You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Obstructive sleep apnoea | Mate hoto hau
Key points about obstructive sleep apnoea (OSA)
- Obstructive sleep apnoea (OSA or mate hoto hau) is a condition where you stop or decrease breathing while you're asleep.
- It's caused by the muscles in your airway relaxing when you're asleep and narrowing or blocking your airways. You then stop breathing (apnoea) or breathe less (hypopnoea) until your brain wakes you up. It usually involves snoring.
- OSA leads to poor, disrupted sleep and daytime sleepiness.
- It affects 2–10% of adult women and 4–25% of adult men. Being very overweight is the main risk factor.
- Treatment can include losing weight, avoiding lying on your back, continuous positive airway pressure (CPAP), dental/oral appliances and surgery.

Obstructive sleep apnoea (OSA) is when muscles in your throat, your tongue and soft palate relax during sleep. This causes narrowing of your airways and a potential collapse of your upper airway. OSA will make you breathe less deeply and you may stop breathing for a while. Your brain then wakes you up, the muscles tense up again and you're able to start breathing again. Often you won't be aware of it or remember it when you wake up.
Snoring is usually part of this problem. Snoring is the sound your breathing makes when the air is passing through a narrowed airway.
People with less space in the back of their throat will be affected more. For this reason if you are seriously overweight you will be more at risk of OSA. However, it can also be a problem if you have upper airways affected by anatomy, such as an underdeveloped lower jaw (retrognathia). Children with abnormally large tonsils may also get OSA. Read more about snoring and obstructive sleep apnoea in children.
If you have OSA, your sleep ends up being interrupted. The impact is similar to having a pillow in your face. As a consequence, OSA affects your sleep quality and reduces the number of hours of good sleep you get. This can make you wake up feeling unrefreshed and feel sleepy during the day. If you sleep well otherwise, you may be able to compensate for this. If not, and if there are other factors affecting the quality of your sleep, there'll be an increased risk of daytime sleepiness, having accidents, and low mood.
If this process continues for years it may also impact on cardiovascular conditions such as high blood pressure and arrhythmias and diabetes.
Everybody may snore and experience short episodes of breathing less when sleeping, but if it happens often it will become a problem.
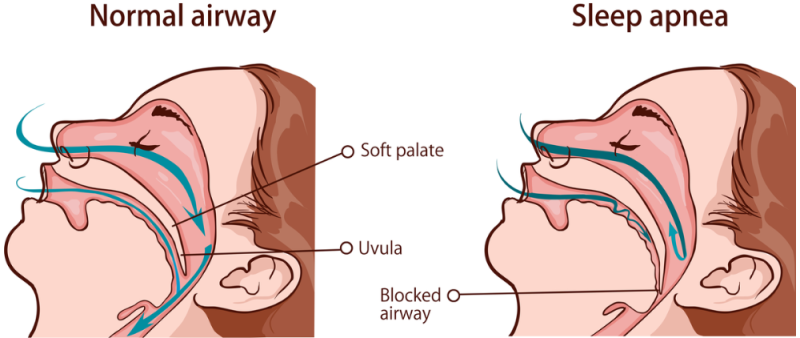
Image credit: Depositphotos
If you have OSA, the muscles in your airways relax too much, and block your airways while you're asleep. When this happens, you stop breathing for a short time until your brain wakes you up to begin breathing again. This cycle can repeat hundreds of times a night. Often you don't know this is happening, but it can reduce the quality of your sleep.
You are at higher risk of getting obstructive sleep apnoea if you:
- are obese (the most important risk factor)
- are a man (men are 2 times more likely to get OSA than women)
- are 40 years of age or over
- are Māori or Pasifika
- have a family history of OSA
- have a small jaw, small throat or nose/throat abnormalities
- have a neuromuscular disease
- are pregnant or have pre-eclampsia
- have hypothyroidism
- have polycystic ovary syndrome (PCOS)
- have big tonsils (most common in children and young people).
Video: What causes snoring and obstructive sleep apnea?
(Capital Otolaryngology Head and Neck Surgeons, US, 2010)
Symptoms of OSA you may have include:
- snoring
- waking up in the morning feeling tired (daytime sleepiness) and groggy
- having early morning headaches
- difficulty concentrating and finishing tasks
- altered mood
- stopping breathing during sleep for 10 seconds or longer (your bed partner can report this)
- waking up frequently with choking
- a dry mouth or sore throat for no apparent reason
- getting up several times a night to go to the toilet.
Some of the symptoms of OSA are similar to other conditions, so it’s important to see your healthcare provider to find out what's causing your symptoms. Your bedpartner may be able to confirm several of these signs.
See your healthcare provider if:
|
If it's left untreated, OSA can cause short or long-term:
- poor sleep quality
- poor work performance
- work accidents if you have a high-risk occupation, eg, heavy machine operator
- motor vehicle accidents
- short-term memory problems
- depression
- hypertension (high blood pressure)
- heart arrhythmia (irregular heartbeat)
- increased risk of cardiovascular diseases, such as heart disease and stroke
- impaired development in children.
Your healthcare provider will take a detailed history of your problem and examine your throat and neck. They will also review your medicines to find out if any of them is causing your sleepiness. You may also be asked to complete sleep questionnaires including the Epworth sleepiness scale (ESS)(external link) as one measure of how sleepy you are during the day. It can be helpful for your spouse or partner to be present, as they can explain what happens to you during sleep.
Blood tests
Blood tests such as a full blood count, thyroid function test or renal function test may be used to exclude other conditions (eg, underactive thyroid) and look for other complicating factors.
Sleep studies
A sleep study test is required to fully investigate this condition. There are different types of sleep studies most of which are done while you sleep in your own bed at home.
Pulse oximetry
The most simple sleep study is called pulse oximetry. This records your oxygen levels and heart rate. It assesses whether, and how often, your oxygen levels drop as a consequence of not breathing.
More comprehensive sleep study tests also record:
- noise levels due to snoring
- the position you're in while asleep – some people only have OSA when lying on their backs (supine-related OSA)
- your chest and abdominal movement when you're breathing, and
- your leg movements.
Generally, the results from these simple tests and questionnaires plus feedback from bedpartners should be enough to make a diagnosis.
Polysomnography test
Rarely, a more detailed sleep study may be done in a dedicated sleep laboratory to see how well you sleep. Polysomnography records a number of measurements such as:
- pauses in your breathing
- brain wave activity (EEG)
- sleep cycle (amount of deep sleep and rapid eye movement sleep)
- sleep position
- leg movements and more.
The tests above provide the oxygen desaturation index (ODI) or the apnoea/hypopnoea index (AHI). These tests measure how many times your oxygen level drops (ODI) or you breathe a lot less, or not at all, for 10 seconds or more in an average hour. An ODI or AHI of 5 or less is normal, if it's greater than 5 a diagnosis of OSA is made. An AHI of 6 to16 is classified as mild, 16 to 30 as moderate and greater than 30 as severe OSA. The total time when you have low oxygen levels (T90) is also highly relevant.
If a sleep study test result doesn't match the questionnaire findings, a repeat or more elaborate test may be needed.
Treatment depends on the severity of your OSA. If you have mild OSA, such as snoring only without daytime sleepiness, it can just be treated with lifestyle changes. If your OSA is more severe, treatment may include continuous positive airway pressure (CPAP), a dental or oral appliance, or surgery.
Lifestyle changes
Here are some changes that can help your OSA:
- Lose weight if you're obese or overweight – (reducing your weight by as little as a few kg can make a big difference. It's important to note that even if you're not overweight, if you have other issues affecting your airways (eg, your anatomy) you may snore and have apnoea. If you have mild or moderate OSA it can quite quickly become severe if you gain even a few kgs.
- Quit smoking if you smoke.
- Avoid alcohol and medicines that make you sleepy before bed – they can increase snoring and the development of sleep apnoea.
- Exercise regularly.
- Avoid sleeping on your back – some people only have potentially severe OSA when sleeping on their back.
- Maintain good sleep habits and sleep hygiene. Read our sleep tips to help with this.
- Do what you can to improve your sleep quality and duration to decrease the impact of OSA.
Continuous positive airway pressure (CPAP)
Continuous positive airway pressure (CPAP) is the most commonly prescribed treatment for OSA. It uses a small air generator which produces air pressure to keep your airway open while you sleep. You will have a choice of different masks to wear during the night while you're sleeping. The mask will be fitted to your nose or face. This method is currently the best treatment option for OSA as the machine (with the best settings) will make sure your airways are open, allowing you to sleep properly.
CPAP should ideally be used all night every night, but as a minimum it should be used 5 nights a week for at least 5 hours per night.
Many people feel much better within a few days of beginning CPAP as they get the benefit of deep restorative sleep. However, you may find it takes a few weeks to get used to wearing the mask and the sound of the machine. The more time you spend using your CPAP machine, the more you'll get used to it. Read more about continuous positive airway pressure (CPAP).
If your OSA is severe you may be eligible for publicly funded CPAP therapy through your local hospital. It's not advisable to get a CPAP machine from another source, without a proper assessment by a qualified health professional. CPAP machines cost about $2000.
Dental or oral appliances
Dental appliances such as special mouthguards and other devices can be used if:
- you have less severe OSA
- you're not seriously overweight, or
- you can’t use CPAP.
Off the shelf products are widely available but often don't work well. It's better to get an oral appliance from a specialist health professional.
Surgery
Surgery might be helpful when specific abnormalities, such as enlarged tonsils or a blocked nose, are contributing to your condition. There's also some evidence that it might be an option for some other people if CPAP doesn't work for them. A specialist ear, nose and throat (ENT) surgical assessment will be needed. Speak to your healthcare provider about the possibility of a referral.
Referral process
Referrals for a public service sleep assessment can be sent to your regional hospital service. A letter with the relevant details and a completed sleep questionnaire are usually required. If you meet the referral criteria you will be prioritised according to need, so wait times will vary. In some regions an initial assessment may be done in the community.
Apps reviewed by Healthify
You may find it useful to look at some Sleep apps, Snoring apps, Breathing apps and Nutrition, exercise and weight management apps.
The following video presented by an ear, nose and throat (ENT) surgeon provides some background to snoring and sleep apnoea and some simple exercises you can try.
A shorter version(external link) is available, but in this one he talks quite quickly so you might want to use your player settings to slow it down a little.
One of the main symptoms of OSA is daytime sleepiness and fatigue from lack of good, proper sleep. If you need to drive, this can be extremely dangerous as driver fatigue is one of the most common causes of motor vehicle accidents in Aotearoa New Zealand.
If you often get sleepy while you're driving, it's important to take a break each time, but also to let your healthcare provider know. They will need to find out the cause of your sleepiness and treat it accordingly.
It's a legal requirement that you only drive when you're medically fit, which means not driving if you're too tired and sleepy. The New Zealand Transport Agency has some fatigue resources(external link) to make it easier to manage driver fatigue. See also drowsy driving tips(external link).
See your healthcare provider as soon as possible if you feel very sleepy during the day while driving, or if your job involves operating machinery or aircraft.
Your driver's licence may be revoked (withdrawn) until a full sleep assessment has been done and your treatment is shown to be working. It's acknowledged that this will be very stressful – particularly if you're a commercial driver.
Members of the Sleep Apnoea Association of NZ Inc (SAANZ) are available to provide support for queries by phone (021 344 253) or email [email protected]). If you have any queries about sleep apnoea, diagnosis, or treatment or are struggling to get used to using CPAP, they are happy to be contacted.
The following links take you to other websites that provide further information on OSA. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
Obstructive sleep apnoea(external link) Asthma + Respiratory Foundation, NZ
Fatigue resources(external link) NZ Transport Agency
Drowsy driving tips(external link) University of Otago, Wellington Sleep Investigation Centre, NZ
Obstructive sleep apnoea and CPAP therapy(external link) Well Sleep, University of Otago, Wellington, NZ
Obstructive sleep apnoea syndrome(external link) Patient Info, UK
The effects of sleep deprivation on your body(external link) Healthline, US
Brochures
Obstructive sleep apnoea [PDF, 2.2 MB] Auckland DHB, NZ
Healthy sleep hygiene [PDF, 306 KB] Auckland DHB, NZ
Sleep problems [PDF, 931 KB] Healthify He Puna Waiora, NZ and Mediboard 2023
Obstructive sleep apnoea poster [JPG, 103 KB] Health New Zealand | Te Whatu Ora, NZ, 2024
Attending your oximetry appointment [PDF, 1 MB] Health New Zealand | Te Whatu Ora, Counties Manukau, NZ
Apps
Sleep apps
Snoring apps
Breathing apps
Nutrition, exercise and weight management apps
References
- Obstructive sleep apnoea in adults(external link) 3D Regional HealthPathways, NZ, 2025
- Obstructive sleep apnoea in adults(external link) BPAC, NZ, 2012
- Obstructive sleep apnoea(external link) Starship, NZ, 2021
- Randerath W, Verbraecken J, de Raaff CAL, et al. European Respiratory Society guideline on non-CPAP therapies for obstructive sleep apnoea(external link) Eur Respir Rev. 2021;30(162):210200
- Medical aspects of fitness to drive – a guide for health practitioners(external link) NZ Transport Agency, 2014
Assessment tools
Epworth sleepiness scale(external link) Calculate by QxMD, 2015
STOP-Bang questionnaire(external link) STOP Bang Canada
The Mallampati Score(external link)
Tonsillar size assessment(external link)
Information and resources
Physical activity behaviour and barriers to activity in adults at high risk of obstructive sleep apnoea(external link) Journal of Primary HealthCare, NZ, 2020
Managing obstructive sleep apnoea and achieving equity: implications for health(external link) Medical Journal, NZ, 2011
Bakker, Jessie P., et al. Continuous positive airway pressure treatment for obstructive sleep apnoea – Maori, Pacific and NZ European experiences(external link) Primary Health Care. 2013; 221
Medical aspects of fitness to drive – a guide for health practitioners(external link) NZ Transport Agency, 2014
MacKay S, Carney AS, Catcheside PG, et al. Effect of multilevel upper airway surgery vs medical management on the Apnea-Hypopnea Index and patient-reported daytime sleepiness among patients with moderate or severe obstructive sleep apnea – the SAMS randomized clinical trial(external link) JAMA 2020;324(12):1168-1179
Australasian Sleep Association position statements (external link)
Continuing professional development
Video: Sleep apnoea and OSA – S Samant Ear, nose and throat update part 2 (19 minutes)
(PHARMAC, NZ, 2019)
For more videos of the same series, visit PHARMAC seminars.
Brochures
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Roland Meyer, Specialist Physician, Respiratory and General Medicine
Last reviewed: