If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Complex regional pain syndrome
Also known as CRPS
Key points about complex regional pain syndrome
- Complex regional pain syndrome (CRPS) is a medical condition that usually affects an arm or leg. It presents with severe pain and other symptoms, which may become chronic.
- It’s not common, but can happen after an injury or trauma.
- Pain is the main symptom but others can include changes related to sensation, temperature, sweating, swelling, movement, and hair/nails/skin.
- There’s no cure, but recovery outcomes are better if you start treatment (eg, physical therapies, pain management, counselling) early.
- If you have ongoing pain and other symptoms, or pain that’s worse than it should be after an injury, talk to your healthcare provider.

Complex regional pain syndrome (CRPS) is a condition that usually develops after an injury or trauma, eg, a fracture, sprain, crush, or surgery. It’s not very common but is a recognised medical condition. It usually affects a single arm or leg, but over time can affect other parts of your body.
Symptoms generally start within a month of the trauma and continue for longer than would be expected after an injury or event.
There are 2 types of CRPS. They have similar symptoms but different causes:
- Type 1 is the most common and happens after an illness or injury that didn’t involve nerve damage. It used to be called Reflex Sympathetic Dystrophy (RSD) or Sudeck’s atrophy.
- Type 2 happens after nerve injury and used to be called Causalgia. Nerve injuries can cause symptoms very similar to CRPS, but it's called CRPS if your symptoms go past the part of your body that's controlled by the injured nerve.
Symptoms like CRPS that happen after a heart attack or stroke are usually called Shoulder-Hand Syndrome.
The cause is not well understood. It generally starts after an injury, but clearly not everyone who has an injury develops CRPS.
CRPS happens when there is an over-reaction to trauma by multiple body systems, including the immune system, peripheral nervous system (arms and legs) and central nervous system (brain and spinal cord). When these systems don’t switch off like they should after an injury is healed, or enough time passes, they can become over sensitive and stop working properly.
Psychological symptoms (eg, stress and anxiety) do not cause CRPS, but are very normal responses when you're trying to cope with the challenging symptoms of CRPS. Unfortunately, they can make CRPS symptoms worse by chemically increasing the sensitivity of the body systems involved in CRPS. This is why it's important to try and reduce stress levels.
Who is at greater risk of CRPS?
You are more at risk of developing CRPS if you're a woman around the age of menopause, and if your arm or leg is kept still for a long time.
The pain can feel like stabbing, stinging, burning, aching, or a combination of those. It may be constant or variable, and you may experience flare-ups (or exacerbations) of pain.
Other symptoms include changes related to sensations, temperature, sweating,swelling, movement and hair/nails/skin. These can include:
- tingling
- numb or sensitive skin on the affected area
- pain that feels more intense than it should in response to pressure or hot and cold
- swelling
- sweating or dry skin
- joint stiffness and swelling
- change in skin colour (white and blotchy, red, or blue)
- hair and nail growth changes
- muscle spasms, shaking, or weakness
- problems with movement
- feeling like your arm or leg doesn’t belong to you
- sleep problems.
These are early warning signs. If you have pain and more than 1 of these other symptoms, you need to talk about them with your healthcare provider as soon as possible.
Any healthcare provider can diagnose CRPS, but you may be asked to see a pain specialist to confirm your diagnosis. You should start treatment (eg, medicine, movement therapy, and desensitisation) with your GP, physiotherapist, hand therapist, and/or psychologist/counsellor even if your diagnosis of CRPS has not yet been confirmed. Your symptoms may get worse without treatment, so if you think you might have CRPS, talk to your healthcare provider as soon as possible.
There’s no single test used to diagnose CRPS so a diagnosis will be based on a physical examination and your medical history. Your healthcare provider will ask about your pain (eg, where it is, what it feels like, when it began) and any other symptoms you are experiencing.
Tests may be done to assess your sensation (feeling) and ability to move.
Other tests may be recommended – mainly to rule out other possible explanations. These could include:
The guidelines for diagnosing CRPS are called the Budapest Criteria. They state that all 4 of the following must be met for a clinical diagnosis to be made:
- Continuing pain which is disproportionate to any inciting event (more intense than would be expected after the event you experienced)
- At least 1 sign (based on evaluation or testing) in 2 or more of the categories
- At least 1 symptom (based on your experiences) in 3 or more of the categories
- No other diagnosis can better explain the signs and symptoms (eg, arthritis, infection, bone or soft tissue injury, peripheral nerve damage).
The categories are:
- Sensory: Unexpected or excessive pain response
- Vasomotor: Temperature asymmetry (difference between affected and unaffected limbs), skin colour changes
- Sudomotor/oedema: Swelling, sweating changes or asymmetry
- Motor/trophic: Decreased range of motion, movement problems (eg, muscle weakness, tremor, contractions), changes to hair, nails or skin.
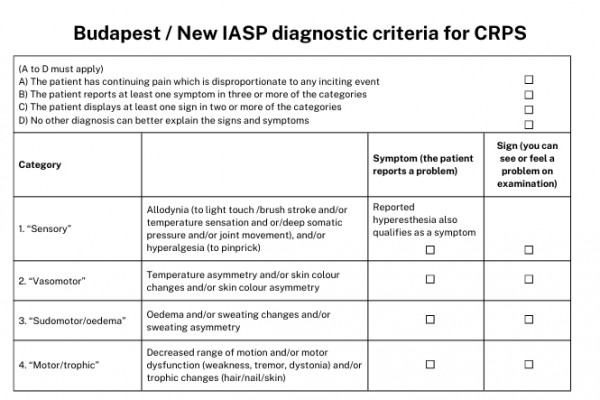
Image credit: Healthify He Puna Waiora adapted from Harden et al. 2022
Healthcare providers
Symptoms of CRPS vary from person to person so a range of healthcare providers from different disciplines are likely to be involved. Examples include:
- pain specialists
- GPs
- physiotherapists / hand therapists
- psychologists / counsellors
- occupational therapists.
There’s no simple cure for CRPS, so treatment aims to maintain and improve movement and function of your arm/leg, improve your quality of life, and manage your pain.
Treatment
Treatment approaches may include:
- providing you and your family/whānau with information about CRPS
- pain management medicines and techniques (eg, distraction, relaxation, mindfulness techniques, TENS machine, Rongoā)
- physical therapies including maintaining or increasing movement, strengthening muscles, and desensitisation (therapy to help sensations to your skin feel normal)
- mirror therapy to reduce pain and help you to move your arm/leg
- counselling and psychological support
- help with sleeping
- help with housework, childcare, transport, and/or return to work
- surgical interventions (many surgeons will be reluctant to operate if you have CRPS because it can make CRPS symptoms worse).
It’s important that any management or care plan is designed with you and specifically for you as an individual, taking into account how you and your family/whānau are affected by CRPS. It’s likely to involve setting goals to help you to see and measure your own progress. Read more about care planning and setting goals.
Apps reviewed by Healthify
You may find it useful to look at some Pain management apps and Meditation and mindfulness apps.
Many people’s CRPS symptoms will reduce. The amount of time this takes will vary for each person and is hard to predict. It's more likely if you are diagnosed and given the right treatment within the first few months of CRPS starting. However, treatment can be useful at any point of your CRPS journey, to help improve pain management, function, and quality of life.
Not everyone’s CRPS symptoms will go completely. Often the pain will continue. Some other symptoms will come and go, or change over the years – new ones can start and others fade. You can get better at managing your pain and other symptoms with fewer flare ups, and treatment can help with this.
When CRPS symptoms are settled you are in “remission”. This is called “CRPS with remission of some features”, and used to be called “CRPS not otherwise specified”.
CRPS can be a long-term, painful condition and it can be very difficult to live with. It’s important that you look after your physical and mental health.
It can help to:
- keep doing your daily activities as much as you can
- talk to whānau and friends and accept help when needed
- rest, and pace yourself with activities
- continue to do things you enjoy, eg, hobbies
- talk to a counsellor or therapist if you are having problems accepting your diagnosis or knowing how to live with CRPS
- join a support group so you can talk to others with the same condition.
Kiwi CRPS is a New Zealand based group who run 1 public and 3 private Facebook groups. These cater for:
- adults diagnosed with CRPS
- family and friends of adults with CRPS
- parents of children diagnosed with CRPS.
Read more about Kiwi CRPS(external link) and their support groups(external link) and have a look at the Rare disorders NZ(external link) website.
- Some research suggests if you take a high dose of vitamin C after a fracture or surgery you may reduce your risk of developing CRPS.
- Similarly, if you start moving as soon as you can after having an injury or stroke you reduce your CRPS risk.
Complex regional pain syndrome(external link) MSD Manual Consumer Version, NZ
Complex regional pain syndrome treatment(external link) NHS, UK
Book
The chronic pain couple(external link) Karra Eloff
Apps
Pain management apps
Meditation and mindfulness apps
References
- Chronic non-cancer pain(external link) Auckland Region HealthPathways NZ, 2018
- Complex regional pain syndrome (CRPS)(external link) Better Health, Australia
- Complex regional pain syndrome(external link) Mayo Clinic, US, 2022
- About CRPS(external link) Kiwi CRPS, NZ
- Complex regional pain syndrome in adults UK guidelines for diagnosis, referral and management in primary and secondary care(external link) Royal College of Physicians, UK, 2018
- Complex regional pain syndrome (CRPS)(external link) MSD Manual, NZ, 2022
- Complex regional pain syndrome(external link) NHS, UK, 2022
Clinical guidelines
Harden RN, McCabe CS, Goebel A, et al. Complex regional pain syndrome – practical diagnostic and treatment guidelines, 5th Edition(external link) Pain Med. 2022; 23(Suppl 1): S1–S53.
Complex regional pain syndrome in adults UK guidelines for diagnosis, referral and management in primary and secondary care(external link) Royal College of Physicians, UK, 2018
Wilson H, et al. Te Kete – diagnosis and explanations for patients with 'persistent somatic symptoms' and chronic pain(external link) NZ, 2024
Patient experiences
Griffiths GS, Thompson BL, Snell DL, Dunn JA. Experiences of diagnosis and treatment for upper limb Complex Regional Pain Syndrome – a qualitative analysis Pain Med. 2023;24(12):1355–1363
Webinar: Understanding Complex Regional Pain Syndrome
Apps
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Grace Griffiths, Master of Occupational Therapy, NZ Registered Hand Therapist, Hutt Valley; Deb Beazley Kiwi CRPS Charitable Trust
Last reviewed:





