If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Sore throat in adults | Mate korokoro
Also called pharyngitis
Key points about sore throats
- Having a sore throat is very common, especially in children (see our other page on sore throat in children). The discomfort can range from a scratchy feeling to severe pain.
- A sore throat can be caused by a viral infection, eg, a cold, the flu or COVID.
- It can also be caused by a bacterial infection – most commonly Streptococcus (often known as 'strep throat').
- If you're at higher risk of rheumatic fever, you need to have any sore throat checked by a healthcare provider. If it's not treated it can cause rheumatic fever and heart damage. If it's strep throat you will need antibiotics.

Causes of a sore throat
About 90% of sore throats are caused by viral infections, eg, the common cold, flu or COVID. Viral sore throats usually get better by themselves within a week. Antibiotics don't fix viral sore throats.
Some sore throats are caused by bacteria, most commonly Streptococcus (often known as 'strep throat'). Read more about strep throat.
Children and young people at risk of rheumatic fever require treatment with antibiotics for 10 days to prevent rheumatic fever. Find out when you need to see a healthcare provider and when you need to see one urgently in the section below.
Other conditions that can cause a sore throat include:
Video: Sore throats in adults – your essential guide
(Healthify He Puna Waiora, NZ, 2025)
Māori tamariki and Pasifika children are most at risk of developing rheumatic fever and should see a doctor or nurse if they show ANY sign of sore throat.
Video: Rheumatic fever
(Stop Sore Throats Hurting Hearts, NZ, 2016)
When to get help if you're at higher risk of rheumatic fever
|
For people at higher risk of rheumatic fever, it is very important that a sore throat is always checked early by a nurse or GP. This is because untreated strep throat can cause rheumatic fever and heart damage for life. |
You are at higher risk of rheumatic fever if:
- you have had rheumatic fever before
- someone in your family or household has had rheumatic fever.
You are also at higher risk if you have 2 or more of the following:
- Māori or Pasifika ethnicity
- You're 3 to 35 years of age
- You live in poorer or crowded living conditions.
When to get help if you're not at higher risk of rheumatic fever
If you're not high risk for rheumatic fever, you should see your healthcare provider if your symptoms aren't improving after 48 hours, or if you:
- have neck stiffness or ear pain
- have swollen glands (feel for tender lumps in your neck) that are getting bigger
- have any other symptoms you're concerned about.
Seek immediate medical help if you:
Call Healthline 0800 611 116 if you're not sure what to do. |
The main symptoms of a sore throat are:
- a painful or scratchy throat, especially when you swallow
- difficulty swallowing
- redness at the back of your mouth
- bad breath
- cold and flu symptoms, eg, a cough, hoarseness, red eyes and runny nose (usually not seen with strep throat).
- swollen glands in your neck
- your tonsils are large and covered in white stuff.
The image below shows a normal throat and a red throat with white spots on a swollen tonsil.
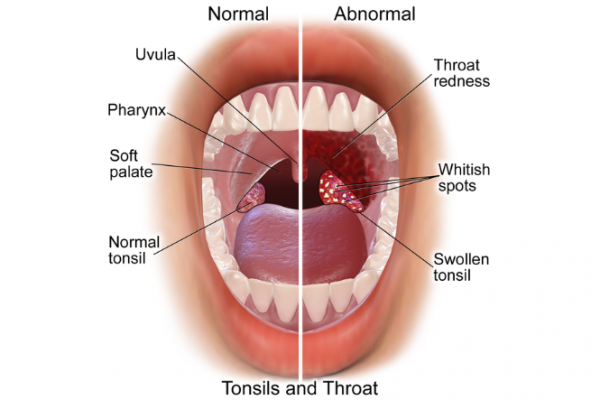
Image credit: Medical gallery of Blausen Medical 2014 via Wikimedia Commons(external link)
It's not possible to be sure from symptoms whether a sore throat is caused by a virus or bacteria. This is why people at higher risk of rheumatic fever should always get a throat swab done. See diagnosis and treatment of strep throat.
Your healthcare provider will ask questions about your symptoms and look in your mouth. They may take a throat swab to test for Streptococcus if you are at high risk of rheumatic fever or are at risk of spreading a strep throat infection. For example, if you are a:
- healthcare worker
- residential care worker
- food handler
- teacher
- childcare worker
- student.
If glandular fever is suspected you may need to have a blood test.
Self-care
The treatment of a sore throat depends on the cause. A sore throat that's caused by a viral infection is usually treated by self-care measures such as:
- pain relief medicines
- drinking more fluids
- eating soft foods
- trying ice blocks
- honey and lemon juice.
Medicines for sore throat
A sore throat is often caused by a viral infection, and the pain and discomfort usually eases after a few days. It often doesn't need treatment with medicine. But if the pain is very uncomfortable you can use the following medicines to ease the symptoms.
| Medicines | Description |
|---|---|
| Paracetamol or ibuprofen |
|
|
Throat products (lozenges, |
Talk to your pharmacist about the best pain relief for you or your child. Medicated throat lozenges are not suitable for children. Some lozenges have a high sugar content and may not be suitable for people with diabetes. |
| Cough suppressants |
|
When are antibiotics used for sore throat?
Most people don't need antibiotics for a sore throat because most sore throats are caused by viruses and antibiotics are not effective at killing viruses. Antibiotics don't make much difference to symptoms – you have a 50% chance of being better in 3 days without antibiotics, and within 3 days with them. In either case, with or without antibiotics, you have a 90% chance of being better in 7 days.
Antibiotics are needed in some cases – although it's not considered worthwhile to routinely prescribe antibiotics for most children, Māori or Pasifika children or those coming from crowded homes may benefit from taking antibiotics. This is because the chances of them developing other health problems such as ear infections, rheumatic fever or glomerulonephritis (inflammation of the kidneys) are higher than for most children.
Antibiotics may also be given if you are at risk of spreading a strep throat infection, eg, if you are a:
- healthcare worker
- residential care worker
- food handler
- teacher
- childcare worker
- student.
The course of the antibiotics is usually for 10 days, and it is important that you or your child complete the full 10 days of antibiotics, even if you or your child start to feel better. This helps to stop strep throat from turning into rheumatic fever. Antibiotics can be given in a form of a capsule, liquid or as an injection.
To help soothe a sore throat you can do these things:
- Drink plenty of cool or warm water or diluted juice.
- Eat cool, soft food or warm soups.
- Older children and adults may be able to gargle with warm salt water.
- Suck on ice cubes.
- Avoid smoking or smoky places.
- Rest as much as you can.
- Suck medicated throat lozenges (not for children).
- Take pain relief medicine, eg, paracetamol or ibuprofen.
Apps reviewed by Healthify
You may find it useful to look at some Self-management and healthy living apps.
Sore throat (external link) Health New Zealand | Te Whatu Ora
Rheumatic fever prevention programme(external link) Health New Zealand | Te Whatu Ora
Sore throat in children(external link) KidsHealth NZ
It starts with a sore throat(external link) East Bays Courier, Auckland
Coughs, colds and sore throats – antibiotics aren’t likely to help coughs, colds or sore throats(external link) Choosing Wisely, NZ
Apps
Self-management and healthy living apps
Brochures
Sore throats and rheumatic fever(external link) Health Promotion Agency, NZ, 2013
Virus action plan (adult)(external link) He Ako Hiringa, NZ, 2023 te reo Māori(external link), Samoan(external link), Tongan(external link), Arabic [PDF, 188 KB], Hindi(external link), Chinese (simplified) (external link)
Virus action plan (child)(external link) He Ako Hiringa, NZ, 2023 te reo Māori(external link), Samoan(external link), Tongan(external link), Arabic [PDF, 214 KB], Hindi(external link), Chinese (simplified) (external link)
References
- Sore throat(external link) Auckland Regional HealthPathways, NZ, 2020
- Sore throat(external link) Health New Zealand | Te Whatu Ora
- Rheumatic fever and heart disease(external link) Heart Foundation, NZ, 2023
Clinical guidelines and resources
Antibiotics – choices for common infections(external link) BPAC, NZ, 2023
Navigating uncertainty – managing respiratory tract infections(external link) BPAC, NZ, 2019
Management of recurrent group A streptococcal (GAS) positive sore throats in children and adolescents at high risk of rheumatic fever(external link) Ministry of Health, NZ and Heart Foundation, NZ, 2019
NZ guidelines for rheumatic fever – group A streptococcal sore throat management guidelines 2019 update(external link) Heart Foundation, NZ, 2019
Summary of key changes in the group A streptococcal sore throat management guideline 2019 update(external link) Heart Foundation, NZ, 2019
Sore throat algorithm(external link) Heart Foundation, NZ, 2019
Antimicrobial stewardship using pharmacy data(external link) NZ Medical Journal, 2016
Guide for household sore throat management(external link) Heart Foundation, NZ, 2019
Rheumatic fever in Māori – what can we do better?(external link) BPAC, NZ, 2011
Sick and tired of being tired and sick – laboratory investigation of glandular fever(external link) BPAC, NZ, 2012
Apps
Brochures
Sore throats and rheumatic fever
Health Promotion Agency, NZ, 2013

Virus action plan (adult)(external link) He Ako Hiringa, NZ, 2023 te reo Māori, Samoan, Tongan, Arabic, Hindi, Chinese (simplified)
Virus action plan (child)(external link) He Ako Hiringa, NZ, 2023 te reo Māori, Samoan, Tongan, Arabic, Hindi, Chinese (simplified)
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator
Last reviewed:
Page last updated:





