You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Sleep problems
Key points about common sleep problems
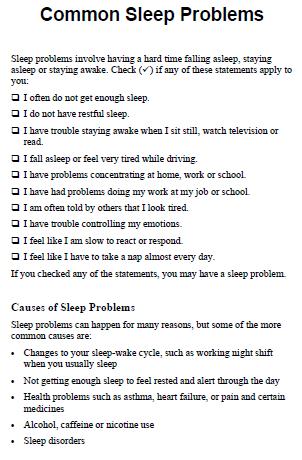
- Nearly everyone has difficulty getting to sleep from time to time, but for some people, sleep can be a regular ongoing problem.
- Poor sleep not only makes you feel tired, but can really interfere with your day-to-day functioning and affect your health.
- Taking a close look at what's happening can help you work out the cause of the problem.
- Learning how to manage sleep problems can greatly improve your quality of life.

Insomnia
- This is a condition where you have trouble sleeping or staying asleep for long enough.
- It generally includes difficulty getting to sleep, staying asleep (poor sleep quality) or waking much too early.
- Read more about insomnia.
Obstructive sleep apnoea (OSA)
- This is a condition where you stop breathing while you're asleep.
- The usual symptoms are snoring, not feeling refreshed on waking, feeling sleepy during the day, altered mood and morning headaches.
- Read more about obstructive sleep apnoea.
Snoring
- This is where you make a snorting or rattling noise when you breathe during sleep.
- The noise comes from the vibrating of the soft palate and tissue in your mouth, nose or throat.
- Some people snore occasionally and the sound they make isn't too loud, while others may snore every night, loud enough to be heard in the next room.
- See our tips to reduce snoring.
Sleep deprivation
- This is a condition that develops if you don't get enough sleep, or you sleep at the wrong time of day (that is, you're out of sync with your body's natural clock).
- It also includes not sleeping well or not getting all of the different types of sleep that your body needs.
- Read more about the different types of sleep, signs you aren't getting enough sleep and sleep deprivation and parenting.
Restless legs syndrome
- This a sleep disorder that causes an intense, often irresistible urge to move your legs. This sensation is brought on by resting, for example lying down in bed or sitting for prolonged periods, such as when you're driving or watching a movie.
- It typically occurs in the evening, making it difficult to fall asleep and stay asleep.
- It can lead to daytime sleepiness, irritability and concentration.
- Read more about restless legs syndrome.
Tiredness during the day is usually how you know you have a sleep problem. If you sleep in the same room or bed with someone else, they may tell you about problems they notice during the night. If you often have trouble getting to sleep, or if you often wake during the night, then you may not be getting enough sleep. Some of the tools or quizzes used to assess sleep are shown below.
Tools and quizzes to assess your sleep
You can fill these in at home and if the results indicate that you may have a sleep problem, print your results and discuss these with your healthcare provider.
- Twenty Winks Sleep Questionnaire Goodfellow Unit and Healthify He Puna Waiora
- Provides you with personalised information and links to more information based on your responses.
- The Auckland Sleep Questionnaire(external link) Goodfellow Unit, University of Auckland
- To help you establish the causes of your sleep problems.
- The Epworth Sleepiness Scale(external link)
- To help you recognise possible sleep apnoea.
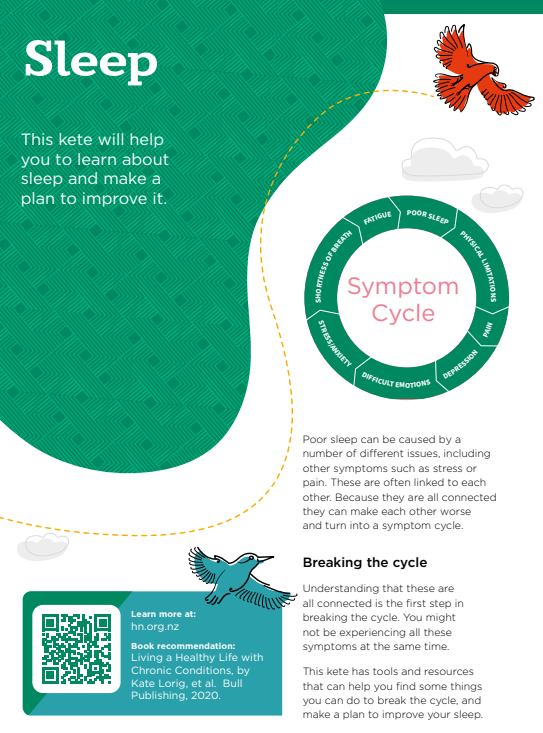
- Te Kete Haerenga sleep and sleep tips [PDF, 66 KB] Healthify He Puna Waiora
- Use this sleep tracker to see what you are doing during the day and before sleep to help you improve your sleep habits.
Sleep tracking apps can help you understand your sleep patterns better. Some can measure your body movements to track whether you're asleep, awake or restless in your sleep. Other tracking apps have a diary function where you can record lifestyle activities related to sleep.
Wearable devices can measure sounds, your pulse or movements at night to estimate your sleep. They can be inaccurate, for example. if you're lying very still the device may record this as sleep. Read more about sleep apps.
Importance of sleep
Not getting enough sleep, or getting poor-quality sleep, increases your risk of high blood pressure, heart disease, obesity and diabetes. That means it’s important to make changes so you can get good quality sleep.

Image credit: 123rf
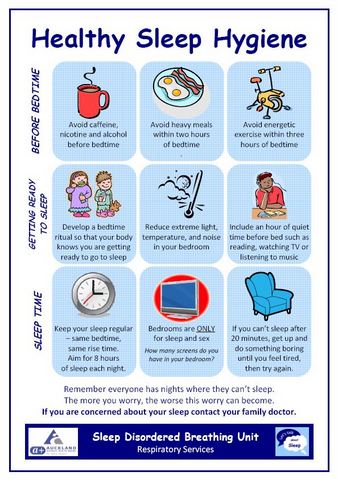
If you're experiencing the effects of poor sleep, making a few changes to your daily routine and habits can make a big difference. Try these strategies to help you sleep better at night.
- Set your body clock – go to bed and get up at the same times each day, including weekends.
- Wind down at bedtime – have an hour of quiet time before bed; switch off your electronic device, read, have a bath or listen to music.
- Avoid stimulants – within 2 to 3 hours of bedtime:
- don’t smoke
- don't drink alcohol or caffeinated drinks
- don't eat a heavy meal
- don't do energetic exercise.
- Make your bedroom suitable for sleep – keep it cool, dark and quiet and use it only for sleep and sex.
- Reduce blue light exposure in the evening – it disrupts your body clock, causing poor sleep. If you use your phone or computer in the evening switch it to night-time setting or, better still, turn it off.
- Get up if you can’t sleep – if you can’t sleep after 20 minutes or so, get up and do something boring until you feel tired, then try again. Don’t lie in bed getting frustrated.
- Avoid naps – try not to sleep during the day.
- Be active in the day – take regular daytime exercise and get outside early to help set your body clock for a good night’s sleep.
- Use an app – try an app or online sleep programme.
See also these tips to improve your sleeping habits and our Te Kete Haerenga toolkit for understanding more about your sleep and making a plan to improve it.
If lifestyle changes haven't helped, talk to your healthcare provider about whether you need other treatment. Your healthcare provider will want to find out about what's been happening in your life, your pattern of sleep and whether you have any other health conditions. This is because the treatment for sleep problems varies depending on the underlying issue.
Insomnia
- Finding out if there is an underlying cause and treating that cause is important.
- Setting up good sleep habits (sleep hygiene) is the first step – see what to do to improve your sleep.
- Sleep restriction therapy involves creating a new sleep schedule by limiting the amount of time you spend in bed, so that the time you spend there matches the time you actually sleep.
- Another possible treatment is a type of cognitive behavioural therapy (CBT) that is specifically designed for people with insomnia (called CBT-I). The aim is to change unhelpful thoughts and behaviours that may be contributing to your insomnia. It's an effective treatment for many people and can have long-lasting results. Read more about CBT-i(external link).
- Read more about insomnia.
Obstructive sleep apnoea
- The treatments for sleep apnoea include weight loss, cutting down on alcohol, the use of dental appliances such as mouthguards, and continuous positive airway pressure (CAP) machines.
- Read more about obstructive sleep apnoea.
Snoring
- Try sleeping on your side, as this sometimes works for some people. Do this by:
- using a pillow or bolster to keep you on your side
- putting something (eg, a tennis ball) under your back to make it uncomfortable to lie on your back
- using a device that vibrates when you lie on your back, waking you and reminding you to turn over.
- Making changes to your lifestyle such as losing weight, cutting down on alcohol and quitting smoking can be helpful.
- Talk to your healthcare provider or dentist about special devices you can use in your nose or mouth to reduce your snoring.
- Read our tips to reduce snoring.
Sleep deprivation
- The aim of treatment for sleep deprivation is to increase your total sleep time.
- This is mainly done by treating the cause of your sleep deprivation.
- Your healthcare provider will help you assess the causes of your interrupted sleep.
- Read more about signs you're not getting enough sleep and coping with sleep deprivation as a new parent.
Restless legs syndrome
- Healthy diet, exercise, massage, heat or ice packs, avoiding smoking, and distraction can all help.
- There are several medicines you can try.
- Read more about restless legs syndrome.
A note about sleeping medicines
Sleeping tablets or medicines that encourage sleep are not used often because they have the potential to cause harm. Using sleeping tablets on an ongoing basis can mean you become dependent on them. They can also increase your risk of falls, confusion, dementia and difficulties with driving.
Taking sleeping tablets for more than a few nights in a row can make your sleeping problems worse. If you're taking sleeping tablets regularly, ask your healthcare provider about ways to help you stop taking them. You may need to stop taking them gradually (over several weeks or months) before stopping completely.
Read more about sleeping medicines (hypnotics).
Video: Beditation – getting a better night's sleep (35 minutes)
Click the image below to visit the website, scroll down to see the video, then click play.  (external link)
(external link)
(NHS, UK, 2022)
Video: Tips for insomnia: The good sleep guide
Sleep(external link) Fresh Mind, NZ
Sleep disorders(external link) Medline Plus, National Institutes of Health
Why sleep matters(external link) Healthy Sleep – Division of Sleep Medicine at Harvard Medical School, US
Common sleep problems(external link) (13 languages) Health Information Translations
Tiredness and fatigue(external link) NHS Choices, UK
Things you can do to help you stop snoring(external link) NHS Choices, UK
Brochures
Sleep problems [PDF, 931 KB] Healthify He Puna Waiora and Mediboard, NZ, 2023
Healthy sleep hygiene [PDF, 306 KB]Auckland DHB, NZ
Common sleep problems(external link) Health Information Translations, 2020 English(external link), Arabic(external link), Chinese (simplified)(external link), Chinese (traditional)(external link), French(external link), Hindi(external link), Japanese(external link), Korean(external link), Nepali(external link), Russian(external link), Somali(external link), Spanish(external link), Vietnamese(external link)
10 tips for a better night sleep(external link) Farmstrong, NZ, 2018
Te Kete Sleep [PDF, 497 KB] Healthify He Puna Waiora, NZ, 2022
Sleep assessment quizzes
Twenty Winks Sleep Questionnaire Goodfellow Unit and Healthify He Puna Waiora, NZ
The Auckland sleep questionnaire(external link) (short version) Goodfellow Unit, University of Auckland, NZ
The Epworth sleepiness scale(external link) (MW Johns) QxMD
Sleep diaries
Sleep diary [PDF, 227 KB] Healthify He Puna Waiora, NZ, 2023
Apps
References
- Sleep deprivation and deficiency(external link) National Heart, Lung and Blood Institute, US, 2016
- de Gage SB, Bégaud B, Bazin F. Benzodiazepine use and risk of dementia – prospective population-based study(external link) BMJ 2012;345:e6231
- Hypnotics(external link) NZ Formulary, 2025
- Prescribing hypnotic medicines – a focus on zopiclone(external link) BPAC, NZ, 2018
- Blue light(external link) Health New Zealand | Te Whatu Ora
Continuing professional development
Webinar: Sleep health, insomnia and practical solutions(external link) Sally Powell, Nurse Practitioner, Masters of Health Sciences
About this presentation:
The impact of sleep deprivation can be significant, with often simple measures making a big improvement to wellness. The range of sleep disorders that affect sleep quality is vast and this presentation will:
- Improve knowledge of identifying the aspects of good versus poor sleep health
- Outline strategies to enable improvement in sleep quality and reduce the burden in this population.
Video: Sleep health, insomnia and practical solutions
You can watch the video, answer questions and claim hours with a certificate.
Sleep assessment questionnaires and scales
- Twenty Winks Sleep Questionnaire Goodfellow Unit and Healthify He Puna Waiora, NZ
- The Auckland sleep questionnaire(external link) (short version) Goodfellow Unit, University of Auckland, NZ
- The Epworth sleepiness score(external link) (MW Johns) QxMD
- Sleep profile quiz(external link) BBC, UK (5 to 10 mins to fill in online)
- Sleep diary (2 weeks)(external link) American Academy of Sleep Medicine
Updates and best practice guides for sleep problems and insomnia
Treating sleep issues(external link) Goodfellow Unit NZ, 2023
Insomnia podcast(external link) Prof Bruce Arroll Goodfellow Unit July 2017
I dream of sleep: Managing insomnia in adults – part 1 diagnosis and non-pharmacological treatment(external link) BPAC, NZ, 2017
I dream of sleep: Managing insomnia in adults – part 2 the idea pharmacological approach for improving sleep(external link) BPAC, NZ, 2017
Appropriate use of zopiclone and benzodiazepines for the treatment of insomnia(external link) BPAC, NZ, 2020
Melatonin – is it worthwhile for sleep?(external link) BPAC, NZ, 2024
(external link)Sleep changes in older adults(external link) Family Doctor, American Academy of Family Physicians, 2012(external link)
The Sleep/Wake Research Centre(external link) Massey University, Wellington
Videos
Sleep well and energise – a no pills approach(external link) Goodfellow Webinar, NZ, 2020
Dr Giresh Kanji discusses the risks of insomnia including anxiety, depression, early death, dementia, cancer, hypertension and ischaemic heart disease.
Sleep and sleep disorders(external link) by Dr Andrew Veale The Goodfellow Unit, NZ, 2018
Management of sleep problems(external link) Goodfellow Unit, NZ, 2020
Dr Matire Harwood from the University of Auckland discusses sleep problems, their causes and how good sleep habits can be developed.
Sleep restriction therapy
Sleep restriction therapy is a behavioural treatment for insomnia that works by reducing the amount of time spent in bed awake and not sleeping. Several studies have shown it to be effective for many people with insomnia.
Instructions for sleep restriction(external link) Kaiser Permanente Clinics, US
Falloon K, Elley CR, Fernando A, et al. Simplified sleep restriction for insomnia in general practice – a randomised controlled trial(external link) BJGP 2015;65(637):e508–e515
Brochures
Auckland DHB, NZ
Healthify He Puna Waiora, NZ, 2022
Health Information Translations, 2020
English, Arabic, Chinese (simplified), Chinese (traditional), French, Hindi, Japanese, Korean, Nepali, Russian,Somali, Spanish, Vietnamese
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed: