You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Insomnia | Rarunga moe
Key points about insomnia
- If you have trouble getting to sleep or staying asleep you may have insomnia (rarunga moe).
- It can be short-term or temporary (acute), or long-lasting (chronic) if it’s lasted more than 3 days a week for more than 3 months.
- Lack of sleep can reduce your performance at work and put you at risk of accidents. If it lasts it can also affect your health and mood.
- Good sleep hygiene, cognitive behavioural therapy, sleep apps and, in some cases, medicines can help. Talk to your healthcare provider if your sleep problems continue.

Insomnia is a sleep disorder. It can affect how much sleep you get and the quality of that sleep.
If you have insomnia, you may experience:
- difficulty getting to or falling asleep
- difficulty staying asleep (poor sleep quality)
- waking up too early
- struggling with feeling tired and staying awake in the daytime as a consequence.
The amount of sleep you need varies depending on your age and what else is happening in your life. The recommended amount of sleep for an adult is at least 7 hours. If you wake up feeling refreshed and can function well throughout the day, you're getting enough sleep. Read more about how much sleep is enough.
There are 2 main types of insomnia:
- Acute insomnia: Insomnia that is short-term which lasts a few days and is temporary.
- Chronic insomnia: For some people, insomnia may be ongoing, lasting more than a few days a week for more than 3 months.
Why is insomnia a problem?
If you have insomnia, you won't get enough good quality sleep and will be tired during the day.
- This can lead to poor work performance and an increased risk of car and work accidents.
- It also makes it harder to concentrate, remember things, make decisions and solve difficult problems.
- Insomnia over many months or years can also affect your health and mood. It can increase your risk of depression, anxiety, heart disease, high blood pressure and diabetes.
The good news is that there are things you can do to help your sleep and reduce your risk of being affected by problems caused by insomnia.
The initial symptoms of insomnia may include:
- difficulty getting to or falling asleep
- difficulty staying asleep (poor sleep quality)
- waking up too early
- tiredness and fatigue in the day.
Ongoing or chronic insomnia can cause:
- poor concentration and memory
- loss of interest in usual activities
- irritability
- depression and anxiety about sleep
- poor work performance
- being at risk of work or motor vehicle accidents
- poor quality of life
- poor social functioning
- low libido (interest in sex).
Often insomnia starts in a time of stress (eg, a death, a break-up or job loss), and passes when the stress does. However, many other things can also cause insomnia.
Common causes of acute insomnia
- Alcohol (overuse or withdrawal).
- Nicotine (smoking).
- Caffeine late in the evening or at night.
- Eating too much late in the evening.
- Recreational drugs such as cocaine or ecstasy.
- Poor bedtime routine and sleep habits, eg, an inconsistent sleep schedule.
- Shift work (switching between day and night shifts).
- A poor sleep environment (eg, noise or light, a room that's too hot or too cold, an uncomfortable bed, or using your beds for something other than sleep or sex).
- Partner disturbance (eg, restlessness or snoring).
- Caring for babies and young children.
- Jet lag.
- Physical pain or discomfort in your body.

Image credit: Canva
Causes of chronic insomnia
- Physical health conditions including asthma, acid reflux (GORD), heart problems, chronic pain, allergies and itch due to eczema, Parkinson’s disease and dementia.
- Some prescription medicines such as steroid medications (prednisone), ADHD medications (methylphenidate), some of the antidepressants (SSRIs), antiparkinson medicines such as L-Dopa, beta blockers, diuretics causing the need to urinate in the night and others (check with your pharmacist).
- Menopause including hot flushes and night sweats.
- Urinary symptoms such as having to go to the toilet often in the night.
- Mental health conditions, eg, anxiety, depression, PTSD, psychosis.
- Sleep disorders, such as sleep apnoea, restless legs syndrome, sleep walking and circadian rhythm sleep disturbance.
Your healthcare provider will ask you questions about your sleep patterns, sleep routine, sleep habits and whether you have any existing health conditions. They will also ask you about your general wellbeing and mental health, and whether there's anything making you feel stressed or anxious.
Questions or issues to consider should include:
- your bedtime
- the time taken to fall asleep
- the number of times you wake up and what wakes you
- whether it's difficult to go back to sleep if you do wake in the night
- time spent asleep versus time in bed – ideally this should be more than 80%
- the quality of your sleep
- the regularity of your sleep routine – ideally this should be as regular as possible(eg, during the week at weekends and on holiday days) .
It's a good idea to record your sleep in a sleep diary(external link) for 2 weeks before going to see your healthcare provider.
Your healthcare provider may ask you to fill in a questionnaire (eg, the Epworth Sleepiness Scale)(external link) to find out how sleepy you are in the daytime and how it's affecting your daily functioning.
If possible, your partner or whānau members should be asked if they've noticed your disrupted sleep pattern and its impact on your everyday life.
You may also need a blood test to rule out other conditions that can cause the same symptoms. If there's concern about other sleep disorders, you may be referred to a sleep clinic for further tests and treatment.
Although insomnia can go away on its own, there are a few lifestyle changes and adjustments you can make to get a good night’s sleep.
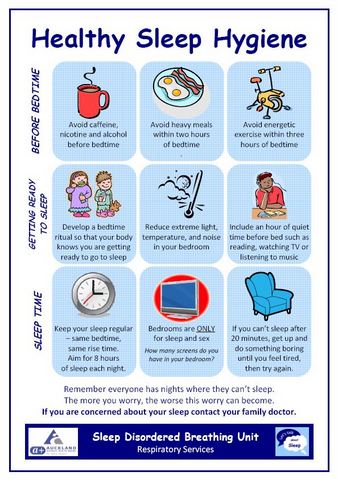
Sleep hygiene
Sleep hygiene refers to aspects of your lifestyle and bedtime environment that make it easier or harder to get better quality sleep.
Here are some changes you can make to improve your sleep hygiene:
- Go to bed at the same time every night – this will help set your biological clock so you start to feel drowsy at bedtime.
- Create your own bedtime ritual (eg, writing down the things on your mind that are worrying you or that you need to do tomorrow, making a hot, milky drink or taking a warm bath) and start it at the same time each night.
- Reduce or avoid caffeine, cigarettes and alcohol, especially in the evenings.
- Avoid large meals late in the evening, but don’t go to bed hungry – have a late snack if you need to.
- Exercise outdoors early or in the middle of the day, but best not too close to your bedtime.
- Avoid TV, computer screens and mobile phones for an hour or 2 before bed, as the artificial (blue) light interferes with your natural cues to sleep.
- Unwind before bed by reading or listening to music, doing yoga or meditating.
- Don't use your bed for work or catching up on social media – the time asleep in bed should be more than 80% of the total time you spend in bed.
- Get up if you can't sleep during the night.
- Make sure your bedroom is cool, dark and as quiet and comfortable for sleep as possible.
- Turn around any bedroom clocks – clock-watching makes insomnia worse.
- Try using mindfulness or relaxation techniques.
Read more tips to improve your sleeping habits. There's printable information about sleep and a checklist you can use to track your sleep hygiene behaviours in Te Kete Haerenga and sleep. Try filling in the Twenty Winks Sleep Questionnaire and get personalised sleep information.
Medicines for sleep
Medicines for managing sleep problems (eg, sleeping tablets) are usually only considered for short-term treatment of severe insomnia. They may be effective in the short term but there's no evidence of long-term efficacy or safety and they're not recommended for chronic insomnia. Medicines used to help your sleeping may also result in dependence.
Medicines that are generally used for insomnia include:
- Over-the-counter sleeping tablets or supplements which may be costly and not effective but may be worth a try (magnesium, herbal remedies such as valerian, chamomile, passion flower, tart cherry juice).
- Sleeping tablets, also called hypnotics (eg, zopiclone) or others.
- Benzodiazepines (eg, temazepam) generally should be a last resort for the treatment of chronic insomnia. There's a risk of daytime drowsiness which may limit their usefulness. In older adults there's an increased risk of falls. If benzodiazepines are used regularly, your body is likely to become dependent on them for sleeping and may habituate (get used to) to their effect. This means they'll work less well unless the dose is increased.
- Melatonin is mainly used if you need to change your body clock (eg, for jet lag or if you have delayed sleep phase disorder) when you have got into a habit of going to sleep and waking later than is normal or practical for you. It may not be helpful for chronic insomnia and higher doses can lead to bad dreams.
- Some sedating anti-histamines may help but there's a risk of daytime drowsiness which may limit how useful they are.
- Some antidepressants used at a low dose (eg, amitriptyline or mirtazapine) may be helpful for some people but there have been no clinical trials to prove this in large groups of people. There's a risk of daytime drowsiness and other side effects which may also limit the usefulness of these medications.
If you've have been prescribed medicines for sleep, your doctor should talk to you about your safety to drive(external link), as some of these medicines can have side effects. Read more about medicines for sleep problems.
Other supplements are also used for insomnia, but there's little (if any) evidence that they work.
Talk to your healthcare provider to find out the best treatment option for you.
If your insomnia has become chronic, see your healthcare provider. Medical conditions or sleep-related disorders causing ongoing sleep problems may need to be investigated and managed. Your healthcare provider may also recommend cognitive behavioural therapy for insomnia (CBTi) or sleep (or bedtime) restriction therapy.
Cognitive behavioural therapy for insomnia (CBTi)
This is a form of cognitive behavioural therapy (CBT) designed especially for people with insomnia (CBTi). It involves a trained provider helping to identify the thoughts, feelings and behaviours that are contributing to your insomnia. It will be different for each person, as it depends on your own particular circumstances and needs, but can include:
- education about sleep and sleep hygiene
- relaxation techniques
- sleep restriction (see below)
- addressing negative concerns and thoughts about sleep and insomnia
- homework (eg, keeping a sleep diary).
It’s been found to be very effective, with up to 80% of people experiencing improvement in their sleep.
It can be done by a trained doctor or sleep therapist. Just a Thought provides a free insomnia course you can do yourself online. Read more about how CBT-I works(external link) and the Just a Thought insomnia course(external link).
Online programmes include:
- Sleepio(external link)
- CBT for Insomnia(external link)
- The Sleep School(external link) (a cost is involved).
Sleep (or bedtime) restriction therapy
Sleep restriction therapy (also called bedtime restriction therapy) involves creating a new sleep schedule by limiting the amount of time you spend in bed, so that the time you spend in bed matches the time you actually sleep.
Spending a long time in bed awake may make your insomnia worse because you can spend this time feeling worried or frustrated about being unable to sleep. Sleep restriction therapy aims to decrease the amount of time it takes to fall asleep, increase the amount of time spent sleeping before you wake in the night and enable you to have more regular sleep patterns.
Sleep restriction therapy is often a component of CBTi and is best done under the supervision of a healthcare provider.
- To undertake sleep restriction therapy, it’s important to keep a sleep journal and strictly stick to the sleep schedules that are part of the therapy.
- It may temporarily result in more daytime sleepiness and there need to be precautions taken.
- Sleep restriction therapy isn't suitable for everyone. For example, it’s not recommended for people in certain occupations (eg, transportation, construction and healthcare) as they might put themselves or others at risk if they attempt to work while sleep deprived.
- It also may not be suitable for people with some health conditions (eg, major illness or recent surgery, untreated sleep apnoea, epilepsy or seizure disorders that are not well controlled, and untreated bipolar disorder).
- For sleep restriction therapy to work well, avoid falling asleep before bed (eg, while watching TV or reading) as this will decrease the need for sleep when you go to bed.
- You'll probably feel sleepier than usual when you wake-up in the morning and during the day. You'll start to need an alarm clock in the morning to ensure you don't sleep past the designated wake time. It's important to stick to the new schedule and not to nap during the day.
- Here are some examples of sleep restriction plans:
Apps reviewed by Healthify
You may find it useful to look as some Sleep apps and Cognitive behavioural therapy (CBT) apps.
Insomnia can cause daytime sleepiness and fatigue. If you need to drive, this can be extremely dangerous. Driver fatigue is one of the most common causes of motor vehicle accidents in New Zealand.
If you experience drowsiness during the day, it's important to stop driving and let your doctor know. Your doctor will need to find out the causes of your sleepiness and treat it accordingly. It's also a legal requirement that you only drive when you are medically fit – this includes not driving if you're too tired and sleepy.
The New Zealand Transport Agency has some fatigue resources(external link) to make it easier to manage driver fatigue. You can also read more about drowsy driving tips.(external link)
See your healthcare provider as soon as possible if you feel very sleepy during the day while driving, or your job involves operating machinery or aircraft.
The following links take you to other websites that provide further information on insomnia. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
Insomnia (beyond the basics)(external link) UpToDate, US
Tips for getting a good night's sleep(external link) Here to Help, Canada
The complete guide to insomnia and how you can manage it(external link) How To Sleep, UK
Brochures
Healthy sleep hygiene [PDF, 306 KB] Health New Zealand | Te Whatu Ora Auckland
Common sleep problems(external link) Health Information Translations, 2020 available in the following languages: English(external link), Arabic(external link), Chinese (simplified)(external link), Chinese (traditional)(external link), French(external link), Hindi(external link), Japanese(external link), Korean(external link), Nepali(external link), Russian(external link), Somali(external link), Spanish(external link), Vietnamese(external link)
Sleep problems [PDF, 931 KB] Healthify He Puna Waiora, NZ, 2019
Apps
Sleep apps
Mental health and wellbeing – CBT apps
References
- Insomnia(external link) 3D HealthPathways, NZ, updated 2024
- I dream of sleep – managing insomnia in adults part 1(external link) BPAC, NZ, 2017
- I dream of sleep – managing insomnia in adults part 2(external link) BPAC, NZ, 2017
- Overuse of benzodiazepines – still an issue?(external link) BPAC, NZ, 2015
- Insomnia treatment in NZ(external link) NZMJ, 2012;125:1349
- The assessment and management of insomnia in primary care(external link) The BMJ, UK, 2011
- What doctors wish patients knew about insomnia(external link) American Medical Association, US, 2022
- Insomnia(external link) Sleep Foundation, US, 2024
- Cognitive behavioral therapy for insomnia (CBT-I) – an overview(external link) Sleep Foundation, US, 2024
- Melatonin(external link) Mayo Clinic, US, 2023
- Sleep restriction therapy(external link) Sleep Foundation, US, 2023
- Insomnia disorder bedtime restriction therapy(external link) Australasian Sleep Association, Australia
I dream of sleep – managing insomnia in adults part 1(external link) BPAC, NZ, 2017
I dream of sleep – managing insomnia in adults part 2(external link) BPAC, NZ, 2017
Melatonin: is it worth losing any sleep over?(external link) BPAC, NZ, 2015
Overuse of benzodiazepines – still an issue?(external link) BPAC, NZ, 2021
Insomnia treatment in NZ(external link) NZMJ, 2012;125:1349
The assessment and management of insomnia in primary care(external link) The BMJ, UK, 2011
Sleep hygiene and lifestyle steps patient can take to improve sleep handout(external link) BPAC NZ, 2017
Author in the room – Daniel J. Buysse, MD talking about insomnia(external link) Institute of Healthcare Improvement, 2013
Insomnia disorder bedtime restriction therapy(external link) Australasian Sleep Association, Australia
Brochures
Auckland DHB, NZ
Health Information Translations, 2020
English, Arabic, Chinese (simplified), Chinese (traditional), French, Hindi, Japanese, Korean, Nepali, Russian, Somali, Spanish, Vietnamese
Healthify He Puna Waiora, NZ, 2019
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Roland Meyer, Specialist Physician, Respiratory and General Medicine
Last reviewed:





