You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Warfarin
Sounds like 'war-far-in'
Key points about warfarin
- Warfarin is an anticoagulant.
- It's used to treat and prevent clots in your blood.
- Find out how to take it safely and possible side effects.

Warfarin is an anticoagulant that is used to slow clotting. It helps to prevent blood clots from forming and stops existing clots from growing bigger. It is used for people with artificial heart valves, to protect clots developing on the valves.
It's also used for people who have an irregular heart rhythm known as atrial fibrillation because they are at increased risk of stroke. A stroke happens when blood clots form in the heart and travel to the brain. Warfarin is also used for the prevention and treatment of deep vein thrombosis, where blood clots form in veins deep within the legs and pelvis. From here, the clots can travel to the lungs and cause a pulmonary embolism.
There are different brands of warfarin
- In Aotearoa New Zealand there are 2 different brands of warfarin tablets – Marevan® and Coumadin®. Most people take the Marevan® brand.
- Marevan® and Coumadin® are slightly different from each other and they're not interchangeable. Therefore, it is important that you stay on the same brand.
- If your tablets look different from usual, check with your pharmacist.
- Both brands come in different strengths and each are a different colour. You may need to take more than one strength of tablet to make up your dose.
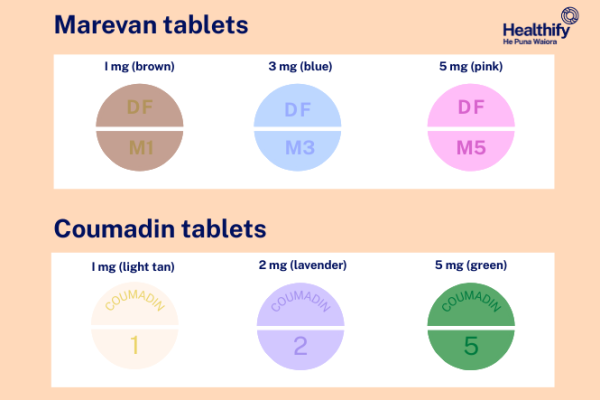
Image credit: Healthify He Puna Waiora
Video: How does warfarin work?
The following animation describes how warfarin works in your body.
(British Heart Foundation, UK, 2018)
The dose of warfarin will be different for different people. It depends on why you're taking it and your blood test results. You will need to have regular blood tests that measure how long your blood takes to clot. Your doctor will tell you how often you will need a test. The test is called an INR (international normalised ratio) test. The goal of warfarin therapy is to control blood clots. Having too little warfarin puts you at risk of your blood clotting and having too much warfarin puts you at risk of bleeding. Therefore, the effect of warfarin must be monitored carefully with blood testing. INR tests are very important to help your healthcare provider decide on the best dose of warfarin for you.
Warfarin and INR
INR tests help your prescriber work out what dosage of warfarin is right for you. They will check whether your INR blood test results are within the best range for you (INR range). An INR in the right range will prevent blood clots and reduce the risk of bleeding.
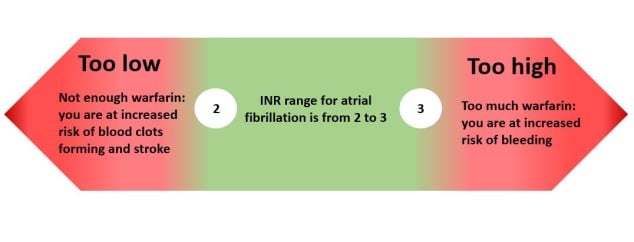
High INR: If your INR is too high, you are at increased risk of bleeding. Your warfarin dose may need to be lowered.
Low INR: If your INR is too low, you are at increased risk of blood clots forming and your warfarin dose may need to be increased.
Read more about warfarin and INR.
Timing
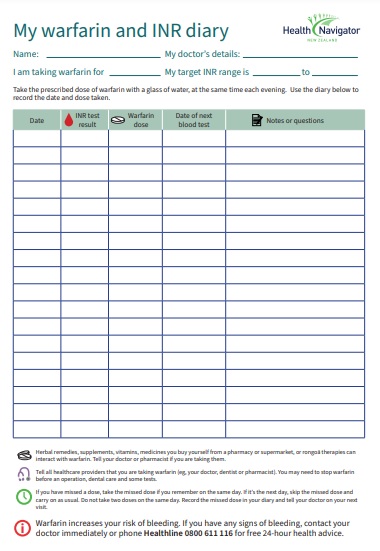
- Take your tablets (as one dose), once a day, at the same time each day.
- It's best to take your warfarin in the evening so you can have your blood test to check your INR in the morning. The test is usually done about 12 hours after taking a dose.
- You can take warfarin with or without food.
- To help you keep track of when you have taken your tablet, you can use a medicine organiser or a warfarin diary(external link).
Missed dose
- If you forget to take a dose, take the missed dose if you remember on the same day. If not, skip the dose and carry on as normal.
- Don't take 2 doses of warfarin on the same day.
- Record your missed dose in your anticoagulant booklet and tell your healthcare provider on your next visit.
- Contact your healthcare provider if you miss 2 or more doses in a row.
- Missing doses increases your risk of getting blood clots. Make sure you don’t run out of tablets – get a new prescription when you're running low.
When taking warfarin, it's important to use the medicine safely and correctly. The benefits of warfarin need to be carefully balanced with possible side effects. Not enough anticoagulation can lead to a blood clot or stroke, but too much anticoagulation can lead to serious bleeding.
You might bleed or bruise more easily while you're taking warfarin
- Be careful when shaving, clipping fingernails, brushing and flossing your teeth, or playing sports.
- Avoid new tattoos and piercings as these can cause bruising and bleeding.
- If you have a fall or hurt your head or body, get medical attention immediately, even if you feel okay.
- Some types of bleeding are more serious than others. If bleeding concerns you, is heavier than usual or takes an unusually long time to stop, you should talk to your healthcare provider quickly.
Some foods and drinks can affect warfarin
Warfarin works by interfering with the production of vitamin K – if you have too much vitamin K in your diet it can make warfarin less effective. You can still eat foods that contain vitamin K but in moderate amounts. The most important thing is to keep your regular diet stable. You shouldn't change your eating habits very much as large changes can interfere with warfarin treatment. Alcohol increases the risk of severe bleeding while on warfarin. Alcohol should be limited. If you make any changes to your regular diet, tell your healthcare provider. Read more about warfarin and diet.
Other things to be aware of
- Tell all healthcare providers that you're taking warfarin (eg, your doctor, dentist, pharmacist or podiatrist): You may need to stop taking your anticoagulant before surgery, dental care and some tests.
- Taking other medicines: Warfarin can interact with some medicines and herbal supplements, so check with your doctor or pharmacist before starting warfarin and before starting any new products. This includes over-the-counter anti-inflammatories including diclofenac (eg, Voltaren Rapid), ibuprofen (eg, Nurofen) and naproxen (eg, Naprogesic).
- Pregnancy: Warfarin isn’t given to pregnant women. If you're taking it and could become pregnant, talk to your healthcare provider about contraception. If you're on warfarin and find out you're pregnant (or you're planning a pregnancy) talk to your healthcare provider or anticoagulant clinic about stopping or changing your prescription.
Like all medicines, warfarin can cause side effects, although not everyone gets them. If you're concerned about any symptoms you think might be related to your medicine, talk to your healthcare provider. The following information offers some guidance but doesn't include all possible side effects.
Common side effects
Tell your healthcare provider if these bother you.
- Nausea (feeling sick).
- Diarrhoea (runny poo).
- Rash.
- Hair loss.
Tell your healthcare provider immediately or phone Healthline free on 0800 611 116 if these occur
- Signs of bleeding, such as unexpected bruises, bleeding gums or nosebleeds.
- For women, if you notice heavier bleeding during your period than before starting warfarin, continue your warfarin and see your healthcare provider as there are ways to manage heavy periods.
Phone 111 for an ambulance or go to your nearest accident and emergency (A&E) clinic if these occur
- You have difficulty breathing or pain in your chest.
- You have pain or swelling in your legs.
- You have symptoms of a stroke such as face drooping, arm weakness, speech difficulty, confusion, trouble seeing, trouble walking.
- You've had a serious fall or injury to your head.
- Signs of severe bleeding such as coughing up blood or vomiting blood or there is blood in your urine (wee) or bowel motions (poo).
- You have bleeding that won’t stop after 10 minutes of applying pressure.
Read more about medicines and side effects and reporting a reaction that you think might be a side effect.
Find out what to do if you think a child or someone else has taken a medicine that's not for them.
The following links have more information on warfarin:
Warfarin Guide for Rheumatic Heart Disease(external link) Te Reo Māori(external link), Samoan(external link), Tongan(external link)
Warfarin Patient Information(external link) Te Reo Māori(external link), Samoan(external link), Tongan(external link)
Warfarin(external link) (te reo Māori(external link)) New Zealand Formulary, NZ
Starting on warfarin(external link) Pharmac, NZ
Taking your warfarin medication(external link) BPAC, NZ
Marevan®(external link) Medsafe, NZ
Apps/tools
Brochures
Brochures
Healthify He Puna Waiora, NZ
English [PDF, 131 KB]Cook Islands Māori [PDF, 246 KB]

Warfarin Management Guide for Rheumatic Heart Disease
Health New Zealand | Te Whatu Ora
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:






