If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Acute bronchitis
Also known as bronchitis, chest infection or chest cold
Key points about bronchitis
- Acute bronchitis is swelling and inflammation inside the main airways of your lungs (bronchi), causing them to produce more mucous.
- The main symptom is a chesty or productive cough, with green or yellow mucous. You may also have cold symptoms.
- It's most often caused by a virus, possibly by a COVID-19 infection so it's advisable to do a COVID test.
- You should start to feel better after a few days, but the cough may last for a few weeks longer.
- Contact your healthcare provider or call Healthline on 0800 611 116 if you have shortness of breath and high fever, or if you feel very unwell.

Acute bronchitis is commonly caused by a virus. It’s when the inside of your lungs becomes swollen causing them to create more mucous. Your body responds by coughing to bring the yellow or green mucous up and out of your lungs. You may also have other cold-like symptoms such as a sore throat, runny nose and mild fever.
There are 2 types of bronchitis – acute and chronic.
This page covers acute bronchitis (chest infection) in adults. For information on chronic bronchitis (chronic obstructive pulmonary disease or COPD) see COPD. For information on chest infection in babies and children under 2 years of age see bronchiolitis.
The image below shows what happens to your airways when you have bronchitis.
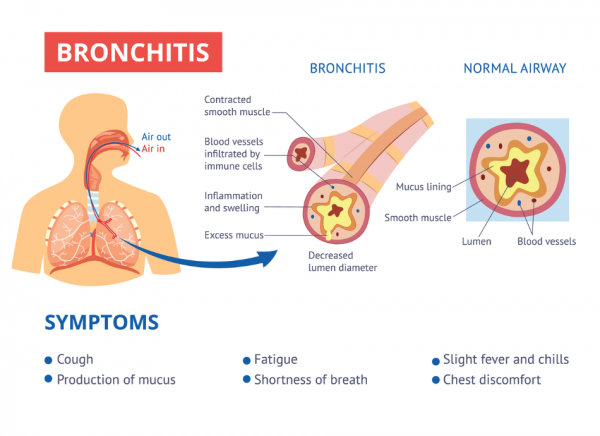
Image credit: Depositphotos
What causes acute bronchitis?
The main cause of acute bronchitis is a virus. This is often the same virus that causes a common cold, which is why bronchitis often occurs after a cold. Acute bronchitis is more common in winter. It may also be caused by a COVID-19 infection.
Acute bronchitis can affect people of all ages. For information on chest infection in babies under 6 months of age see bronchiolitis.
What are the symptoms of acute bronchitis?
The main symptom is a chesty or productive cough where you bring up green or yellow mucous. You may also get cold symptoms, such as:
- mild fever
- sore throat
- aches and pains
- runny nose
- headache
- tiredness.
You’ll usually start to feel better after a few days, but the cough may remain for a few weeks.
|
If you, or a family member, are short of breath, coughing up blood, have a high fever or feel very unwell you need to talk to your healthcare provider or call Healthline on 0800 611 116 straight away. These are the signs that a chest infection is more serious – it could be pneumonia or another serious condition. |
You don’t usually need to see your healthcare provider if you have acute bronchitis as your body will fight the virus and get better by itself.
You can help yourself feel better by:
- resting for a few days
- drinking plenty of fluids, mainly water, to help prevent dehydration
- using an extra pillow to elevate your head as you sleep
- quitting if you smoke
- using your inhaler if you have asthma or another chronic lung condition.
Consult your healthcare provider if:
- your cough is bothering you and/or lasts for more than 2 weeks
- you have a high fever
- you have pain when coughing.
Apps reviewed by Healthify
You may find it useful to look at some Asthma apps and Quit smoking apps.
Usually, the symptoms of acute bronchitis go away by themselves after a few days and don't require medication. However, the following medicines may help to ease your symptoms:
Pain relievers
Medication such as paracetamol or ibuprofen will help to ease your muscle aches and pains and headache, and reduce fever but they won't help with your cough.
Cough medicines
You might want to consider cough medicines, but they won't treat the virus or bacteria causing your bronchitis. If you do, choose an expectorant one (eg, for a 'phlegmy' cough) as this is designed to help clear mucous from your lungs.
Avoid cough medicines that reduce your urge to cough (suppressants). These may help if you have an irritating, dry cough, especially at night, but they shouldn't be used if your cough is chesty.
A drink of honey, lemon and hot water, can help soothe a sore throat and ease your cough.
Read more about cough medicines for adults.
Cough and cold medicines for children
- Note that cough and cold medicines are not recommended for children under 6 years of age.
- For children 6 to 12 years of age, only use cough and cold medicines that say on the label they can be used for that age group. Read more about cough and cold medicines in children.
Antibiotics
Antibiotics are not often used to treat acute bronchitis because they have no effect on viruses, which are usually the cause of bronchitis.
However, if your healthcare provider thinks you also have a bacterial infection in your airways, you may need to take antibiotics.
Inhalers
If you are wheezing, your doctor may prescribe an inhaler to open your airways, such as salbutamol, the same medicine you may have heard of for asthma treatment.
Bronchitis can’t always be prevented but some things might help:
- Washing your hands can prevent the spread of viruses that can cause bronchitis.
- Wearing a face mask in crowded spaces and when you're near others who are sick. This will also reduce the risk of you spreading a virus.
- Avoid smoking or other lung irritants.
-
Be up-to-date with your vaccinations such as:
-
Flu vaccine - recommended to get every year to be protected against current strains
The following links provide further information on bronchitis. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
What is acute bronchitis?(external link) Asthma and Respiratory Foundation NZ
Chest infections (bronchitis)(external link) Health New Zealand | Te Whatu Ora
Bronchitis(external link) NHS, UK
Apps
Resources
Virus action plan (adult)(external link) He Ako Hiringa, NZ, 2023 te reo Māori(external link), Samoan(external link), Tongan(external link), Arabic [PDF, 188 KB], Hindi(external link), Chinese (simplified)(external link)
Virus action plan (child over 6 months)(external link) He Ako Hiringa, NZ te reo Māori(external link), Samoan(external link), Tongan(external link), Arabic [PDF, 214 KB], Hindi(external link), Chinese (simplified)(external link)
Bronchitis – what causes bronchitis?(external link) Choosing Wisely, NZ
Bronchitis – how is bronchitis diagnosed?(external link) Choosing Wisely, NZ
Bronchitis – medicines and treatments)(external link) Choosing Wisely, NZ
Bronchitis – what are the symptoms of bronchitis?(external link) Choosing Wisely, NZ
What is acute bronchitis?(external link) Asthma Respiratory Foundation NZ
References
- Respiratory tract infections (self-limiting) – reducing antibiotic prescribing(external link) BPAC, NZ, 2015
- Acute cough illness (acute bronchitis)(external link) Centers for Disease Control, US, 2024
- Paul IM, Beiler J, McMonagle A, et al. Effect of honey, dextromethorphan, and no treatment on nocturnal cough and sleep quality for coughing children and their parents(external link) Arch Pediatr Adolesc Med. 2007 Dec;161(12):1140-6.
Clinical resources
Respiratory tract infections (self-limiting) – reducing antibiotic prescribing(external link) BPAC, NZ, 2015
CICADA – cough in children and adults(external link) Australian cough guidelines summary statement
Acute cough illness (acute bronchitis)(external link) Centers for Disease Control, US
Apps
Brochures
Choosing Wisely, NZ, 2016

Virus action plan (adult)(external link) He Ako Hiringa, NZ, 2023 te reo Māori, Samoan, Tongan, Arabic, Hindi, Chinese (simplified)
Virus action plan (child)(external link) He Ako Hiringa, NZ, 2023 te reo Māori, Samoan, Tongan, Arabic, Hindi, Chinese (simplified)
Choosing Wisely, NZ, 2016
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Roland Meyer, Specialist Physician, Respiratory and General Medicine
Last reviewed:





