Naloxone for opioid overdose
Frequently asked questions about naloxone for opioid overdose
Key points about naloxone
- Naloxone is a medicine used to treat opioid overdose.
- If taken soon enough after an opioid overdose, it can save a life
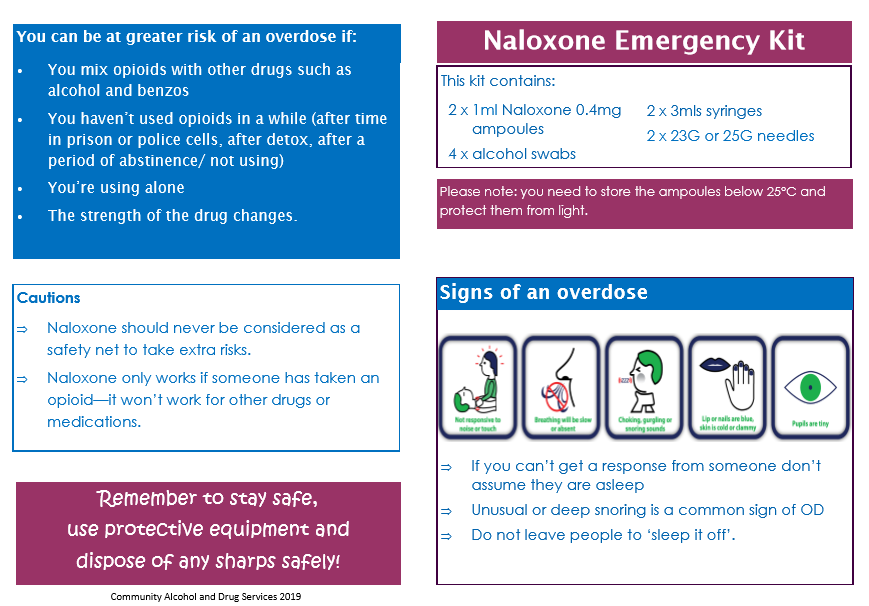
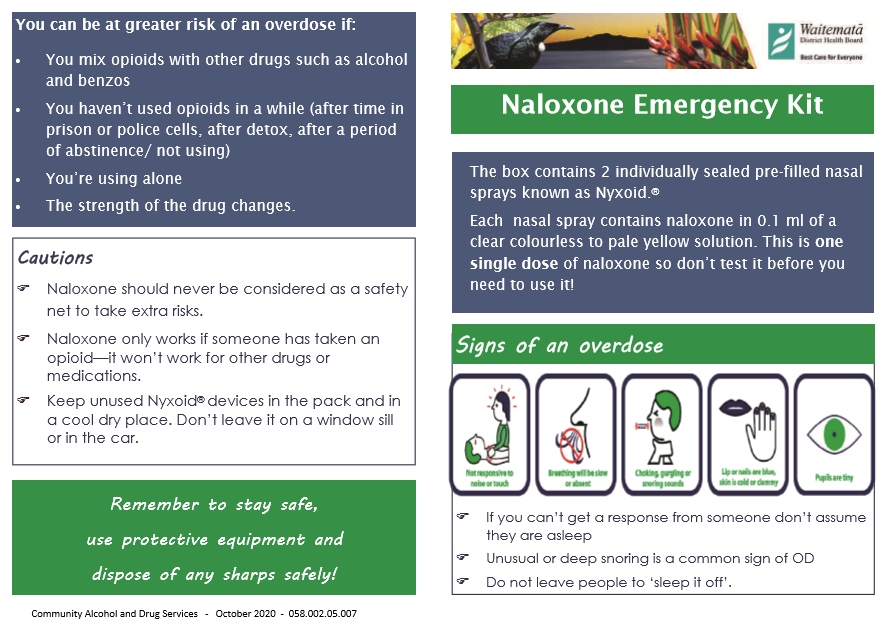
- In New Zealand naloxone is available as an emergency kit or take-home kit which can come as an injection or a nasal spray. These emergency kits are easy to use so anyone can give naloxone in an emergency.
- Find out how to use naloxone safely and possible side effects.

Naloxone is a medicine used to treat opioid overdose. Opioids are strong pain medicines, and drugs such as heroin. Examples of opioids include codeine, morphine, oxycodone, methadone, fentanyl, tramadol and heroin. Opioids slow your breathing and affect your consciousness – if you take too much or overdose on opioids, your breathing may stop and you could die. Read more about opioids and who is at risk of opioid overdose.
Naloxone works by reversing the effects of opioids. It can return normal breathing patterns to a person whose breathing has shallowed or stopped because of an opioid overdose. Naloxone can be given by injection or nasal spray and works very quickly, within 2–5 minutes.
| Opioid overdose is an emergency because it causes life-threatening problems such as slow or stopped breathing and unconsciousness. |
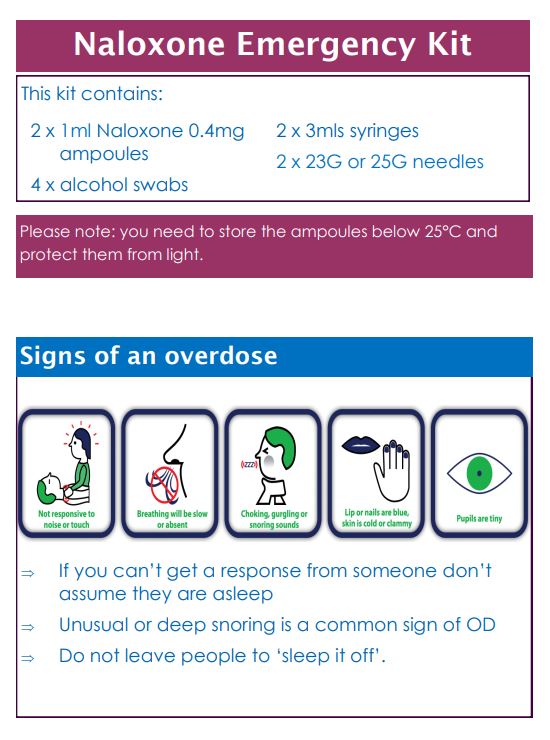
Naloxone is only used when a person shows signs of an opioid overdose. A person may have overdosed if they:
- are very sleepy or hard to wake up (passed out)
- have little or no breathing
- are snoring deeply or making gurgling sounds
- have blue lips or nails
- have tiny pupils.
Note: Naloxone is only effective against an opioid overdose. It doesn't work for an overdose of other types of medicines, illicit drugs or alcohol. But, in an emergency, if you don't know the exact cause of the overdose and think it could be from opioids, it is safe to use naloxone. See below can naloxone harm someone?
For detailed instructions on how to give naloxone see the leaflet in the emergency kit or the guides: Naloxone Injection Emergency Kit [PDF, 412 KB] and Naloxone Nasal Emergency Kit. [PDF, 294 KB]
| Here are some important things to remember when using naloxone |
|
An overdose is always an emergency. Even if naloxone has been given, always call for help.
Naloxone is active in the body for only 20–90 minutes, but the effects of most opioids can last longer. This means that the effects of naloxone are likely to wear off before the opioids are gone from the body, which could cause breathing to stop again. Naloxone may need to be used again, depending on the amount and type of opioids taken or the way they have been taken – either swallowed, inhaled or injected.
Naloxone injection is only available on prescription. It is best to contact your local alcohol and drug addiction support service. They will be able to advise you on where you can get a naloxone emergency kit from. Alcohol and drug addiction support service.(external link)
When collecting your naloxone kit, you may want to consider taking a friend or member of your whānau with you so they can support you and learn how to use the kit.
Naloxone nasal spray (Nyxoid) can be bought from a pharmacy without a prescription, but it is very expensive, and not all pharmacies have stock. It's best to call your pharmacy to get more information.
| If you are taking opioids, have a plan. Talk about overdose with people you trust before it happens. Ask your healthcare provider whether you need an emergency naloxone kit. |
|
Once you have the kit, always keep the naloxone in a place where family, friends, and close contacts can find it in an emergency. Let them know:
|
No. It is safe to give naloxone if you suspect an opioid overdose. It won't hurt if you are wrong about it being an overdose. People who receive naloxone for an overdose may wake up and go into withdrawal. Symptoms of withdrawal include:
- feeling nervous, restless or irritable
- body aches
- dizziness or weakness
- diarrhoea (runny poos), stomach pain or feeling a little sick
- fever, chills or goose bumps
- sneezing or runny nose
- anxiety
- fast heart beat
- confusion.
Talk to your healthcare provider if you have questions about withdrawal symptoms.
Very rarely, people who take opioids can have more serious side effects following naloxone such as seizures, pulmonary oedema, and ventricular arrhythmias if a large dose of naloxone is given.
Research has found that having naloxone available does not encourage people to use opioids more. The goal is to prevent deaths from opioid overdose by making naloxone available and educating people about how to prevent, recognise and intervene in overdose situations.
- Community Alcohol Drugs Support Auckland(external link) NZ
- NZ Drug Foundation(external link) NZ
- Alcohol Drug Helpline(external link) general freephone 0800 787 797, text 8681, Māori, Pacific Peoples, Youth helplines.
- Alcohol and drug services(external link) Health New Zealand | Te Whatu Ora
Nyxoid (naloxone nasal spray)(external link) Consumer information, NZ
DBL Naloxone hydrochloride injection(external link) Consumer information, AUS
Needle exchange services (external link) Drug Information Outreach, NZ
Maximising opioid safety(external link) Monash University, AUS
Risks of opioid medicines(external link) Medsafe, NZ
Resources
Naloxone injection pamphlet [PDF, 412 KB] Waitematā District Health Board (WDHB), NZ
Naloxone nasal pamphlet [PDF, 294 KB] Waitematā District Health Board (WDHB), NZ
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
- Naloxone hydrochloride(external link) NZ Formulary, NZ
- Having naloxone on hand can save a life during an opioid overdose(external link) Food and Drug Administration, US, 2019
- Naloxone nasal spray (Nyxoid) for opioid overdose(external link) NPS, Australia, 2020
- Take-home naloxone in Australian hospitals(external link) SHPA, Australia, 2020
Brochures
Waitematā District Health Board (WDHB), NZ
Waitematā District Health Board (WDHB), NZ
Community Alcohol and Drug Services, NZ, 2019
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated:





