If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Eczema | Mate harehare
Also known as atopic eczema or atopic dermatitis
Key points about eczema
- Eczema is a very common skin condition that causes your skin to be dry, itchy, red and swollen.
- It’s also called atopic eczema or atopic dermatitis.
- 'Atopic' is a term used to describe a group of conditions including asthma, eczema and hay fever. Eczema is more common if you, or a family member, has one of these conditions.
- Eczema most often happens in babies and children, though sometimes it can occur for the first time when you're an adult.
- There’s no cure for eczema and it needs to be managed well on a daily basis to keep symptoms under control.

Eczema, also called atopic eczema or atopic dermatitis, is a very common skin condition that causes your skin to be dry, itchy, red and swollen (inflamed).
‘Atopic’ is a term used to describe a group of conditions such as asthma, eczema and hay fever. Atopic eczema is more common if you have one of these conditions or a whānau (family) member has one.
Atopic eczema occurs most frequently in pēpi (babies) and tamariki (children). But it can sometimes occur for the first time when you’re an adult. Many tamariki grow out of atopic eczema, but it can return years later. Read more about eczema in children.
Video: What is eczema? | Patient explainers
The exact cause of eczema is not known but it's believed that a combination of genes and environmental factors cause it.
Eczema is an atopic condition which means it happens for people who have a genetic tendency to react to allergens. Other atopic conditions include hay fever and atopic asthma. You're more likely to get eczema if you or a whānau member has another atopic condition.
Some people with eczema have a lower amount of a protein called filaggrin. This protein plays an important role in keeping your skin barrier healthy. Having less filaggrin leads to dry skin and increases the risk of developing eczema.
People with eczema also tend to have an overactive immune system. This can be triggered by a substance inside or outside of the body, causing inflammation.
Eczema triggers
A trigger is something that causes your eczema to flare up. Common triggers include:
- heat or changes in temperature
- irritants such as soap, bubble bath, detergent, fabric conditioner and perfumed products
- fabrics such as wool or synthetic materials, which can be prickly
- chemicals such as chlorine in a swimming pool or chemicals in a spa
- stress
- food allergies such as cows milk
- environmental allergens such as animal dander, pollen or house dust mites.
The main symptom of eczema is itching. This itching can be moderate to severe, and is often worse at night. Your skin may also become dry, inflamed and cracked.

Image credit: Canva
When your eczema becomes worse it's called a flare-up – this can last for a few weeks.
- If it's mild, it can involve 1 to 2 areas of skin.
- If it's severe, it can involve many areas of your skin.
Eczema can affect any area of your skin. In adults it is most common on:
- your wrists
- the inside of your elbows
- the backs of your knees
- your torso
- your limbs.
It can sometimes affect your face and genital areas.
Complications from eczema
Sometimes your skin can become infected. Signs and symptoms of infection include:
- skin that's weepy and crusted
- lots of white or yellow pimples
- a sudden flare-up of eczema all over your body
- shivering
- painful skin
- painful blisters that look like chickenpox.

Image credit: DermNet NZ
Your healthcare provider will usually diagnose eczema based on your medical history. They will talk to you about your symptoms and look at your skin.
Blood tests and skin tests aren't usually needed.
Self-care
- Moisturise your skin to keep it hydrated. Use colour and fragrance free products. There are many types of moisturisers – you can ask your pharmacist for advice. If your eczema is moderate or severe talk to your healthcare provider.
- Bathe or shower daily to help moisturise your skin. Use soap substitutes such as an aqueous cream.
- Use anti-inflammatory steroid cream. Ask your pharmacist for advice on what cream is best for you.
- Keep your nails short to avoid scratching yourself. This can lead to inflammation and infection.
See eczema medicines and eczema in children for more information on treating atopic eczema.
If you have severe eczema that doesn't respond to treatment, your healthcare provider may refer you to a dermatologist (skin doctor). You can also pay to see a private dermatologist. You can find a private dermatologist on Healthpoint(external link).
Apps reviewed by Healthify
You may find it useful to look at some eczema apps.
The key to avoiding flare-ups of your eczema is to:
- moisturise your skin regularly
- know your triggers for eczema flare-ups
- avoid your triggers where possible
- use any medications from your healthcare provider or pharmacist as recommended.
Brochures
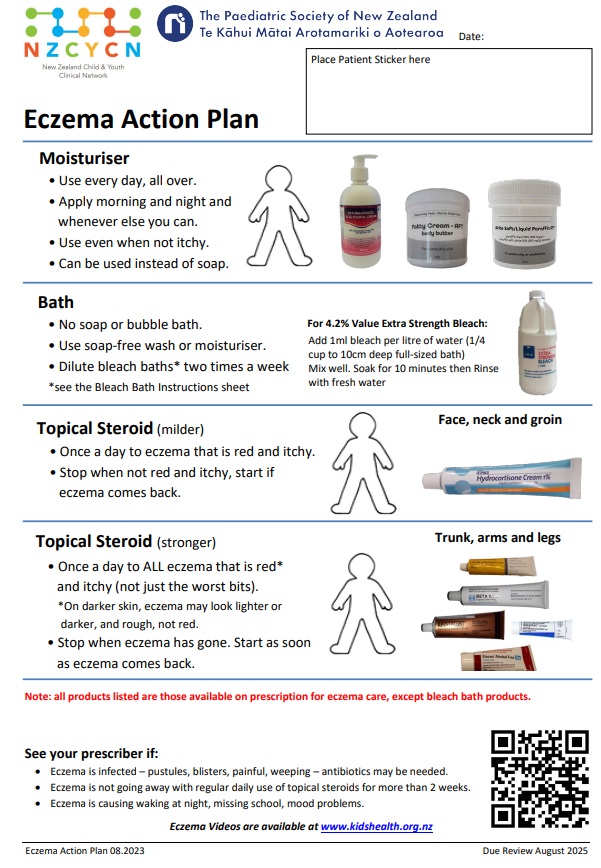
New Zealand Child & Youth Clinical Network, 2023
New Zealand Child and Youth Clinical Network, 2023
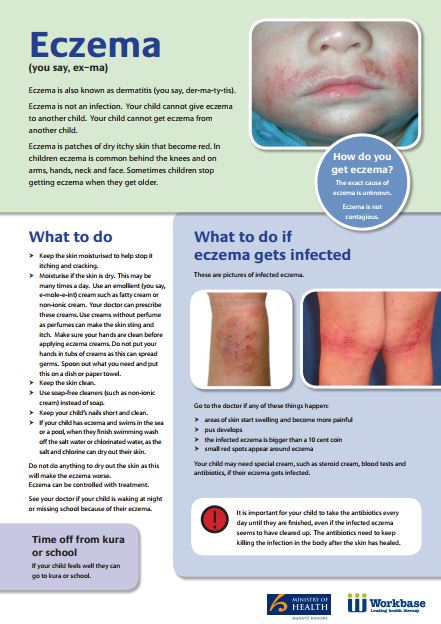
Health Literacy NZ
Credits: This content has been collaboratively developed by Health New Zealand | Te Whatu Ora, KidsHealth, and Healthify He Puna Waiora to provide trusted health information.
Last reviewed:





