You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Strep throat
Key points about strep throat
- Strep throat is different from a sore throat that you might get with a cold caused by a virus.
- Without treatment, strep throat can cause rheumatic fever. Rheumatic fever can damage your, or your tamariki’s heart.
- Strep throat is caused by a bacteria called Streptococcus pyogenes. It’s spread by close contact, often by breathing in droplets from an infected person’s coughs and sneezes.
- It’s important to get sore throats checked by your GP or nurse especially if you or your tamariki are at high risk of rheumatic fever.
- Strep throat can be treated with antibiotics to get rid of the infection and prevent rheumatic fever.

Strep throat is a contagious infection caused by a bacteria. It’s different from a sore throat you might get with a cold that’s caused by a virus.
If it’s not treated, strep throat can cause rheumatic fever which can result in permanent damage to your, or your tamariki’s heart. The risk of getting rheumatic fever increases if you have repeated untreated strep throat infections.
It’s important to get sore throats checked by your healthcare provider, especially if you or your tamariki are at high risk of rheumatic fever. Strep throat can be treated with antibiotics to get rid of the infection and prevent rheumatic fever. Read more about rheumatic fever.

Image credit: James Heilman, MD, via Wikimedia Commons(external link)
If you or your child are at high risk of rheumatic fever, it’s very important that any sore throat you get is always checked early by a nurse or GP. This is because untreated strep throat can cause rheumatic fever and heart damage for life.
You’re at higher risk of rheumatic fever if:
- you’ve had rheumatic fever before
- someone in your family or household has had rheumatic fever.
You’re also at higher risk if 2 or more of these apply to you:
- you’re Māori or Pacific Peoples
- you’re 3 to 35 years of age, especially tamariki or rangatahi 4 to 19 years of age
- you live in poorer or crowded living conditions.
Strep throat is a sore throat that’s caused by a bacteria called Streptococcus pyogenes or group A strep. It’s contagious and is usually spread by breathing in droplets from the coughs and sneezes of someone who has the infection. It can also be spread through kissing or sharing food, drinks or toothbrushes.
Some people may get strep throat after touching skin sores infected with the strep bacteria.
Symptoms of strep throat can include:
- a painful or scratchy throat, especially when you swallow
- difficulty swallowing
- redness at the back of your mouth
- fever
- bad breath
- swollen glands in your neck
- enlarged tonsils covered in white stuff
- headache
- stomach pain
- nausea (feeing sick) and vomiting (being sick).
Sometimes, you may also have a skin rash along with fever and sore throat. This condition is known as scarlet fever.
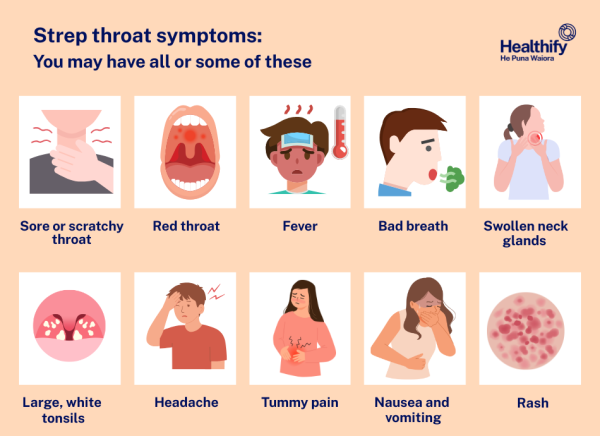
Image credit: Healthify He Puna Waiora
It's very difficult to tell the difference between strep throat and a sore throat that’s caused by a virus.
You should get any sore throat checked by a healthcare provider (eg, at your medical centre or at school) straight away, especially if you or your child is at high risk of rheumatic fever.
Don’t wait to see if the sore throat gets better by itself. Strep throat needs to be treated immediately. Treating sore throats early can stop rheumatic fever from developing.
Tell your children to let you when they have a sore throat so they can be checked. Your child may get a lot of sore throats, but you need to get them checked every time and straight away.
Video: Checking sore throats to prevent rheumatic fever
(NZKidsHealth, NZ, 2018)
Strep infection is diagnosed by doing a throat swab. Your doctor of nurse will do this when you get your throat checked, it's not painful. If your swab is positive for group A strep, you’ll be treated with antibiotics to get rid of the infection and prevent rheumatic fever.
If you’re at high risk of rheumatic fever, you may be started on antibiotic treatment without having a throat swab.
The treatment of strep throat depends on your risk of getting rheumatic fever. If you’re very unwell, you’ll be referred to the hospital for tests and treatment.
Low risk of rheumatic fever
If you have a sore throat and you’re not at high risk of rheumatic fever, treatment is just self-care to ease the pain – the infection will get better on its own in a few days. See below for things you can do to help ease your sore throat.
High risk of rheumatic fever
If you’re at high risk of rheumatic fever you’ll need antibiotic medicine. You may also be given antibiotics if you have a weakened immune system or if you have a high risk of spreading the strep bacteria, such as if you’re a healthcare worker, residential care worker, food handler, teacher, childcare worker or student.
- Oral antibiotics (penicillin V or amoxicillin) are normally given for 10 days. It’s important that you, or your child, finish all the antibiotics, even if you feel better, to make sure the strep throat doesn’t cause rheumatic fever. If you have a penicillin allergy, you’ll be given erythromycin instead.
- A one-off antibiotic injection to treat a strep throat might be a good alternative if you think it may be difficult to take the full 10-day course of antibiotic capsules or liquid. You can ask your healthcare provider to consider this if you would prefer it.
- Keep children away from school or early childhood centres for at least 24 hours after they start antibiotics, to reduce the risk of spreading the strep bacteria.
Everyone in your whānau or household should have a throat swab if:
- anyone in your whānau or household has had rheumatic fever, or
- there have been 3 or more cases of strep throat in your whānau or household in the last 3 months.
If their swab comes back positive for group A strep they should be treated for strep throat – even if they're feeling well.
Repeated sore throats
If you have tamariki or rangatahi who’ve had 3 or more sore throats due to a Strep A infection over a 3-month period, they’ll be given a one-off antibiotic injection or a 10-day course of oral antibiotics under the supervision of a healthcare provider. They’ll be re-swabbed after finishing the antibiotics and if they’re still positive for Strep A they’ll be referred to a specialist doctor to see what further treatment they need. Everyone in your whānau or household should also be swabbed and treated if their swab result is positive.
There are things you can do to ease your sore throat.
- Suck a teaspoon of honey (note that this isn’t safe for children under 12 months of age) or gargle warm salt water. You can make salt water by mixing a teaspoon of salt in a cup of warm water. Spit out the water after gargling.
- Adults can try using a gargle, throat spray or pain-relief (anaesthetic) lozenges that you can get from your pharmacy. These aren’t suitable for children.
- Children may find frozen treats such as smoothies, popsicles or ice cream soothing.
- Have soft foods or soups if it hurts to swallow.
- Take paracetamol – check doses carefully and ask your healthcare provider or pharmacist whether it’s safe for you. Use our paracetamol dose calculator to find the right dose for your tamariki.
- You should go back to your healthcare provider if you or your child get worse after 24 hours or develop any symptoms of rheumatic fever, such as painful or swollen joints (eg, hips, knees, elbows) fever, rash or jerky movements.
Do the following things to help stop strep infections spreading or coming back.
- Cover your mouth and nose with your elbow or a tissue when you sneeze or cough and throw used tissues away.
- Avoid close physical contact, such as kissing, when you’re sick, and don’t share eating or drinking utensils (eg, cups or knives and forks).
- Wash your hands well with soap and water before eating or preparing food.
- Try to have space between your children when they sleep to reduce the chance of germs being spread through coughs and sneezes.
- Keep your home warm and dry. Find out about the Healthy Homes Initiative(external link) which helps eligible families to make their homes warmer, drier and healthier.
- Get all sore throats checked and treated by your healthcare provider or school nurse. Contact your child’s school to see if they have a free sore throat check programme.
- Some pharmacies also do free sore throat checks. You can also call Healthline free on 0800 611 116 if you’re worried about your child's sore throat.
- Get skin infections treated too as this limits the spread of strep A bacteria.
The following links provide further information about strep throat. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Strep throat – a patient's guide(external link) Family Doctor, NZ
Strep throat(external link) Centers for Disease Control and Prevention, US
Strep throat in kids and teens(external link) Nemours KidsHealth, US
Brochures
Steps of rheumatic fever(external link) Health Promotion Agency and Ministry of Health, NZ, 2013 available in English(external link), te reo Māori(external link), Cook Island Māori(external link), Samoan(external link), Tokelauan(external link), Tongan(external link), Tuvaluan(external link)
Help stop rheumatic fever from hurting hearts(external link) Stop Sore Throats Hurting Hearts, NZ
References
- Aotearoa New Zealand guidelines for the prevention, diagnosis, and management of acute rheumatic fever and rheumatic heart disease – 2024 update(external link) Health New Zealand | Te Whatu Ora, NZ, 2024
- Sore throat(external link) Health New Zealand | Te Whatu Ora, 2025
- Anderson A, Spray J. Beyond awareness – towards a critically conscious health promotion for rheumatic fever in Aotearoa, NZ(external link) Soc Sci Med. 2020; 247:112798
- Acute pharyngitis – aetiology(external link) BMJ Best Practice, UK, 2025
- Rheumatic fever(external link) Health New Zealand | Te Whatu Ora, 2025
Aotearoa New Zealand guidelines for the prevention, diagnosis, and management of acute rheumatic fever and rheumatic heart disease – 2024 update(external link) Health New Zealand | Te Whatu Ora, NZ, 2024
Rheumatic fever(external link) Health New Zealand | Te Whatu Ora, 2025
Webinar
Don’t miss that ARF diagnosis(external link) (64 mins) Goodfellow Unit, NZ, 2024
Presented by Dr Barnett Bond (GP and Chairman of the Auckland Rheumatic Fever and Rheumatic Heart Disease Group, Mary-Anne Ross (Rheumatic Fever Nurse specialist) and Assoc. Prof Nigel Wilson (Paediatric Cardiologist).
Brochures
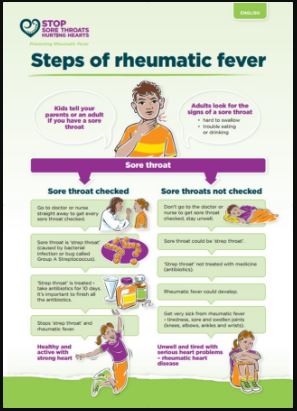
Steps of rheumatic fever, Health Promotion Agency, NZ, 2013
English, te reo Māori, Cook Island Māori, Samoan, Tokelauan, Tongan, Tuvaluan
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Sara Jayne Pietersen, FRNZCGP, Auckland
Last reviewed:






