If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Tonsillitis | Pokenga repe korokoro
Key points about tonsillitis
- Tonsillitis (pokenga repe korokoro) is when the tonsils at the back of your throat become red and swollen (inflamed).
- Tonsillitis is common in children over 2 years of age, but teenagers and adults can get it too.
- Treatment for tonsillitis is usually rest and pain relief.
- Surgical removal of your tonsils (tonsillectomy) may be considered if you get tonsillitis often.
- Tonsillitis caused by 1 type of bacteria (group A strep) may trigger rheumatic fever for at-risk groups. This may harm the heart, joints, skin and brain – so learn the signs for when you need to get help urgently.

Your tonsils are the 2 small, rounded masses of tissue that can be seen at the sides of the back of your throat. They’re made of tissue similar to your lymph glands and are part of your immune system. Tonsils are thought to help protect your body from infection during the first year of life but are not essential for immune function in later life.
Tonsillitis is the medical name for when your tonsils become red and swollen (inflamed). Tonsillitis can happen more than once.
Viruses
Tonsillitis is usually caused by viruses, such as those related to colds. You can inhale the viruses through droplets in the air from people sneezing and coughing, or by contact with secretions from the nose or throat of people with the infection. Tonsillitis may be a symptom of the Epstein-Barr virus which causes glandular fever – this is more common in teenagers.
Bacteria
The main type of bacteria causing tonsillitis is Group A Streptococcus (group A strep), which causes a strep throat infection. If you have group A strep throat you may need to take antibiotics if you have other risk factors for rheumatic fever. Untreated strep throat can lead to serious complications for vulnerable groups, such as rheumatic fever (which can cause permanent damage to your heart) or inflammation of your kidneys. Read more about rheumatic fever.
Symptoms can include:
- sore throat (often severe)
- red and swollen tonsils
- hoarse or no voice
- a high temperature (fever) of 38°C or above
- difficulty swallowing
- headache
- swollen lymph nodes (glands) on either side of your neck
- possibly pus on your tonsils.
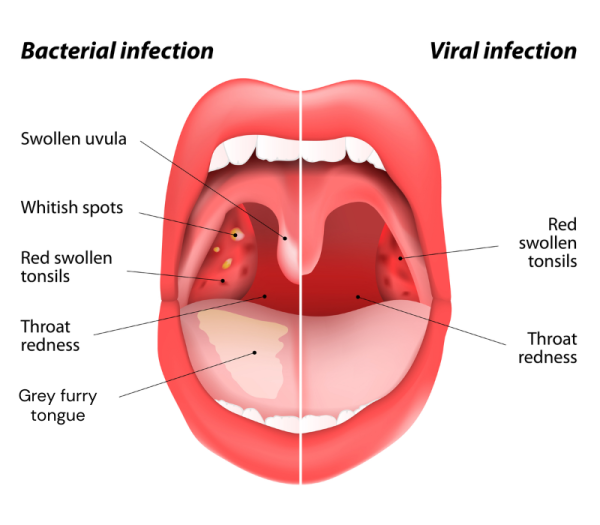
Image credit: Depositphotos
At risk of rheumatic fever?
The group A strep bacteria that causes tonsillitis can cause rheumatic fever. This is a very serious condition that can lead to heart damage and kidney disease.
It's important that you seek urgent medical advice if you have any signs of tonsillitis and have:
- a personal, family, or household history of rheumatic fever, or
- 2 or more of the following:
- Māori or Pacific ethnicity
- you're 3 to 35 years of age
- living in crowded accommodation or a lower socio-economic area.
- have difficulty breathing
- can't swallow saliva, which may cause dribbling
- can't get enough fluids
- have severe pain
- have ongoing high fever
- aren't improving after two days
- have earache or joint pain.
If you're not sure what to do, phone Healthline on freephone 0800 611 116. Calls are free and are answered by registered nurses or other health professionals who can help you.
Usually, your healthcare provider will only need to talk to you about your symptoms and look at your throat. If they need to clarify the cause of tonsillitis or consider other diagnoses, they may order more tests such as a swab or a blood test.
If you're at risk of rheumatic fever or if you have a job where you are at risk of spreading an infection (such as teaching or being a student), you may have a swab taken from your throat to check for strep throat.
If your healthcare provider thinks you might have glandular fever they will arrange for a blood test.
Mild tonsillitis often doesn't need any treatment and symptoms get better in 2 or 3 days.
Self-care for tonsillitis
Rest
Children and adults need rest to recover from tonsillitis.
Fluids and food
Make sure the person with tonsillitis drinks plenty of fluids, mainly water, especially if they have a fever (high temperature).
- Offer cold drinks, sips of ice to suck or ice blocks. They may like some soft foods such as jelly, ice cream or custard.
- Don’t worry if they don't eat much for a few days, as long as they drink plenty of fluids.
- Children and older adults should be taken to the doctor if they haven't managed to drink anything for 15 hours.
Medicines for tonsillitis
Pain relief medications
- Taking pain relief medicines such as paracetamol may ease your symptoms and may allow you to eat and drink more comfortably. Read more about paracetamol.
- You can also use ibuprofen, an anti-inflammatory medicine, to ease the pain. Note that ibuprofen may not be suitable if you have some medical conditions or if healthcare providers are concerned that you have rheumatic fever – they may ask you to avoid it until the diagnosis is confirmed. Read more about ibuprofen.
Over-the-counter products
Pharmacy sore throat products such as lozenges, sprays, or gargles can ease pain – some numb soreness with anaesthetics, while others use antiseptics or anti-inflammatories. Always follow directions and ask your pharmacist for the best choice for you or your child. Don't use medicated lozenges for children, and choose low-sugar options if you have diabetes.
Gargling may help
Older children and adults may be able to gargle with warm salt water to relieve sore throats, help remove secretions and promote healing. You can make salt water by mixing half teaspoon of salt to a cup of warm water. Children must be old enough to gargle and they must spit out the water after gargling.
Do I need antibiotics?
Antibiotics are not usually needed to treat tonsillitis because tonsillitis is mostly caused by viruses (a viral infection). Antibiotics only work against bacteria (a bacterial infection) but not viruses.
Your healthcare provider may prescribe antibiotics for tonsillitis if:
- your symptoms are severe
- there's a high risk of you spreading the infection
- you're at high risk of getting rheumatic fever— for example Māori tamariki or Pasifika children or people living in crowded homes
- you have a weakened immune system
- you keep getting tonsillitis.
If you have confirmed group A strep throat (on a swab) or are at high risk of rheumatic fever, take the full course of antibiotics as directed by your healthcare provider. This is usually a 10 day course for liquid, capsule or tablet antibiotics. Some people who are swabbed and started on antibiotics may be asked to stop if the swab is negative for group A strep throat. Typically, a penicillin-based antibiotic course (eg, phenoxymethylpenicillin or amoxicillin) is used to treat strep throat. If you're allergic to penicillin, a non-penicillin option such as erythromycin may be used instead.
Surgery to remove your tonsils
An operation to remove your tonsils (tonsillectomy) may be considered if you often get tonsillitis. Read more about tonsillectomy.
Other children or family members should be kept away from the person with tonsillitis if possible. To prevent the spread of infection, use good hygiene measures:
- Wash your hands often and well.
- Use a tissue or the inside of your elbow to cover coughs and sneezes.
- Don't share eating utensils or cups or drink bottles.
- Clean surfaces well – particularly in the kitchen and bathroom
- Keep your home warm and dry – find out about Aotearoa New Zealand’s healthy homes initiative(external link) if you need help to keep your home warm and dry.
The following links provide further information about tonsillitis. Be aware that websites from other countries may have information that differs from Aotearoa New Zealand recommendations.
Sore throat(external link) Health New Zealand | Te Whatu Ora, NZ
Tonsillitis(external link) NHS, UK
Brochures
Virus action plan (adults)(external link) He Ako Hiringa, NZ
Virus action plan (child over 6 months)(external link) He Ako Hiringa, NZ
References
- Aotearoa New Zealand guidelines for the prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease(external link) Health New Zealand | Te Whatu Ora, NZ, 2024
- Australian guideline for the prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease (edition 3.3)(external link) Menzies School of Health Research (ARF/RHD writing group), Australia, 2025
- Sore throat(external link) Health New Zealand | Te Whatu Ora
- Sore throat(external link) Auckland Region HealthPathways, NZ, 2025
- Algorithm – assessment and management of sore throats in Aotearoa(external link) Heart Foundation, NZ, 2024
Aotearoa New Zealand guidelines for the prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease(external link) Health New Zealand | Te Whatu Ora, NZ, 2024
Australian guideline for the prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease (edition 3.3)(external link) Menzies School of Health Research (ARF/RHD writing group), Australia, 2025
Algorithm – assessment and management of sore throats in Aotearoa(external link) Heart Foundation, NZ, 2024
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Grace Lee, FRNZCGP and Clinical Educator
Last reviewed:





