Angioplasty and stents
Also known as coronary angioplasty or percutaneous coronary intervention (PCI)
Key points about angioplasty and stents
- Angioplasty is a procedure to widen a blocked or narrowed coronary artery to improve blood flow to your heart.
- A stent (a short wire mesh tube) is inserted into your coronary artery using a thin tube (called a catheter) through an artery in your groin or wrist.
- The stent is left in place permanently. It keeps the blood vessel open and allows blood to flow more freely.

What is it?
Angioplasty is a procedure to widen a blocked or narrowed coronary artery to improve blood flow to your heart.
When is it done?
Angioplasty is done if the blood vessels to your heart (coronary arteries) are blocked or narrowed from a build-up of cholesterol and other substances (called plaque). This condition is known as atherosclerosis which can cause coronary artery disease.
The main symptoms of the blockage or narrowing are chest pain (angina) or shortness of breath. While angina can often be treated with medicines, a coronary angioplasty may be needed in severe cases where medicines aren't enough. After an angioplasty, many people find their symptoms get better and they're able to do more than they could before the procedure.
Angioplasty is also done as an emergency treatment after a heart attack, when blood flow to a section of heart muscle becomes blocked.
Angioplasty can increase your chances of surviving more than clot-busting medication (thrombolysis).
Coronary angioplasty is done by an interventional cardiologist (heart doctor) in the cardiac catheterisation laboratory of a hospital. A coronary angioplasty is performed using local anaesthetic, which means you'll be awake during the procedure. You will be given sedating medicines to make you sleepy and relaxed.
- The start of the procedure is the same as for a coronary angiogram.
- A catheter (which is a fine, flexible hollow tube), will be passed into an artery in either your groin or arm. A wire with a small, inflatable balloon at its tip is passed up the catheter. A fine wire mesh tube called a stent sits on the outside of the balloon.
- Your doctor will then use X-ray screening to direct the wire into a coronary artery until its tip reaches a narrow or blocked section. The balloon is then gently inflated.
- The stent expands with the balloon. As the balloon is inflated, it opens the stent against the artery walls.
- The balloon is deflated and removed.
- The stent stays in the artery to flatten the plaque against the artery wall, opening the artery to allow blood to flow more easily.
- During this time you may experience mild chest pain as the blood supply to the heart muscle is temporarily interrupted. It's important to let your doctor know if this happens.
Stents can be bare metal stents or drug eluting stents, which are coated in medicines to stop the artery blocking again. Your cardiologist will discuss with you which type of stent is the best for you.
Sometimes no stent is used and the balloon alone is used to press on the plaque and open the artery. This is called balloon angioplasty.
The image shows a catheter, balloon and stent placed into a coronary artery.
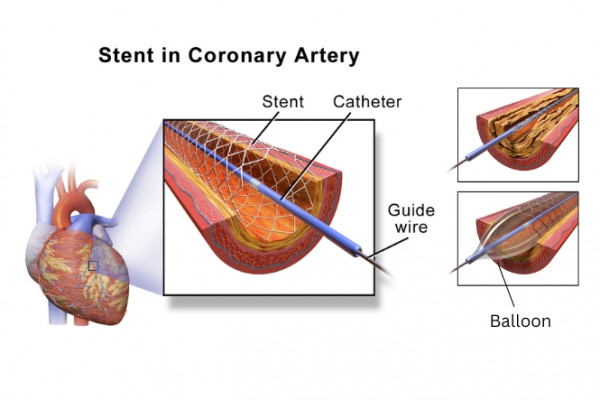
Image credit: Blausen Medical Communications, Inc.(external link)(external link) Wikimedia Commons (2 images combined)
Video: Heart stents – what you need to know
This video provides lots of information about angioplasty and coronary stents. It may take a few moments to load.
(Heart Matters, Australia, 2021)
A shorter video on coronary angioplasty(external link) can be watched on YouTube.
There will be a routine examination and some tests before the procedure, eg, blood tests and an electrocardiogram (ECG). A healthcare provider will explain the procedure and answer any questions you may have.
If you're are taking medicines (especially dabigatran, rivaroxaban or warfarin), your healthcare provider will advise you on whether to continue or stop taking it. You should take all your medicines to hospital with you.
When you return to the ward the nursing staff will monitor you closely until you're fully recovered. If the catheter was in your groin, it's usually removed about 2 to 4 hours after you get back to the ward. If the catheter was in your arm, it will be removed at the end of the procedure.
It's normal to have some bruising around the site and for it to be slightly tender. If you experience discomfort at the site, inform the nurse and you will be given pain relief. You may feel a small lump where the catheter was inserted, but this should disappear over the next few months. If this increases in size or becomes painful, seek medical advice.
Before you go home, a nurse will teach you how to check the site for bleeding and explain what to do if this happens. You'll be advised not to do any heavy lifting or straining for about a week. This is to prevent bleeding from the insertion site.
After an angioplasty you may go home that evening or stay the night in hospital and go home the following day. You will need to arrange for someone to take you home.
Before leaving hospital you'll be started on medicines, which must be continued when you go home. These will help prevent further heart problems. To prevent blood clots forming, you'll be given medicines including aspirin and either clopidogrel or ticagrelor. You should also take cholesterol-lowering medications (statins) which help protect you from further narrowings in the heart arteries and often you will also be prescribed medicines to lower your blood pressure. Always follow your doctor's instructions and don't stop taking any medicines without talking to your healthcare provider first.
After an angioplasty most people return to normal, everyday activities within 1–2 days of returning home, and can usually return to work after a week.
Remember that having an angioplasty is not a cure for heart disease. Your symptoms may have stopped, but you will still need to make, and maintain, changes to your lifestyle to prevent the angina returning. The best way to prevent further heart disease is to reduce or remove any risk factors. Every risk factor you reduce or remove can have a major effect on lowering your chances of having further heart disease problems, eg, angina or a heart attack.
Learn more about:
- stopping smoking
- exercise and physical activity
- eating and drinking for a healthy heart(external link)
- reaching a healthy weight.
You may also be invited to go on a cardiac rehabilitation programme.
The New Zealand Transport Agency (NZTA) cardiovascular guide(external link) states you mustn't drive for at least 2 days after an angioplasty.
If you have complications from the procedure, or you have had a heart attack resulting in angioplasty, you must not drive until you have been given medical clearance – this is generally 2 weeks for a car licence.
If you hold a vocational licence (eg, you drive passenger vehicles, trucks, forklifts, courier vans or fly aeroplanes) different rules apply. Your licence needs to be approved by a cardiologist or specialist who will examine you and make sure it's safe for you to drive.
It also pays to check with your insurance company to ensure you're fully covered.
All types of surgery have a risk of complications, but the risk of serious problems is small. Coronary angioplasty doesn't involve major surgery and doctors describe it as a minimally invasive form of treatment.
Risk factors
Overall, the risk of serious complications from a coronary angioplasty is small, but this depends on factors such as:
- whether the procedure was planned or was an emergency treatment
- your age
- your general health
- whether you've had a heart attack.
Your healthcare provider can give you more information about your individual risks and benefits.
Possible complications
- It's quite common to have some discomfort, bleeding or bruising under the skin where the catheter was inserted.
- Some people may be allergic to the contrast agent used during the procedure.
- More serious complications are less common but can include damage to the artery where the angioplasty was done, severe bleeding requiring a blood transfusion or a heart attack, heart rhythm problems, kidney problems, stroke or death.
Angioplasty – explained(external link) Watch, learn, live – interactive cardiovascular library – American Heart Association
Coronary stent – explained(external link) Watch, learn, live – interactive cardiovascular library – American Heart Association
Resources
A guide to coronary angiography & angioplasty(external link) Heart Foundation, NZ
References
- Angioplasty and stents(external link) Heart Foundation, NZ
- Coronary angioplasty(external link) NHS, UK, 2022
- Medical aspects of fitness to drive – a guide for health practitioners Waka Kotahi NZ Transport Agency, NZ, 2014
Heart Foundation, NZ
Heart Foundation, NZ, 2019

Heart Foundation, NZ, 2015
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed:





