You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Heart failure | Manawa ngoikore
Also known as congestive heart failure or heart dysfunction
Key points about heart failure
- Heart failure (manawa ngoikore) is when your body retains fluid because your heart isn't working well.
- It means your heart is struggling, not that it's about to stop.
- Symptoms develop slowly and can be different for different people.
- You might feel tired and less able to exercise, or you might feel short of breath, be unable to lie flat or have swollen ankles.
- Heart failure can be managed so that you have minimal symptoms day-to-day.

Heart failure (manawa ngoikore) is when your heart can’t pump blood properly around your body. It's also known as congestive heart failure.
- Heart failure means your heart’s pumping action is getting weaker. It doesn’t mean your heart is about to stop.
- There are many conditions that can cause heart failure.
- Symptoms develop slowly and can vary. They include shortness of breath, swelling of your ankles, legs or tummy, tiredness and being less able to exercise.
- Symptoms can get worse and become particularly severe during a flare-up (exacerbation).
- Heart failure can't be cured, but there are treatments to help manage it.
- There are many things that you, your whānau and your healthcare team can do to help you feel better and stay well for as long as possible.
See your healthcare provider or go to the nearest emergency department if you or someone you care for has heart failure and experiences the following:
- sudden chest pain that lasts more than a few minutes
- sweating and weakness
- more shortness of breath than usual despite following action plan steps
- feeling very unwell
- dizziness, fainting or blackouts
- fever (a high temperature – above 38°C)
- increased swelling of ankles or abdomen (tummy)
- coughing for no reason.
Your heart is a pump made of muscle. The right side of your heart pumps blood through your lungs to pick up oxygen. The oxygenated blood goes back to the left side of your heart and gets pumped all around your body. Your heartbeat is the feeling of this pumping. Your body uses the oxygen to help provide the energy you need to live.
Your heart has 4 chambers with muscular walls. Blood from all around your body arrives first at your right atrium, the smaller upper chamber on the right side of your heart, which pumps your blood into right ventricle. Your right ventricle pumps blood around your lungs where it picks up oxygen then flows back to your left atrium. Your left atrium pumps blood into your left ventricle, which pumps it out to your body through your aorta. Because it needs to get blood to your whole body, your left ventricle is your strongest chamber. Each time it pumps, between 50 and 70% of the blood inside it is squirted into your aorta. This is called the ejection fraction.
Your aorta is your main artery – from here your blood flows through smaller and smaller arteries, then capillaries in every part of your body where it delivers the oxygen, then flows back through your veins to your right atrium. Then the cycle starts again.
Every minute your heart pumps 4 to 6 litres of blood around your body. When you’re active, your heart beats faster and pumps much more than this each minute.
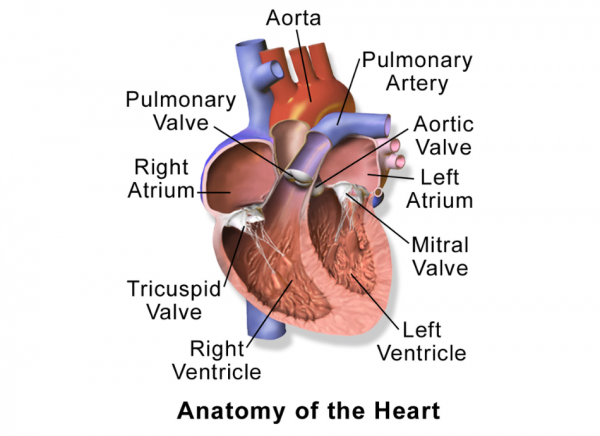
Image credit: Medical gallery of Blausen Medical 2014(external link)
Video: How the heart works
Heart failure
Heart failure (manawa ngoikore) happens when your heart pump struggles to effectively move blood around your body, and this leads to fluid retention. It doesn’t mean your heart is about to stop. Heart failure can happen if your heart muscle gets weak and floppy so it can’t squeeze enough blood out, or stiff or thick so it can’t relax enough between beats to fill with blood. It can happen to 1 chamber of your heart, which can affect the others over time. Or it can affect several chambers or your whole heart at the same time.
You can watch a video about heart failure on the Heart Foundation’s understanding heart failure(external link) page.
Heart dysfunction can get worse over time. Your body makes changes to accommodate it (neurohormonal activation). But as time goes by these changes begin to fail too. Fluid starts to build up in different parts of your body, causing symptoms such as swelling of your ankles and shortness of breath.
2 to 3% of adult New Zealanders are living with heart failure. If you’re over 70 years of age, there’s an even higher chance – 1 in 10 people (10%). Māori and Pacific Peoples are more likely to get heart failure at a younger age.
When to get help
See your healthcare provider or go to the nearest emergency department if you or someone you care for has heart failure and experiences the following:
- Sudden chest pain that lasts more than a few minutes.
- Sudden severe shortness of breath.
- Fainting or blackouts.
Symptoms
Symptoms of heart dysfunction develop slowly and can vary from person to person. Common symptoms are:
- shortness of breath with exercise or when lying flat (this is caused by a build-up of fluid in your lungs)
- waking suddenly at night feeling breathless
- tiredness or fatigue
- feeling breathless when walking or bending over
- weakness
- swollen ankles.
You could also notice:
- swelling (oedema) of your feet, legs or tummy, or of your lower back and scrotum if you sit most of the time
- fast heartbeat
- feeling generally unwell (malaise)
- sudden weight gain, due to fluid build-up
- cough at night time
- wheezing – even if you don't have asthma
- loss of appetite
- shortness of breath when bending over
- bloating
- dizziness
- low mood
- fainting
- confusion – especially for older adults.
Many conditions can cause heart failure. Most of them are conditions that affect your heart.
Heart conditions that can cause heart failure
- Coronary artery disease is the most common cause of heart failure. Coronary artery disease describes the blockage of the blood vessels that supply your heart. It includes heart attack (when the blockage happens suddenly) or angina (chest pain due to reduced blood flow to your heart muscles). Coronary artery disease can cause scarring of your heart muscles and weaken your heart’s pumping action.
- High blood pressure (hypertension) can put extra strain on your heart as your heart needs to pump harder. Over time, your heart muscles can be damaged.
- Cardiomyopathy is a disease of the heart muscle itself. It can be caused by:
- some viral infections
- drinking too much alcohol
- methamphetamine
- genetic conditions
- chemotherapy
- diabetes.
- Heart rhythm or conduction problems (arrhythmias) such as atrial fibrillation.
- Heart valve disease.
- Congenital heart disease.
- Myocarditis which is inflammation or infection of your heart muscle. This is commonly caused by a virus (including COVID-19) and may lead to heart failure, especially of the left side of your heart.
Other conditions that can cause heart failure
- Anaemia (low red blood cells).
- Overactive thyroid.
- Too much alcohol.
- Thiamine deficiency.
- Methamphetamine or cocaine use.
- Obstructive sleep apnoea.
- Chronic obstructive pulmonary disease (COPD).
- Being very overweight, especially carrying extra weight around your middle.
Common medicines that can contribute to heart failure
- Non-steroidal anti-inflammatories, eg, ibuprofen, diclofenac.
- Corticosteroids, eg, prednisone.
- Antidepressants, eg, nortriptyline, citalopram, venlafaxine.
- Urinary alkalinising sachets for bladder infections (because they are high in salt).
- Calcium channel blockers, eg, diltiazem.
Sometimes a cause can't be found.
A flare-up, or exacerbation, is when your heart failure symptoms suddenly get worse. This is often linked to fluid retention. This might include:
- increased shortness of breath
- increased swelling of your ankles or tummy
- worsening cough
- confusion
- feeling generally unwell.
Each flare-up can make your heart weaker. It's important to be prepared and know how to recognise the symptoms of a flare-up and what to do when they happen.
What are the causes of a flare-up?
A heart failure flare-up means you're retaining more fluids in your body, such as in your lungs, ankles or tummy. Fluid retention is prevented by heart medications which block your body's hormone response to heart dysfunction. A flare-up can be caused by:
- not taking your heart failure medicines or starting a new medicine that interferes with how your heart failure medicines work
- an infection, eg, pneumonia or cellulitis
- high blood pressure
- a heart attack
- a new heart rhythm problem (arrhythmia), eg, atrial fibrillation
- anaemia
- an overactive thyroid
- sleep apnoea
- cardiomyopathy
- too much fluid and salt intake.
Any other issue that makes your heart work harder can cause a flare-up. Sometimes a cause isn’t found.
Exacerbations of heart failure are managed according to your heart failure action plan, see the self-care section below.
If flare ups are recognised and treated early, it can mean you don't need to be treated in hospital. Usually the treatment involves taking a diuretic (water tablet) such as furosemide or bumetanide to remove the excess fluid from your body. If diuretics aren't working to remove the excess fluid, you may need to go to hospital. Hospital treatments can include:
- an intravenous diuretic (through a line in your hand)
- oxygen
- investigation and treatment of any cause of your exacerbation, such as blood tests, chest X-ray and antibiotics for pneumonia/infection.
Your healthcare provider will ask you questions about your symptoms and your past medical history. They will also examine you, including checking your weight, pulse and blood pressure, and listening to your heart and lungs.
Some tests can be done to help diagnose heart failure and what might be causing it. These include:
- Blood tests such to check electrolytes, kidney function, thyroid function, and a full blood count,
- A brain natriuretic peptide (BNP) blood test. This is a hormone made by stressed heart muscle cells. A normal BNP test result for your age means you're very unlikely to have heart failure.
- An electrocardiogram (ECG) to check the electrical activity of your heart and to look for signs of coronary artery disease or a heart rhythm that can cause heart failure.
If the diagnosis isn't clear, or your healthcare provider thinks there could be a different reason for your symptoms, you may need:
- a chest X-ray
- breathing tests such as spirometry.
If your healthcare provider thinks you do have heart failure, they will usually refer you for a heart ultrasound scan – an echocardiogram (echo). It shows how each part of your heart is functioning, and how much blood is being pumped with each beat (your ejection fraction).
There are different kinds of heart failure, depending on whether your heart is having trouble pumping blood out or relaxing to fill back up with blood. Your echocardiogram will show which type you have.
Heart failure with reduced ejection fraction (HFrEF) means that your left ventricle is pumping out (ejecting) less than 40% of the blood inside each time it beats. This is what happens with a weak, enlarged, floppy heart. The most common cause of this type of heart failure is coronary artery disease (heart attacks), which is more common in men.
Heart failure with preserved ejection fraction (HFpEF) means that your left ventricle pumps out 50% or more of the blood in it with each beat. This is what happens with a stiff or thickened heart. Because your heart has not relaxed between beats, it doesn’t fill with blood properly, so there is less blood to be pumped for the next heartbeat. It’s also called diastolic dysfunction.
This type of heart failure is more common in women. You may first notice symptoms at menopause. Pregnancy complications and emotional, physical or sexual harm in the past make HFpEF more likely.
There can be a long wait for an echocardiogram in the public health system, but treatment starts straight away. If you’re not going to have an echocardiogram, or while you are waiting, you will be treated for HFrEF.
You can improve your symptoms through self-management and monitoring. It can also help to involve your whānau.
There are 5 pillars of heart health and these can be applied across all heart conditions.
1. Overall wellbeing
You might have lots of different feelings while coping with your diagnosis and symptoms, such as fear, denial, anxiety, or depression.
You can improve your mood and wellbeing by:
- getting plenty of rest and setting yourself up for a good night's sleep, as this allows your body and mind to restore
- moving your body each day
- doing meaningful activities – feeling useful and finding a sense of achievement can help you regain balance in your life
- planning time to relax
- developing healthy relationships at home, at work and in your community – can help you feel connected to your community and can provide extra motivation to keep on track with other lifestyle measures
- joining a support group
- making an appointment with a counsellor.
2. Good sleep
Sleep is an important part of a healthy lifestyle. Get a good bedtime routine and try to be consistent each night. Avoiding digital devices/screens, evening time caffeine and alcohol is important for good quality sleep. If you're struggling to sleep or think you may snore or suffer from sleep apnoea, talk with your healthcare provider or health coach. Read more about sleep.
3. Eat foods that nourish your body
This includes whole grains, fruit and vegetables and eating less processed foods. A healthy diet can help you manage your heart failure and other health issues you may have. Read more about healthy eating. Processed foods contain high amounts of salt which leads your body to hold on to more fluid. Read more about salt and specifically how to eat less of it.
4. Move every day
Start moving more by doing a little and then slowly increasing your activity as you manage more. Try walking gently around the house or down the road for 5 to 10 minutes at first. Gradually build up to 30 minutes of activity on most days of the week. The best exercise is the one you enjoy. Ask your healthcare provider about suitable exercises for you or about any exercise programmes available in your area. Read more about how to start exercising if you’re out of shape.
5. Avoid things that aren’t good for your heart.
Smoking, alcohol and some drugs including methamphetamine damage your heart. If you need support to quit or want to talk to someone about this, read more about quitting smoking and alcohol and drug support.
Other things you can do to care for yourself
Aim for a healthy body weight
If you're underweight or have a poor appetite, having foods or drinks that are higher in energy and protein can help boost your energy. If you're overweight, weight loss can help you feel less breathless. However, weight loss can be difficult to achieve and maintain. Repeated weight loss dieting can reduce your wellbeing and cause weight gain in the long term. Your goal may be maintaining your current weight, or paying attention to good nutrition rather than weight. Ask your doctor, nurse or dietitian for advice on weight.
Check your weight and symptoms each day
Most of the symptoms of heart failure happen when your body is retaining (holding on to) extra fluid. If you put on more than 1 to 2 kg over a few days, your body is retaining fluid, not fat. Your healthcare provider will help you work out your target weight – this is your weight with no extra fluid and is the weight at which your body and heart work best.
- Use the 5 W’s – Wee, Weigh, Write it down, Where is the fluid hiding, What to do?
Weigh yourself every morning after you've been to the toilet, before you eat or drink anything and before you get dressed. Use digital scales, on a firm surface, eg, lino or tiles. Record your weight and remember to bring it with you to every appointment with your healthcare team.
You also need to check for swelling. Check whether your rings, waistband, socks or shoes feel tighter. Press firmly into the skin of your ankle, shin and knee with your thumb for 5 to 10 seconds. If your thumb makes a dent that doesn’t quickly fill, you have swelling.
Monitor any changes in your breathing. Are you are more short of breath than usual, having trouble speaking or lying flat. Do you cough at night or need extra pillows?
Record your weight, any swelling or breathing changes in a paper daily checks record(external link) or app and use this to follow your heart failure action plan.
Have a heart failure action plan
A heart failure action plan provides you with instructions and information on how to manage your heart failure and how to recognise and cope with worsening symptoms, such as flare-ups (exacerbations).
You can develop your heart failure action plan with your healthcare provider and adapt it to suit you and how severe your heart failure is. At each visit with your healthcare provider, you can review the plan and make adjustments as needed.
Here's an example of a heart failure action plan(external link) by the Heart Foundation NZ.

Build a health care team
Managing heart failure well needs the input of your GP or nurse practitioner who knows about your other health issues that may affect your heart failure. Other healthcare team members who may be involved in your care include a heart specialist, heart failure nurse, dietitian and pharmacist.
It’s important to attend your follow-up appointments regularly. This allows your healthcare provider to monitor your health and see how your condition is progressing, as well as review your medicines and answer any questions you may have. Bring your heart failure action plan with you so that your healthcare provider can monitor and better understand what is happening for you.
Join a cardiac rehabilitation programme
You may be advised to attend a cardiac rehabilitation group at your local hospital. These are excellent for learning more about ways you can help your heart and supporting you to get more active. Some local gyms also have exercise classes for people with heart failure. Read more about cardiac rehabilitation.
Get vaccinated
Vaccination against COVID-19, the flu and pneumococcal disease (not funded) is recommended as these infections can make your symptoms worse. Ask your healthcare provider about getting these vaccinations.
Apps reviewed by Healthify
You may find it useful to look at some heart failure apps, heart rate apps, first aid and emergency apps, quit smoking apps, alcohol use apps, depression apps, anxiety apps, self-management apps and nutrition, exercise and weight management apps.
Heart failure can’t be cured, but there are treatments available to manage your condition.
Treatments for heart failure include:
- medicines
- devices for heart failure
- surgery.
Medicines
Medicines for heart failure with reduced ejection fraction (HErEF)
These medicines improve your symptoms, prevent fluid retention and lengthen your life if you take them every day. You should expect to take multiple medicines for the rest of your life. Some tablets cause side effects, but often these are not as severe as heart failure symptoms.
Many of the medicines start with a small dose and are built up step by step, depending on whether you have any side effects. If you get side effects, talk to your healthcare provider before stopping. It can take a while to find the right dose and combination for you.
The 'fab four' for improving heart function
- Beta blockers help with your heart's pumping action by slowing your heart rate and reducing your blood pressure. Examples include bisoprolol and metoprolol.
- Spironolactone and Eplerenone have a diuretic effect (make you pee out extra fluid).
- Empagliflozin makes you pee out extra fluid and reduces your blood pressure. It also lowers your blood glucose if you have diabetes, and helps protect your kidney function for longer.
- Sacubitril with valsartan (Entresto) – this medicine includes a combination of an angiotensin-II receptor antagonist (valsartan) and a neprilysin inhibitor (sacubitril). Sacubitril causes you to pee out water and salt, and relaxes your blood vessels. It acts like a diuretic (water tablet) once you're on a higher dose.
You may not need Sacubitril with valsartan and can be managed on:
- ACE (angiotensin-converting enzyme) inhibitors – ACE inhibitors relax your blood vessels, making it easier for your heart to pump blood around your body. This should also allow you to do more without becoming quite so breathless or tired. Examples include enalapril, lisinopril, quinapril, perindopril, ramipril.
- Angiotensin-II receptor antagonists – these medicines are an alternative if you have difficulty tolerating ACE inhibitors. Examples include losartan and candesartan.
If you have a flare-up (increased weight with symptoms) you may need:
- Diuretics (water pills) – these medicines encourage your kidneys to remove excess fluid and salt from your body by increasing the amount of urine (pee) you produce. Examples include furosemide and bumetanide.
If you also have atrial fibrillation, or if you still have symptoms with all the other medicines above you might need:
- Digoxin which helps your heart beats strongly and regularly.
Medicines used for heart failure with preserved ejection fraction
Because your heart muscle is stiff or thickened with this type of heart failure, medicines are used differently. If you have underlying conditions such as high blood pressure, atrial fibrillation or diabetes those problems will be treated, probably with the same medicines as for HFrEF. But if you don’t, some medicines won’t make a difference to your heart failure itself, so it may not help to take them.
If you're retaining fluid, you’ll need a diuretic such as furosemide or bumetanide.
Your healthcare provider will let you know which medicines are suitable for you.
Devices for heart failure
Devices such as a pacemaker or an implantable cardioverter defibrillator (ICD) which can give cardiac resynchronisation therapy (CRT) help manage heart failure for some people but are not suitable for everyone. Your healthcare team will let you know if these devices would help you.
Surgery
For some people with heart failure, an operation or cardiac procedure may help. The type depends on what's causing your heart failure. Your healthcare provider will let you know whether surgery may help in your situation.
Treatment for advanced heart failure
Although treatment helps to control symptoms, other health conditions can impact on treatment or treatments can become less effective. Heart conditions also get worse over time. The approach may need to move towards supporting you with symptoms rather than trying to improve your heart function. Read more about advanced heart failure.
The New Zealand Heart Foundation(external link) provides resources and support for people living with a heart condition. You can contact them using their online form(external link) or visit their website(external link).
They provide a range of resources including:
- Supporting someone with heart failure(external link) Heart Foundation, NZ
- Heart failure resource pack(external link) Heart Foundation, NZ
You can contact the Heart Foundation's Heart Line on 0800 863 375. This phone line is managed by a consumer care representative who can support you with heart health information, health service navigation and access to resources and support.
Heart attack | Hē manawa
Heart disease tests
High blood pressure | Mate pēhanga toto
Advanced heart failure
Goal setting and making changes
Healthcare provider visits - how to make the most of your appointment
The following links provide further information about heart failure. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Heart failure(external link) Heart Foundation, NZ
Staying well with heart failure(external link) Heart Foundation, NZ
The management of chronic and acute heart failure – what patients need to know(external link) European Society of Cardiology
Heart failure matters(external link) is the European Society of Cardiology patient website. It has an animated journey through heart failure, a symptom diary and monitoring chart, animations of how medicines work, and patient and caregiver videos. Available in 10 languages.
Book
Hope for the best, plan for the rest: 7 Keys for Navigating a Life-Changing Diagnosis. Sammy Winemaker and Heoin Seow, Page Two Books, 2023.
Brochures
Staying well with heart failure(external link) Heart Foundation, NZ, 2019
Heart failure – daily checks record(external link) Heart Foundation, NZ, 2019
My heart failure action plan(external link) Heart Foundation, NZ
Heart failure – what you need to know(external link) NPS MedicineWise and Heart Foundation, Australia
Heart failure – more than just your heart(external link) action plan NPS MedicineWise and Heart Foundation, Australia
Apps
Heart failure apps
Heart rate apps
First aid and emergency apps
Self-management apps
Nutrition, exercise and weight management apps
References
- Heart failure(external link) Auckland Regional HealthPathways, NZ, 2024
- Managing exacerbations of heart failure(external link) Auckland Regional HealthPathways, NZ, 2023
- Heart failure diagnosis and investigation(external link) Patient Info, UK
- Acute exacerbation of congestive heart failure(external link) The BMJ, UK, 2020
- Addressing heart failure in primary care: Part 1 – identifying and diagnosing heart failure(external link) BPAC, NZ, 2025
- Addressing heart failure in primary care: Part 2 – initiating and optimising treatment(external link) BPAC, NZ, 2025
- Bombak A, Monaghan LF, Rich E. Dietary approaches to weight-loss, Health At Every Size® and beyond – rethinking the war on obesity(external link) Soc Theory Health 2019;17:89–108
See our page Heart failure for healthcare providers
Brochures
Heart Foundation, NZ, 2019
Heart Foundation, NZ, 2019

Heart Foundation, NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Tammy Pegg, Cardiologist, Nelson
Last reviewed:





