional development
Video: MS and neuroimmunology, Dr Jennifer Taylor (36 minutes)
Video: Neurology update, 2 of 6. 60-second neurological exam, and case – multiple sclerosis
Online courses
Multiple sclerosis(external link) Free online courses on understanding MS, deciding about DMTs, and mental health and MS. Menzies Institute for Technical Research, University of Tasmania, Australia
Brochures
Living well with MS – a resource for anyone impacted by MS
Multiple Sclerosis New Zealand, 2024

What is multiple sclerosis?
Multiple Sclerosis New Zealand

Preparing for your neurologist appointment
Multiple Sclerosis New Zealand, 2023
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Multiple Sclerosis New Zealand
Last reviewed:





