You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Atherosclerosis
Also known as arteriosclerosis
Key points about atherosclerosis
- Atherosclerosis is the disease process of hardening of the arteries.
- Fatty deposits build up over time in the walls of the arteries, forming lumps (atheroma) which extend into the artery and reduce the blood flow.
- Atherosclerosis increases the risk of conditions such as coronary heart disease, angina, stroke and heart attack.
- Treatment includes medication and medical procedures, such as angioplasty or heart surgery, in combination with lifestyle changes.
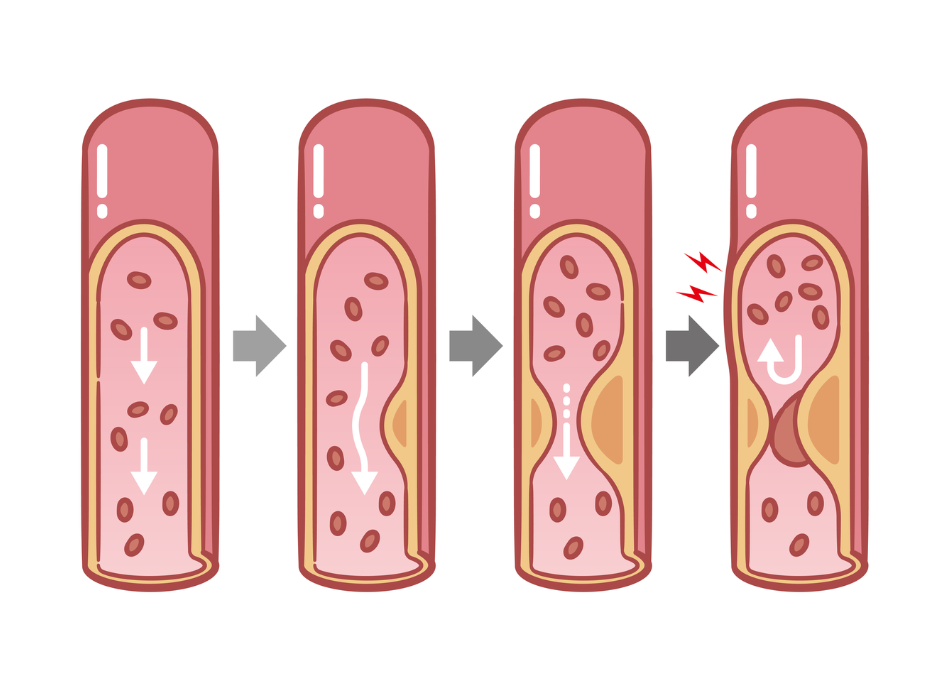
Atherosclerosis is the term used for hardening of your arteries, the blood vessels carrying blood from your heart around your body. They’re lined with a layer of cells called the endothelium. When we're born, our blood vessels are flexible and elastic, and the blood is able to flow through them with ease. As we age, fatty deposits start to develop in the walls of our arteries and gradually they build up, forming lumps called plaques which extend into the middle of the artery, reducing the ease of blood flow through the artery. This process can be broken down into 3 stages:
- Fatty streaks – damage to the inner wall of the artery allows infiltration of fatty substances. At this stage artery damage is minimal and the blood flow isn't seriously affected.
- Soft plaque – deposits of cholesterol, fatty substances, connective tissue and blood products build up, forming a soft bulging lump under a thin cover. The soft lump can partly narrow the artery but also raises the risk of sudden blood clots if its thin cover tears open – even if the narrowing isn’t severe yet. This bulges into the channel of the artery, restricting the flow of blood.
- Hard plaque – calcium deposits stiffen parts of the artery wall, making the blood channel narrower. This can lead to symptoms such as chest pain or leg cramps from poor circulation.

Image credit: Depositphotos
This process can affect any organ. Atherosclerosis of the arteries:
- going to the brain can lead to a stroke
- can cause peripheral arterial disease or clogging of small arteries going to the legs
- in the heart can lead to angina or a heart attack.
If the plaques break open they can form a blood clot called a thrombus which can limit the width of the artery or even block it completely. Read more about thrombosis below.
Atherosclerosis can happen as you get older, and it tends to affect men at an earlier age than women. It may be due to the genes you inherited from your parents – your family history. However, some health conditions and the way you live can increase your risk of developing atherosclerosis.
Health conditions that increase the risk
- High blood pressure – if your blood pressure is high it puts extra strain on your artery walls and over time can damage them and allow fatty deposits (plaque) to build up.
- Diabetes – high levels of glucose in your blood can damage the lining of your arteries making it more likely that plaque will build up.
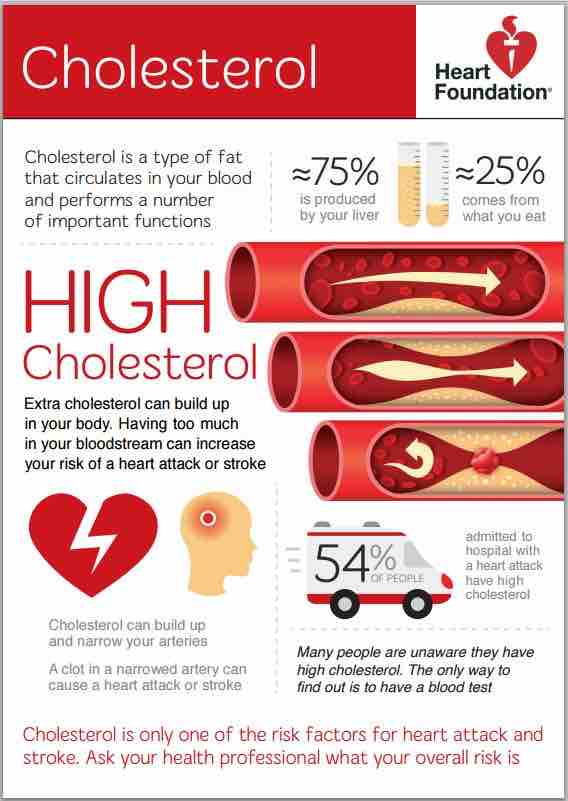
- High cholesterol – the plaque is made up of fat, cholesterol, calcium and inflammatory cells so if the cholesterol levels in your blood are high, it can contribute to the build-up of plaque in the artery walls.
- Inflammatory conditions – conditions such as rheumatoid arthritis or psoriasis can affect your blood vessels leading to plaque build-up.
Lifestyle factors
Lifestyle factors can lead to the health conditions above, or directly harm your arteries, increasing atherosclerosis risk.
- Being overweight or obese is linked to high blood pressure and high cholesterol, both of which increase your risk of developing atherosclerosis.
- Physical inactivity is also linked to being overweight and can contribute to high blood pressure and cholesterol and developing type 2 diabetes.
- Smoking or being around people who smoke (second-hand smoke) can damage your arteries and increase your risk of atherosclerosis.
- Eating unhealthy foods that are high in saturated fat, salt and sugar can lead to weight problems.
- Stress over time can contribute to narrowing of your blood vessels and can raise your blood pressure.
Read more about high blood pressure and high cholesterol.
Thrombosis is the medical term for a clot, the natural process that stops us bleeding when we injure ourselves. In coronary artery disease a clot forms, not because of an outside injury, but from damage to the inner lining of the artery wall, caused by the fatty build-up (plaque) in the wall of the artery.
Normally the lining of the artery is smooth but when plaque builds up, the walls are no longer smooth and sometimes the protruding plaques crack open. When this happens, platelets (blood cells that help with clotting) stick to these cracks to seal them. Soft and hard plaques can result in thrombus formation but soft plaques are more likely to do so as the cover is soft, thin and more likely to rupture. The clot may limit or block the amount of blood flowing through the artery.
The formation of a clot is one of the main problems in coronary heart disease. It's the cause of most heart attacks.
Because the plaque gradually builds up in arteries you may not have any symptoms until it begins to affect the way the blood is travelling around your body, or you have a heart attack or stroke.
However, there may be warning signs such as:
- feeling tired all the time
- feeling short of breath
- having chest pain
- having discomfort or pain in your arms and legs – especially during exercise
- your heart beating unevenly (arrhythmia)
- cold or painful feet
- changes in skin colour
- swelling.
Other things can cause these sorts of symptoms so if you have any concerns or you haven’t had a heart check recently, talk to your healthcare provider.
Your healthcare provider will examine you and discuss your personal and whānau medical history. Depending on your individual risk factors, they may order tests to identify conditions that increase atherosclerosis risk, visualise your blood vessels directly, or assess whether reduced blood flow has damaged organs.
Tests may include:
- blood tests to measure the cholesterol, and glucose in your blood
- blood pressure checks
- an ECG to detect heart rhythm issues or lack of oxygen from reduced flow
- ultrasound scans to check the structure of your heart or blood vessels affected by flow issues
- a stress test to see how well the blood flows around your heart when it’s working hard
- an angiogram to find and measure any narrowed or blocked arteries
- a CT scan which can show what’s happening in the large arteries of your body.
Treatment includes lifestyle changes, medicines, procedures, and sometimes surgery. Your healthcare team will create a personalised plan with you.
Depending on your personal risk factors and current health, your plan may include goals such as:
- promoting heart-healthy eating
- preventing clots and complications (heart attack/stroke)
- easing symptoms
- slowing plaque build-up, and
- improving blood flow by widening or bypassing blockages.
Medicines can address risk factors for plaque formation and can slow atherosclerosis. Your healthcare provider may prescribe treatments to lower blood pressure or cholesterol, manage blood sugar, and prevent clots. If you have severe blockages or high risk of problems, they may suggest procedures or surgery to help open up your arteries. Treatment might include angioplasty with stents, or bypass surgery, depending on how severe the disease is, where the narrowing is and what your symptoms are.
What you do and eat every day makes a big difference to your risk of atherosclerosis building up in your blood vessels. The key things you can do are the same as for heart health.
- Eat heart healthy foods
- Be smoke free
- Keep physically active
- Have a regular heart risk assessment and know the levels of your weight, blood pressure and cholesterol. Work with your healthcare provider to get them down if they're too high.
- If you know you have atherosclerosis or any cardiovascular disease, ask your healthcare provider for a care plan and review the warning signs you need to know about.

Image credit: Healthify He Puna Waiora
Apps reviewed by Healthify
You may find it useful to look at some nutrition, exercise and weight management apps, quit smoking apps and blood pressure apps.
My heart check(external link) Heart Foundation, NZ
Brochures
Cholesterol(external link) Heart Foundation, NZ, 2019 English(external link), Chinese(external link), Hindi(external link), Korean(external link), te reo Māori(external link), Samoan(external link), Tongan(external link)
Blood pressure information sheet(external link) Heart Foundation, NZ, 2019 English(external link), te reo Māori(external link), Tongan(external link), Chinese (traditional)(external link), Hindi(external link), Korean(external link)
Apps
Nutrition, exercise and weight management apps
Quit smoking apps
Blood pressure apps
References
- Atherosclerosis(external link) National Institute of Heart, Lung and Blood, US, 2024
- Atherosclerosis(external link) NHS, UK, 2023
- Atherosclerosis – explained(external link) Watch, Learn, Live: Interactive Cardiovascular Library – American Heart Association
- Atherosclerosis – causes and risk factors(external link) National Heart, Lung and Blood Institute, US, 2024
- Atherosclerosis(external link) Heart Research Institute, NZ
- Atherosclerotic plaque(external link) Heart Research Institute, NZ
- Thrombosis – symptoms and treatment(external link) Cleveland Clinic, US, 2023
Brochures
Heart Foundation, NZ, 2019
English, Chinese, Hindi, Korean, te reo Māori, Samoan, Tongan

Blood pressure information sheet
Heart Foundation, NZ, 2019
English, te reo Māori, Tongan, Chinese (traditional), Hindi, Korean
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Grace Lee, FRNZCGP and Clinical Educator
Last reviewed:





