You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Clopidogrel
Sounds like 'klop-id-oh-grel'
Key points about clopidogrel
- Clopidogrel is an antiplatelet medicine.
- It prevents your blood from forming clots to lower your chance of having a heart attack or stroke.
- Find out how to take it safely and possible side effects.

Clopidogrel is an anti-platelet medication. It’s used to prevent your blood from forming clots by making it less sticky.
Preventing clots in blood vessels that lead to your brain and heart muscle helps to lower your risk of having a stroke and heart attack.
Clopidogrel is used to prevent blood clots in people who have:
- chest pain (from angina)
- had a stroke or mini stroke (TIA, transient ischemic attack)
- had a heart attack (myocardial infarction) and had a coronary stent fitted
- had ‘bypass surgery’ – after CABG (coronary artery bypass graft)
- peripheral vascular/arterial disease (with a stent fitted).
Use with aspirin or anticoagulants
Depending on what it's being used for and your risk of blood clots, your healthcare provider may prescribe clopidogrel with low dose aspirin OR in combination with anticoagulant medicines such as dabigatran, rivaroxaban or warfarin. Read more about antiplatelets and when they are used.
In rare situations, clopidogrel may be used with low dose aspirin and an anticoagulant medicine.
- These medicines taken together can be very effective in preventing blood clots. But, there’s a higher risk of bleeding. This risk increases with age. See below for signs of severe bleeding.
- Depending on the combination of treatment you are prescribed, you may take it for a few weeks or months. After this, your specialist will tell you which medicines to stop.
- It’s important to check with your healthcare provider which of these medicines you need to stop and when.
Clopidogrel may not work for everyone
When you take clopidogrel, it must be activated in your liver via the CYP2C19 enzyme before it can work. This doesn't work as well as expected for some people because of genetic differences (even if they have a healthy liver). These people will be at higher risk of another stroke or heart attack.
Pharmacogenomic testing can tell you if you have a genetic difference in CYP2C19 which makes you less able to activate clopidogrel. You might need a higher dose of clopidogrel or another medicine to prevent blood clots. Read more about how your genes affect the way you respond to some medicines (pharmacogenomics). Remember, don't stop taking your medicines or make any changes to them, without talking to your healthcare provider first.
In Aotearoa New Zealand clopidogrel is available as 75 mg tablets. It’s also called Arrow-Clopid® or Clopidogrel Multichem®.
- Always take your clopidogrel exactly as your healthcare provider has told you. The pharmacy label on your medicine will tell you how much clopidogrel to take, how often to take it, and any special instructions.
- The usual dose of clopidogrel is 1 tablet once a day.
- You may be given a starting dose of 4 tablets (300 mg) or more the first time you take it.
- Timing: Take clopidogrel once a day, at the same time each day. Swallow your tablet with a glass of water.
- Food: You can take clopidogrel with or without food.
- Missed dose: If you miss a dose, take it as soon as you remember. If it’s less than 12 hours until your next dose, wait until the next day and take your dose at the usual time. Don’t take double the dose.
Here are some things to know when you're taking clopidogrel. Other things may be important as well, so ask your healthcare provider what you should know about.
- Other medicines:
- Clopidogrel interacts with some medicines, especially anti-inflammatories such as diclofenac (eg, Voltaren®) and ibuprofen (eg, Nurofen®). These can also be found in some cold and flu medicines (eg, Nurofen Cold and Flu®). Taking these together with clopidogrel may increase your risk of bleeding and should be avoided.
-
Clopidogrel may also interact with herbal supplements (eg, St John’s Wort, garlic, gingko or ginseng) and rongoā Māori. Check with your healthcare provider before starting clopidogrel and before starting any new products.
- Grapefruit, grapefruit juice or sour/Seville oranges: Avoid grapefruit, grapefruit juice or foods containing grapefruit while taking clopidogrel. It can increase your chance of side effects. Read more about grapefruit and medicines(external link).
- Keep taking clopidogrel regularly: You may just need to take it for a short time, but may take it long-term. Your prescriber will advise you about how long to take it for. Speak to your doctor or nurse before stopping it.
- Surgical procedures including dental work: It's important to let healthcare providers know that you're taking clopidogrel. You may need to stop taking clopidogrel for several days before having surgery.
- Pregnancy or breastfeeding: Talk to your healthcare provider if you're pregnant, planning a pregnancy or want to breastfeed.
Like all medicines, clopidogrel can cause side effects, although not everyone gets them.
Common side effects include diarrhoea (runny poo), stomach pain and indigestion or heartburn. These usually go away with time. Tell your doctor if they bother you.
You might bleed or bruise more easily while you're taking clopidogrel, especially with other anticoagulants or aspirin
- Be careful when shaving, clipping fingernails, brushing and flossing your teeth, or playing sports.
- Avoid new tattoos and piercings as these can cause bruising and bleeding.
- If you have a fall or hurt your head or body, get medical attention immediately, even if you feel okay.
- Some types of bleeding are more serious than others. If bleeding concerns you, is heavier than usual or takes an unusually long time to stop, you should talk to your healthcare provider quickly.
The following links has more information on clopidogrel:
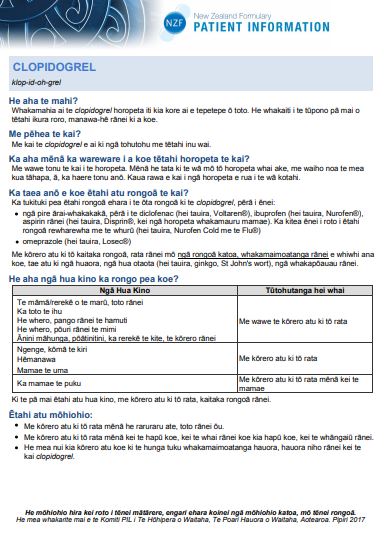
Clopidogrel(external link) New Zealand Formulary Patient Information te reo Māori(external link)
Arrow-Clopid®(external link) Medsafe Consumer Medicine Information, NZ
Brochures
Clopidogrel in te reo Māori(external link) My Medicines, NZ, 2017
Medicines and side effects(external link) Healthify He Puna Waiora, NZ, 2024
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
Apps
References
- Clopidogrel(external link) New Zealand Formulary, NZ
- Arrow-Clopid(external link) Medsafe datasheet, NZ
- Managing patients taking anticoagulants and antiplatelets prior to minor procedures and surgery(external link) BPAC, NZ, 2018
- Ziser K, Rahman S, Soro R, et al. The role of triple antithrombotic therapy in patients with atrial fibrillation and coronary stent insertion(external link) Aust Prescr. 2025;48:18–22
Brochures
My Medicines, NZ, 2017

Medicines and side effects
Healthify He Puna Waiora, NZ, 2024

Health Quality and Safety Commission, NZ, 2019
English(external link)Te reo Māori(external link)
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Johanna Lim, Clinical Pharmacist – Cardiology Expert, Health New Zealand | Te Whatu Ora Te Matau a Māui Hawke’s Bay; Angela Lambie, Pharmacist, Auckland; Stephanie Yee, Pharmacist, Auckland
Last reviewed:
Page last updated:





