You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Opioid medicines overview
Also called opioid analgesics or opiates
Key points about opioid medicines
- Opioid medicines are used to treat moderate to severe short-term pain, such as after an operation or serious injury.
- They are also used to treat pain caused by a terminal illness such as cancer.
- Common examples of opioid medicines include morphine, oxycodone, codeine and tramadol.
- Opioids are not recommended for the treatment of chronic (ongoing) pain that is not related to cancer. They are not very effective for this type of pain and there are risks of addiction.
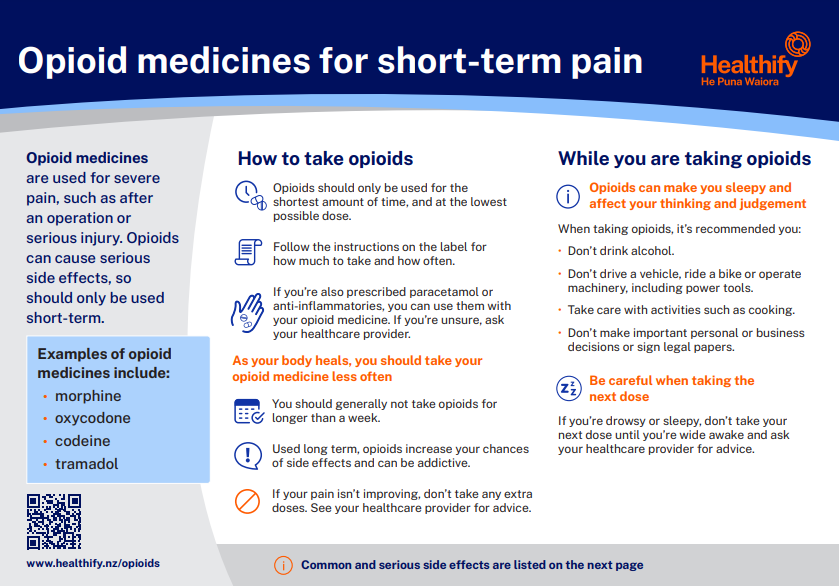
Opioid medicines are used for severe pain, such as after an operation or serious injury. Opioids can cause serious side effects, so should only be used short-term.
- Opioids work by binding to certain receptors in your brain and spinal cord. This decreases pain and your reaction to pain and increases your tolerance for pain.
- Opioids are prescribed when weaker pain medicines alone don't work well enough. See pain relief medications and opioids in palliative care.
- Opioids are not recommended for the treatment of chronic (ongoing) pain that's not related to cancer. They're not very effective for chronic pain, and there are risks of side effects and addiction. Read more about chronic pain.
Examples of opioids available in Aotearoa New Zealand
Opioids are divided into 2 groups – weak and strong opioids.
| Weak opioids | Strong opioids |
Factsheet: Opioids for short-term pain

|
Opioid medicines for short-term pain factsheet |
Opioids are available in different formulations
Opioids are available in different formulations, such as:
- a liquid or syrup
- quick-acting tablets and capsules
- slow-release tablets and capsules
- patches to put on your skin
- injections – which may be under your skin, into a vein or into a muscle.
Which opioid is best for me?
In Aotearoa New Zealand, opioids are available only on prescription. Your doctor will discuss the best option for you. There are many things that affect the choice of opioids, including the intensity and type of pain.
- Intensity of your pain: The weaker opioids such as codeine or dihydrocodeine are best for moderate pain, while the stronger opioids are used for more severe pain. The strong opioids differ a lot in strength; some of them are 10 times stronger than weaker opioids.
- Type of pain: Quick-acting tablets and capsules or liquids start working quickly to ease pain and are useful to treat sudden pain. Slow-release tablets and skin patches release the medicine slowly over several hours to give more even pain control. They're used when continuous pain relief is required. Injections may be used when tablets, capsules or liquids can't be taken or if immediate pain relief is needed.
Read more about opioids in palliative care.
Video: Opioids for short-term pain
Opioids should not be the first medicine you try for pain relief, if you have chronic (ongoing) non-cancer pain. They're not very effective for chronic pain and there are risks of side effects and addiction. It's important to try other treatment options such as lifestyle changes, self-management skills and other medicines. Read more about chronic pain.
The following video provides information to people who may be considering taking opioids for chronic (ongoing) non-cancer pain. This video is not for people taking opioids for cancer pain or palliative care. The video may take a few moments to load.
(NPS MedicineWise, Australia, 2020)
Opioids are strong medication with good pain relief but may cause harm from side effects and dependence. Here are a few tips on how to use opioids safely.
Dosing
- Follow the instructions on the pharmacy label for how much to take and how often.
- Don't increase your dose or take doses more often than prescribed without talking to your doctor first.
- If you’re drowsy or sleepy, don’t take your next dose until you’re wide awake and ask your healthcare provider for advice.
- Sometimes you may feel pain before your next dose is due. Talk to your doctor about this so your dose can be changed, or another pain relief option can be considered.
- If you’re also prescribed paracetamol or anti-inflammatories, you can use them with your opioid medicine. If you’re unsure, ask your healthcare provider.
- Opioids can become less effective with time. This is called tolerance. It means that your body has got used to the pain-relieving effect of the medicine, so you will need more to get the same effect. This is why your doctor needs to know exactly what dose you're taking.
Driving
- Opioids can cause drowsiness and confusion and can affect your ability to concentrate.
- You're more likely to feel drowsy at the start of treatment and when you have a dose increase.
- It's best not to drive if you have just started taking an opioid or if the dose has been recently increased.
- Once you are settled on the dose, and if you don't have any side effects that might affect your driving, you may be able to return to driving.
Alcohol
- Drinking alcohol as well as taking an opioid may increase drowsiness, especially at the start of treatment or when the dose is being increased.
- If you're drowsy, don't drive or operate machinery.
- It's better to drink less alcohol or avoid it completely if you're taking an opioid.
Stopping opioids
- If you've been taking opioids for a while, don't stop taking them suddenly without talking to your doctor. You may have withdrawal symptoms if you stop them or lower the dose too quickly.
- Withdrawal symptoms include tiredness, sweating, diarrhoea, restlessness and irritability.
- To avoid this, your doctor will reduce your dose gradually.
Eat plenty of fibre and drink more water
It might be hard or painful to have a bowel motion/poo (constipation). If this happens, ask your healthcare provider for a laxative, to soften your poo. Eating foods with fibre, drinking plenty of water and keeping active can help. Let your doctor know if you are feeling unwell or if you have tummy pain.
Try other ways to manage your pain
Opioids reduce strong pain but won’t take all of your pain away. Try relaxation techniques, gentle exercises and stretches. You may also be given other types of pain relief such as paracetamol and anti-inflammatories.
Tell all your healthcare providers you’re taking opioids
Opioids can affect some medicines. Ask your doctor or pharmacist if it’s safe to take any other medicines – especially those you take for pain, anxiety, sleep or depression.
If you’re breastfeeding
Don’t take opioids if you’re breastfeeding, unless advised by a specialist. Because opioids cause drowsiness, sleeping with your baby is dangerous. Put your baby to sleep in their own bed.
Be aware of the risk of dependence
If you have become dependent on your opioid medicine, your body starts to rely on them and you'll experience withdrawal symptoms if your dose is reduced or stopped. Dependence can occur within 1 month of starting to take an opioid. Read more about opioid withdrawal symptoms.
Although they may not realise it, the main reason some people continue to take opioids long-term is to avoid withdrawal symptoms. They mistakenly think the opioid is working to reduce pain, when in fact it’s only reducing withdrawal symptoms – which can include pain. The best way to prevent dependence is to use opioids for the shortest amount of time, and at the lowest possible dose.
As with all medicines, opioids can cause side effects, although not everyone gets them. Common side effects include the following:
| Side effects | What should I do? |
|---|---|
|
|
|
|
|
|
|
|
| Read more about medicines and side effects and reporting a reaction you think might be a side effect. | |
The following links provide further information about opioids. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Understanding morphine and other opioid medicine [PDF, 2.6 MB] Palliative Outcome Initiative, NZ
Managing non-cancer pain with opioid medicines [PDF, 208 KB] Choosing Wisely, NZ
Strong painkillers opioids(external link) Patient Info, UK
Risks of opioid medicines(external link) Medsafe, NZ
Resources
Risks of opioid medicines(external link) Medsafe and Ministry of Health, NZ, 2022 English(external link), te reo Māori(external link)
Managing non-cancer pain with opioid medicines Health Quality & Safety Commission, ANZCA and Choosing Wisely, NZ
Understanding morphine and other opioid medicines Palliative Outcome Initiative English, Korean, Samoan, Simplified Chinese, Tongan
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
Opioid pain relief(external link) MidCentral DHB, NZ, 2016
Opioid medicines for short-term pain [PDF, 105 KB] Healthify He Puna Waiora, NZ, 2023 English [PDF, 105 KB], te reo Māori [PDF, 126 KB]
Resource for healthcare providers
B-QuiCK: Prescribing opioids(external link) BPAC, NZ, 2024
Managing opioid-induced constipation(external link) BMJ visual summary, UK, 2017
References
- Opioids(external link) Health Quality and Safety Commission, NZ
- Opioid analgesics(external link) New Zealand Formulary
- Strong opioids for pain management in adults in palliative care(external link) BPAC, 2012, NZ
- Helping patients cope with chronic non-malignant pain – it’s not about opioids(external link) BPAC, 2014, NZ
- Opioid medicines and chronic non-cancer pain(external link) NPS Medicinewise , Australia
Brochures
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated:





