If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Statins
Key points about statins
- Statins are medicines used to lower cholesterol and reduce the risk of heart disease and stroke.
- In Aotearoa New Zealand, available statins are atorvastatin, pravastatin, rosuvastatin and simvastatin.
- Find out more about statins including the benefits and risks of taking them.

Statins are medicines that help lower your cholesterol and protect your arteries. They work by blocking the action of an enzyme in your body needed to make cholesterol.
Taking statins has many benefits
Statins do more than lower cholesterol. They help protect your heart and brain and reduce the risk of heart attack and stroke.
- In people with high cholesterol: Statins help lower cholesterol levels. High cholesterol increases the risk of diseases that affect the heart and blood vessels called cardiovascular disease. Examples of cardiovascular disease include coronary heart disease, angina (chest pain or discomfort), heart attack, and stroke.
- In people with normal cholesterol: Statins may also be used in people with normal cholesterol who have a higher overall risk of heart disease or stroke because they have other risk factors such as diabetes or high blood pressure. They reduce the risk of future heart problems, such as heart attacks.
- After a heart attack or stroke: If you’ve had a heart attack or stroke, your arteries are damaged and narrowed, and you’re at high risk of having another. Statins lower your cholesterol and stabilise plaques to prevent more blockages.
See below for more information about when statins are used.
Statins available in Aotearoa New Zealand
In Aotearoa New Zealand, the following statins are available:
- Atorvastatin (Lorstat®).
- Pravastatin (Clinect®).
- Rosuvastatin (Crestor®, Viatris®).
- Simvastatin (Mylan/Viatris®).
Most people are prescribed atorvastatin. However, for some people, another statin may be a better option. Rosuvastatin is funded under a Special Authority, for people who meet the criteria. A special authority means your healthcare provider will need to make an application to Pharmac (the government medicine funding agency) for approval before the medicine can be funded for you.
Statins: What you need to know
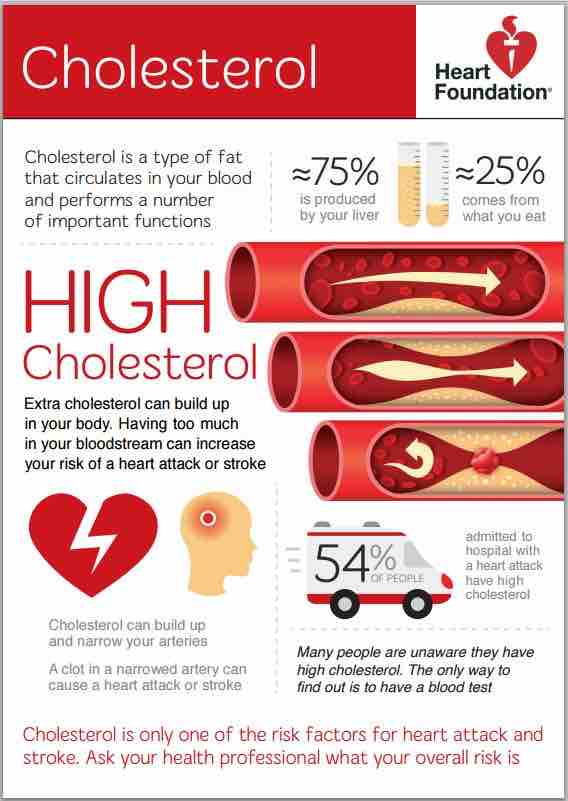
Cholesterol is a type of lipid made by your liver and from the fatty foods that you eat. Everyone has cholesterol and triglycerides in their blood which are needed for hormone production and brain function. Your body needs some cholesterol but if the amount in your blood gets too high, it can cause small fatty patches called plaques (or atheroma) to form. Over time, these patches can build up and make the blood vessels narrow and stiff (a process called atherosclerosis). The narrowing reduces the blood flow through your arteries and can cause heart attack, angina and stroke. Learn more: What is cholesterol.
If you have high cholesterol
Statins lower high cholesterol and help to reduce atherosclerosis which increases your risk of cardiovascular disease and having a heart attack or stroke. Read more about high cholesterol and atherosclerosis.
When deciding whether you should take a statin or not, your healthcare provider will look at your overall risk of having a heart attack or stroke in the future. They work out your individual risk, using information such as your age, sex, ethnicity, blood pressure, whether you smoke and if you have high blood pressure or diabetes. Read more about heart risk assessment
For people with normal cholesterol who are at risk of heart disease and stroke
Statins can reduce your chance of heart disease and stroke, even if your cholesterol levels are normal but your overall risk is high. They are especially recommended for people who already show signs of heart disease, such as angina (chest pain), or who have had a mini-stroke (transient ischemic attack or TIA). This is because fatty plaques may already be present in your arteries, increasing your risk of a heart attack or stroke. Statins help reduce inflammation and stabilise these plaques, lowering your risk of such events.
Your healthcare provider will look at your overall risk of having a heart attack or stroke in the future, using information such as your age, sex, ethnicity, blood pressure, whether you smoke and if you have diabetes. Read more about heart risk assessment.
After a heart attack or stroke
If you’ve had a heart attack or stroke, you're at high risk of having another. Keeping your cholesterol low with the help of statins reduces the buildup of plaque (fatty deposits) in your arteries, helping to prevent further heart attacks or strokes. Some statins such as atorvastatin and rosuvastatin are used at higher doses soon after a heart attack or stroke. Higher doses of these statins reduces the fat content of plaques and stabilises them, making them less likely to rupture (break open) and cause another event.
- Lowers cholesterol levels.
- Slows the buildup of plaque (fatty deposits) in arteries.
- Reduces the risk of heart attacks.
- Helps to prevent strokes.
Statins reduce cardiovascular risk by reducing LDL cholesterol (often called bad cholesterol).
- For people who have high LDL cholesterol level (≥4 mmol/L), statins can reduce LDL cholesterol by more than half.
- Reducing LDL cholesterol can help to reduce heart attacks and strokes.
- Every 1 mmol/L decrease in LDL cholesterol reduces major vascular events by approximately 25% and fatal heart attack or stroke by 20%.
Most people have few, if any, side effects from statins. The most common side effects are tummy upset such as indigestion, bloating, flatulence (wind), headache, and stuffy nose.
Muscle pain or weakness
Some people will have muscle aches and pains when taking statins. It's difficult to know if these are caused by the statin, since aches and pains tends to become more common if you're over 50 years of age. This side effect is rarely serious and often goes away with time. If your pain starts soon after you start your statin, or gets worse, see your healthcare provider. They'll check an enzyme called creatine kinase to see if the aches and pains are caused by or made worse by the statins.
If so:
- a lower dose or a different statin may be prescribed, or
- you may choose to manage the aches because of the benefits of the statin, or
- you may discuss stopping taking your statin with your healthcare provider.
Your healthcare provider will also want to check for a rare but serious condition called rhabdomyolysis (muscle inflammation and damage). They'll check any other medicines you're taking. Rhabdomyolysis can be caused by an interaction between statins and some other medicines including antibiotics.
Increased risk of type 2 diabetes
There's a small chance that statins may increase your risk of getting type 2 diabetes. However, it's usually recommended that people at risk of diabetes do take statins if they're needed to help lower their cholesterol. This is because the benefit of taking statins and preventing a heart attack or stroke is greater than the consequences of developing diabetes.
Memory loss
There are reports that statins may affect cognitive function, mainly memory loss and confusion, and affect sleep and mood but these haven't been fully proven.
The benefits and risks of taking a statin will be different for each person depending on their heart risk assessment. They can change over time as your health and heart risk change.
Your healthcare provider will discuss your cardiovascular risk with you, any possible side effects and how these could affect you.
If you’re considering starting a statin or are already taking one, it’s important to understand how it may affect your health and what choices you have if you’re unsure about continuing treatment. Asking your healthcare provider questions can help you make an informed choice, such as:
- How much will this statin reduce my risk of a heart attack or stroke?
- Are there other ways to lower my cholesterol?
- What are the possible side effects of this statin?
- Are there any foods, drinks or medicines I should avoid while taking a statin?
- Will I need to take it for the rest of my life?
- What should I do if I experience side effects?
- What are my options if I decide to stop taking a statin?
Yes, most people will need to keep taking their statin. The benefits of reducing your risk of having a stroke or heart attack will only continue for as long as you take it. If you stop taking the statin without starting a different cholesterol-lowering treatment, your cholesterol level may rise again.
Eating a healthy diet, exercising regularly and having no more than 1 alcoholic drink a day have all been shown to improve your cholesterol levels. It's best to eat a low-fat diet and reduce the amount of saturated fat you eat.
Read more about ways to reduce your cholesterol.
In Aotearoa New Zealand, atorvastatin is the preferred statin and is most widely used.
Some statins, such as rosuvastatin, are only available for some people if other statins haven’t worked well or if you’re of Māori or Pasifika ethnicity and are at risk of heart disease.
The choice and dose of statin will depend on your heart risk assessment or cardiovascular disease (CVD) risk – people with a lower cardiovascular risk will be on lower intensity treatments and doses than people at higher risk.
Your healthcare provider will discuss your CVD risk with you. Read more about heart risk assessment(external link).
Depending on your body’s response to the statin your healthcare provider may increase your dose or change your treatment if you develop any side effects that bother you.
High cholesterol doesn’t have any symptoms so you won’t notice any changes after taking statins. That's why it’s important to have a blood test to check the changes in your cholesterol levels.
Most people don't feel any different or notice any side effects after starting a statin. Some people may feel muscle aches and pains in the first 6 months.
In rare cases, statins can cause serious problems with your muscles and liver. Tell your healthcare provider immediately if you have signs of problems with your muscles and liver such as muscle pain, muscle tenderness or weakness, dark coloured urine, yellowing of the skin or eyes or a sharp pain in your stomach area.
In general the best time to take a statin is at a time that suits you so that you remember to take it. It's best to take it at about the same time each day.
Some people may recommend that simvastatin and pravastatin are best taken in the evening, but there is little difference in effect.
Many people worry about eating grapefruit or drinking grapefruit juice when they take statin medicines.
This is mostly a concern if you take simvastatin. Eating or drinking large amounts of grapefruit can cause more side effects because grapefruit blocks an enzyme in your liver that helps break down simvastatin. This leads to higher levels of the medicine in your body and increases the risk of problems. But limiting the amount you consume to half a grapefruit, one serving of marmalade, or one glass (250 mL) of grapefruit juice each day is usually safe. It’s best to wait at least 12 hours between eating or drinking grapefruit and taking your simvastatin.
If you take atorvastatin, drinking a lot of grapefruit juice (more than 1.2 liters) might cause side effects, so you should try to limit how much you drink.
If you take pravastatin or rosuvastatin, grapefruit and grapefruit juice are safe and won’t cause problems with your medicine.
You’ll need a blood test to check that your blood cholesterol level has come down. After starting a statin, it takes about 6 weeks for cholesterol levels to stabilise, so most healthcare providers would re-check your cholesterol after a few months. Read more about cholesterol testing.
Do I need to take coenzyme Q10 with a statin?
Statins lower the level of an enzyme in your body called coenzyme Q10, but the effect of this is unknown. Studies have tested coenzyme Q10 supplements to prevent muscle problems from statins but they mostly haven't been shown to be helpful.
Statins shouldn't be taken if you're pregnant because they can affect development of the foetus. If you do become pregnant while taking statins, contact your healthcare provider for advice.
There's no evidence on whether it's safe to breastfeed while taking statins – talk to your healthcare provider if you're breastfeeding or planning to.
If you’re taking a statin and aren’t sure if you want to keep taking it, or if you’re feeling unwell, talk to your healthcare provider. They can explain the risks of stopping, lowering, or changing your medicine.
You can ask them about:
- Trying a different statin.
- Changing your statin dose.
- Other medicines to lower your cholesterol.
- Treatments to help with side effects.
- Changing your diet and lifestyle to lower cholesterol.
Talking with your healthcare provider and getting all the information can help you decide what’s best for you.
Statins(external link) Heart Foundation, NZ
Brochures
Cholesterol – what your lipid test means for you(external link) BPAC, NZ
The pros and cons of taking statins(external link) Medsafe, NZ
Cholesterol(external link) Heart Foundation, NZ English, (external link)Chinese, (external link)Hindi(external link), Korean(external link), te reo Māori(external link), Samoan(external link), Tongan(external link)
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ English(external link), te reo Māori(external link)(external link)
References
- Statins(external link) New Zealand Formulary, NZ, 2024
- Cardiovascular disease risk assessment in primary care – managing lipids(external link) BPAC, NZ, 2018
- Prescribing statins to reduce cardiovascular risk(external link) BPAC, NZ, 2021
- Rosuvastatin – another option to lower cardiovascular disease risk BPAC, NZ, 2022
Brochures
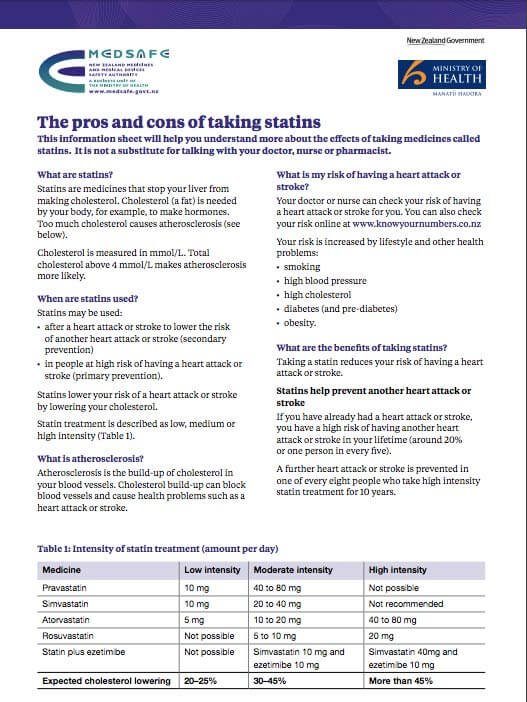
Medsafe, NZ, 2022
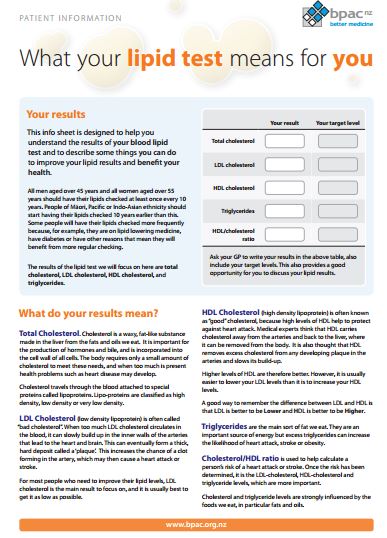
BPAC, NZ, 2012
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed: