Respiratory tract infections | Pokenga atewharowharo
Key points about respiratory tract infections (RTIs or pokenga atewharowharo)
- Respiratory tract infections (RTIs) can affect both the upper and lower parts of your respiratory (breathing) system.
- They often occur after you get a cold or flu-like illnesses.
- Upper RTIs (eg, colds or sinus infections) can mostly be treated at home, but lower RTIs (eg, pneumonia) are more serious and generally need medical care.
- People at greater risk of serious illness may need to consult their healthcare provider.
- Reduce the spread with good hygiene, wearing a mask and getting vaccinations, including COVID-19 and influenza (flu).

|
Reminder: If you have any respiratory symptoms (eg, a cough, sore throat, shortness of breath, head cold or loss of smell, with or without a fever) test for COVID-19 if you can. |
Respiratory tract infections (RTIs) are divided into 2 categories – upper and lower.
Lower RTIs, such as pneumonia, tend to be more serious than upper RTIs, such as colds or a sinus infection.
Most upper RTIs can be treated at home, but young children, older adults, pregnant people or people with long-term health conditions who get a lower RTI may need to see a healthcare provider.
You can reduce the spread of RTIs by:
- washing your hands
- covering your coughs and sneezes
- wearing a face mask
- getting vaccinations such as the COVID-19 and flu vaccines.
Practising health lifestyle habits such as eating well, avoiding smoking, getting plenty of sleep and exercising regularly will help you to stay well.
Upper RTIs are very common and affect your nose, sinuses, throat (pharynx) and voice box (larynx). Symptoms of upper URIs include:
- sore throat
- runny nose
- nasal congestion
- headache
- low-grade fever
- facial pressure
- cough.
Common upper RTIs include:
- colds – viral infections of you nose and upper airways
- sinusitis – sinus infection
- tonsillitis – tonsil infection
- laryngitis – voice box infection
- pharyngitis – throat infection.
Lower RTIs are also known as chest infections. They affect your larger airways (bronchial tubes and bronchioles) and your lungs. Chest infections often follow a cold or flu-like illnesses.
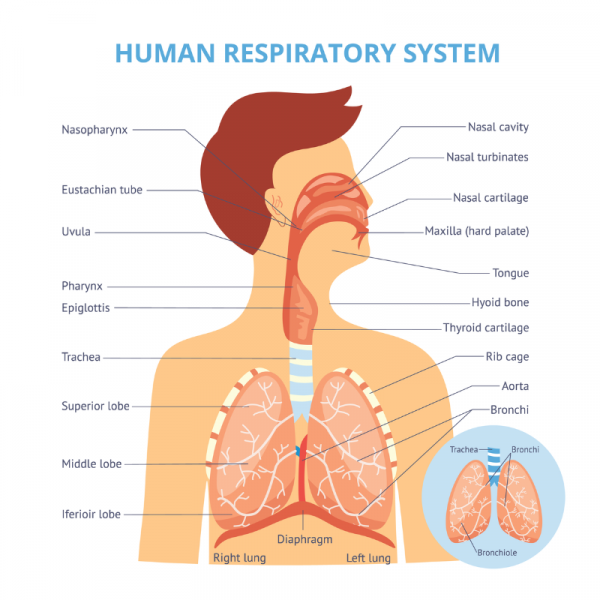
Image credit: Depositphotos
Lower RTIs are generally more serious than upper RTIs. Symptoms of lower RTIs include:
- shortness of breath
- weakness
- fever
- coughing with green or yellow/brown mucus (phlegm or sputum)
- fatigue
- aching muscles
- chest pain or discomfort.
Wheezing isn't usually a symptom unless you have underlying lung disease. Symptoms should get better in 7 to 10 days although cough and mucus can last up to 3 weeks.
Common lower RTIs include:
Most upper RTIs get better in 1 to 2 weeks and you can usually treat your symptoms at home. If you have a COVID-19 infection follow the advice provided for managing your symptoms.
However, a lower RTI can be serious. Those most at risk are young children, older adults, pregnant people or people with long-term health conditions. You may need to be considered for treatment and in some circumstances be considered for investigations, such as blood tests and chest X-ray. Note that sputum tests are not generally helpful.
See a healthcare provider immediately if you or another adult has:
|
See your healthcare provider as soon as possible if you, or someone you are caring for, has a respiratory tract infection and:
- feels very unwell or symptoms get worse
- has had a cough for more than 3 weeks
- is pregnant
- is over 65 years of age
- is a child under 2 years of age
- has a weakened immune system
- has a long-term health condition, such as diabetes, heart disease, asthma, COPD (chronic obstructive pulmonary disease).
The most common cause of a sore throat is a viral infection, but some people with a sore throat may have strep throat. This is a bacterial infection that can lead to rheumatic fever and permanent heart damage in certain people if it isn’t treated.
Symptoms of a strep throat
There may be:
- redness
- swelling
- white patches on the tonsils in the back of your throat
- pain when swallowing
- swelling of the lymph nodes in the front of your neck.

Image credit: Doc James via Wikimedia Commons(external link)
People at risk of complications of strep throat include:
- those who’ve had rheumatic fever before, or who have family or household members with a history of rheumatic fever or rheumatic heart disease
- Māori and Pacific Peoples 3 to 35 years of age – especially children and teenagers
- those living in crowded housing conditions.
See your healthcare provider if you or your child are at high risk of rheumatic fever and have any of the symptoms listed above. Antibiotics may be required for this type of infection and will be effective in clearing it up.
Most upper RTIs are caused by a virus. Viral infections can't be treated with antibiotics as they only work for bacterial infections. However, severe or persistent sinus infections may need treatment with antibiotics. Read more about chronic sinusitis.
Your immune system will be able to fight off most viral infections. Misusing antibiotics to treat viral infections contributes to the problem of antibiotic resistance. If you have a COVID-19 infection you may be eligible for antiviral treatments.
Some lower RTIs (eg, pneumonia or severe bronchitis) are usually caused by bacteria. Your healthcare provider may need to prescribe a course of antibiotics if you have a lower RTI.
Always take antibiotics according to your healthcare provider's instructions and, for most infections, make sure you complete the entire course of treatment even if you're feeling better. You may get the infection again and some antibiotics may no longer work if the bacteria have become resistant.
If you need a course of antibiotics several times a year, make sure that you have been checked for:
- underlying lung disease
- problems with your immune function
- chronic sinus disease.
To help you or the person you are caring for feel more comfortable and speed your recovery, take the following self-care steps:
- Get plenty of rest.
- Drink lots of water to stay hydrated and loosen mucus.
- Take paracetamol or ibuprofen for pain and fever. Avoid aspirin in young children.
- Drink warm lemon and honey for a sore throat and cough – to make the drink, squeeze half a lemon into a cup of boiled water and stir in 1 to 2 teaspoons of honey. Note that honey shouldn't be given to babies under 12 months of age.
- Gargle warm salty water for a sore throat – dissolve half a teaspoon of salt in a glass of warm water. Gargle the solution then spit it out. You can repeat this as many times as you like. Children shouldn’t try this.
- Take a teaspoon of honey for a cough. Note that honey shouldn't be given to babies under 12 months of age.
- Rub mentholated ointment onto your chest.
- Try decongestants and nasal sprays for a blocked or runny nose.
- Use a saline nose rinse for sinus congestion.
- Use pillows to raise your head while you're sleeping to make breathing easier and clear mucus.
- If you've been prescribed any medicines, take these as directed.
- If your cough hasn't resolved after 3 weeks, see your healthcare provider – particularly if you are a smoker, have smoked in the past or if there could be other underlying lung disease such as asthma or COPD.
Contact your healthcare provider immediately or call Healthline free on 0800 611 116 if you or your child have trouble breathing, have a high fever or show other signs that the infection is getting worse.
Do the following to prevent passing on a respiratory tract infection to others. These things will also reduce your risk of getting a RTI if you're in contact with other people who have one.
- Wash your hands often.
- Cover your coughs and sneezes, eg, by using a tissue or coughing or sneezing into your elbow.
- Use disposable tissues and put them in a bin straight away.
- Clean surfaces around the house more often.
- Stay at home if you are unwell.
- Consider using a face mask when in contact with others.
Vaccinations
Vaccinations can protect against certain viruses. However, not all viruses can be vaccinated against. Get the annual flu vaccination – find out if you're eligible for the free flu vaccine(external link). Consider receiving the COVID-19 vaccination / booster every 6 months. You may be a candidate for the RSV vaccination.
If you keep getting RTIs or you're at a high risk of getting one (eg, because you're over 65 years of age or have a serious long-term health condition, such as diabetes, heart disease, asthma, or COPD) also ask your healthcare provider about the pneumococcal vaccine(external link) – this helps prevent some types of pneumonia.
Ensure your whooping cough vaccinations are up to date.
Being generally healthy, being smoke and vape-free and eating a healthy diet should also reduce your risk of getting a respiratory tract infection.

Chest infection(external link) NHS, UK
Respiratory tract infection(external link) NHS, UK
Chest infections(external link) Better Health, Australia
Common cold(external link) Patient Info, UK
Sore throat in detail(external link) KidsHealth, NZ
References
- Chest infection(external link) NHS, UK, 2023
- Respiratory tract infection(external link) NHS, UK, 2021
- Sore throat in detail(external link) KidsHealth, NZ, 2021
- Is it ok to stop antibiotics when symptoms resolve?(external link) BPAC, NZ, 2015
Clinical resources
Navigating uncertainty – managing respiratory tract infections(external link) BPAC, NZ, 2019
Cold season – managing without antibiotics(external link) BPAC, NZ, 2018
Te ha ora – the breath of life – national respiratory strategy(external link) Asthma & Respiratory Foundation, NZ, 2015
Suspected acute respiratory infection in over 16s – assessment at first presentation and initial management(external link) NICE, UK, 2023
Sinusitis (acute) – antimicrobial prescribing(external link) NICE, UK, 2017
Sore throat (acute) – antimicrobial prescribing(external link) NICE, UK, 2018
Cough (acute ) – antimicrobial prescribing(external link) NICE, UK, 2019
Webinar
Practical prescribing for respiratory infections(external link) (Goodfellow Unit, NZ, 2017)
Video: Goodfellow Unit MedTalk – respiratory infections
(Goodfellow Unit, NZ, 2017)
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Roland Meyer, Specialist Physician, Respiratory and General Medicine
Last reviewed:





