You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Coronary artery disease
Also known as coronary heart disease and ischaemic heart disease (IHD)
Key points about coronary artery disease
- Coronary artery disease (CAD) is the most common type of heart disease.
- It occurs when the arteries that supply blood to your heart muscle become blocked.
- CAD can cause chest pain (angina), a heart attack or cardiac arrest.
- CAD and stroke are the number one causes of death and disability in Aotearoa New Zealand.
- There are things you can do to reduce your risk of CAD, such as stopping smoking and keeping your blood pressure and weight in a healthy range.
- When you should start having heart checks depends on your age, ethnicity and other risk factors.

Coronary artery disease (CAD) is the most common type of heart disease. It happens when the arteries that supply blood to your heart muscle (the coronary arteries) become hardened and narrowed causing blockage of your arteries. This reduced blood supply causes damage to the heart muscle, affecting your heart’s ability to work properly.
Gradual blockage of your arteries can result in chest pain called angina, while a sudden or severe blockage can cause a heart attack or cardiac arrest.
Coronary artery disease and stroke are the number one causes of death and disability in Aotearoa New Zealand.
Things such as smoking, high blood pressure and being overweight increase your risk of CAD. Making changes to address these things can reduce your risk.
Narrowing of your coronary arteries can be due to the build up of cholesterol and other material, called plaque, on the inner walls of these arteries. This build-up is called atherosclerosis. As the build up increases, less blood can flow through your arteries. As a result, the heart muscle can't get the blood or oxygen it needs. This can lead to angina (chest pain) or a heart attack.
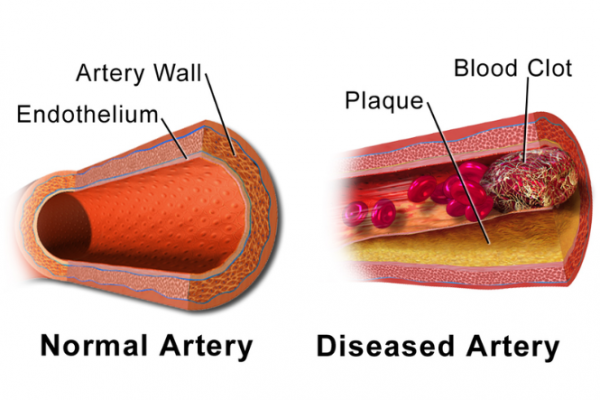
Image credit: Blausen Medical Gallery 2014 via Wikimedia Commons(external link)
Most heart attacks happen when a blood clot suddenly cuts off the blood supply to your heart, causing permanent heart damage. Over time, CAD can also weaken the heart muscle and contribute to heart failure and arrhythmias.
- Heart failure means your heart can't pump blood well to the rest of your body.
- Arrhythmias are changes in the normal beating rhythm of the heart.
The main symptoms of coronary artery disease (CAD) include:
- chest pain or discomfort, which is the main symptom of angina
- breathlessness
- feeling unusually tired.
Some people have no symptoms and only find out they have CAD when they have a heart attack. Read more about the symptoms of angina and heart attack.
If you have chest pain or you’re worried about angina, your healthcare provider will ask about your symptoms and whether you have a personal or family history of heart disease. They’ll examine you and take your blood pressure. They may arrange an ECG and blood tests. Blood tests can be done to check for cardiac enzymes which indicate damage to your heart muscle and identify risk factors such as high cholesterol.
If they think you might have angina your healthcare provider may refer you to hospital for further tests, including an exercise tolerance test (ETT) or coronary angiogram.
If you think you may be having a heart attack: Call 111 immediately and ask for an ambulance. They‘ll do an ECG and when you're in hospital you’ll have further tests.
Read more about what happens if you have angina or a heart attack.
There are a variety of medicines for angina that can ease chest pain or prevent angina symptoms, and stop the progression of heart damage. Medicines are used together with healthy lifestyle choices such as eating a healthy balanced diet, maintaining a healthy weight and exercising regularly.
If you’ve had a heart attack, you'll be given medicine to help you recover. This may include a thrombolytic medication to help break down the clot in your artery. You may need a procedure called an angioplasty to widen a coronary artery and improve blood flow.
Read more about treatment of angina and heart attack.
One in 20 adults have been diagnosed with heart disease. That's more than 165,000 New Zealand adults.
Every 90 minutes a New Zealander dies from heart disease. Many of these deaths are premature (the person dies too early) and could be prevented.
There are a number of factors that are known to increase your risk of CAD. Some risk factors you can’t do anything about, such as your age, ethnicity, gender, and personal or family history of heart attack or stroke.
Other risk factors you can change (see below) and making these changes can have a huge impact on your heart health and general wellbeing.
Your risk of developing CAD is significantly increased if you:
- smoke
- have high blood pressure (hypertension)
- have a high blood cholesterol level
- don't exercise regularly
- have diabetes
- are overweight.
When you should start having heart checks depends on your age, sex, ethnicity and other risk factors. In general, the more risk factors you have, the sooner you should start being checked.
If you have no known risk factors
Men should be tested from 45 years of age and women from 55 years of age.
If you are Māori, Pasifika or South Asian (Indian, including Fijian Indian, Sri Lankan, Afghan people, Bangladeshi, Nepalese, Pakistani, Tibetan)
Men should be tested from 30 years of age and women from 40 years of age.
If you have the following risk factors:
- you smoke
- you have a family history (parent, brother or sister) of diabetes, high cholesterol, heart attack or stroke
- you have gestational diabetes (diabetes during pregnancy) or prediabetes
- you are overweight – BMI ≥ 30 or increased weight around your tummy (waist circumference ≥ 102 cm for men or ≥ 88 cm for women)
- you have kidney disease
- you have high blood pressure or cholesterol
- you have previously had heart trouble or stroke
- you have a heart condition such as atrial fibrillation.
Men should be tested from 35 years of age and women from 45 years of age.
If you have type 1 or type 2 diabetes
Annual testing as part of your yearly diabetes review.
If you have schizophrenia, major depressive disorder, bipolar disorder or other severe mental illness
Everyone should be tested from 25 years of age.
Your healthcare provider can help you work out what your current risk is and what you can do to lower your risk.
Your risk is an estimate of how likely you are to have a heart attack or stroke in the next five years. If you have a 10% risk, this means that if there were 100 people with the same risk as you, we'd expect 10 of them to have a heart attack or stroke in the next 5 years.
You should have a heart risk assessment every 5 to 10 years. If you’re found to have a high risk, you’ll need a yearly health check.
While the best option is to have a heart risk assessment with your healthcare provider, you can use an online tool called My Heart Check to give you an idea of your heart health. My Heart Check(external link) is a free online heart health check developed by the Heart Foundation. It's designed for Kiwis as it's based on New Zealand data.
No matter how high or how low your risk of heart disease is, there are always choices you can make to manage your risk and improve your heart health.
Even a small change can have a positive impact on your risk of heart attack and stroke. The more you change the better.
Learn more about:
- Stopping smoking
- Exercise and physical activity
- Eating and drinking for a healthy heart(external link)
- Reaching a healthy weight
- Managing stress
There are choices you can make today to manage your coronary artery disease(external link) better.
Apps reviewed by Healthify
You may find it useful to look at some blood pressure apps, heart failure apps, quit smoking apps, nutrition, exercise and weight management apps and stroke apps.
What happens during a heart attack?(external link) Heart Foundation, NZ
Brochures
Eating for a healthy heart(external link) Heart Foundation, NZ, 2023
Angina(external link) Heart Foundation, NZ
Heart attack warning signs(external link) Heart Foundation, NZ
Apps
Blood pressure apps
Heart failure apps
Quit smoking apps
Nutrition, exercise and weight management apps
Stroke apps
References
- What is coronary heart disease?(external link) National Heart, Lung, and Blood Institute, US
- What's my risk of a heart attack or stroke?(external link) Heart Foundation, NZ
- Heart risk assessment | Ngā aromatawai manawa(external link) Health New Zealand | Te Whatu Ora, NZ, 2025
Clinical resources
Cardiovascular disease risk assessment and management series(external link) BPAC, NZ, 2018
Continuing medical education
Video: PHARMAC seminar: Cardiovascular disease, 2a&b. Acute coronary syndrome: talk and cases, parts 1&2
(12 minutes + 15 minutes + 30 minutes = 57 minutes) Prof. Ralph Stewart
(Pharmac, NZ, 2017)
Video: PHARMAC seminar: Cardiovascular disease, 2c. Acute coronary syndrome: talk and cases, part 3
(Pharmac, NZ, 2017)
Video: PHARMAC seminar: Cardiovascular disease, 2d. Acute coronary syndrome: talk and cases, part 4
(Pharmac, NZ, 2017)
For more cardiovascular disease videos of the same series, visit Pharmac seminars(external link).
Brochures

Heart Foundation, NZ, 2023
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Sara Jayne Pietersen, FRNZCGP, Auckland
Last reviewed:





