You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Lowering my dose of opioid medicine
Also called opioid tapering
Key points about lowering opioid dose
- Taking opioids such as morphine, oxycodone or codeine for pain over a long time is not recommended, unless the pain is caused by cancer.
- If you have been taking opioids regularly or for a long time for non-cancer pain relief, work on a plan with your healthcare provider to lower your opioid dose gradually.
- Opioid pain medicines can be used to treat moderate to severe short-term pain, such as after an operation or serious injury, or ongoing pain from cancer or for palliative care.

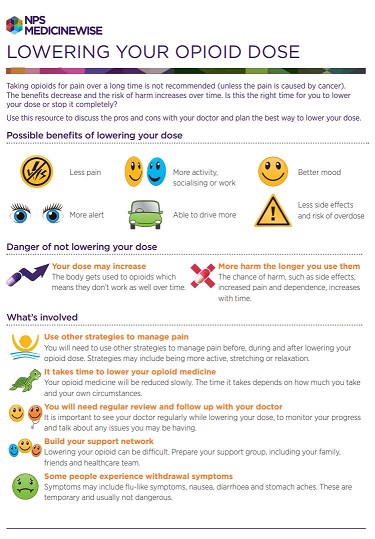
Taking opioids for pain over a long time is not recommended, unless the pain is caused by cancer. Over time the benefits decrease and the risk of harm increases.
- Your body gets used to opioids, which means they don’t work as well over time.
- The amount of relief from pain can reduce even at higher doses because of tolerance to the opioid.
- Sometimes opioids can actually cause your pain to get worse. This is called 'opioid-induced hyperalgesia'.
- The chance of side effects, and dependence, increases with time.
Read more about opioids and opioids in palliative care.
The benefits of gradually reducing or stopping opioids include:
- feeling more alert and in a better mood
- feeling able to do more activities, including socialising or work
- being able to drive safely (it's against the law to drive while impaired)
- reducing your risk of drowsiness and risk of falls
- experiencing less pain
- fewer side effects and reduced risk of overdose.
Develop a plan to lower your opioid dose
If you've been taking opioids for a long time for non-cancer pain relief, it's important that you make a plan with your healthcare provider to lower your opioid dose gradually, rather than suddenly stopping taking them. This is called tapering. Suddenly stopping opioids can cause severe withdrawal symptoms.
What is tapering?
Tapering is the gradual lowering of your dose or stopping your medicine in a planned way. This reduces the chances of withdrawal symptoms. Tapering includes the following steps:
- Understanding that it takes time to stop an opioid. Your opioid medicine will need to be reduced slowly. The time it takes depends on your dose and how you're coping.
- Having regular reviews with your healthcare provider to discuss how tapering is going. See your healthcare provider regularly to monitor your progress and talk about any issues you may be having.
- Building a support network. Lowering your opioid dose can be difficult. Prepare your support group, including your family/whānau, friends and healthcare team.
- Managing withdrawal symptoms if they happen. Some people have withdrawal symptoms. Symptoms may include flu-like symptoms, nausea, diarrhoea and stomach aches. These are temporary and usually not dangerous. Your healthcare provider may recommend reducing your dose more slowly if these happen and are difficult to manage.
- Using other strategies to manage pain. You'll need to use other strategies to manage pain before, during and after lowering your opioid dose. Strategies may include being more active, stretching, relaxation or breathing techniques.
Read more about lowering your opioid dose(external link).
Withdrawal symptoms can occur because of physical or psychological dependence, which can take as little as 1 month to develop. So when an opioid dose is lowered, you may experience a ‘withdrawal’, and your mind and body can respond negatively.
Therefore it's important that you reduce your opioid use slowly so that you don't get withdrawal symptoms or they are minimal.
Withdrawal symptoms vary for each person. They're usually quite different to how you feel when taking an opioid, eg, opioids can cause constipation, while withdrawal symptoms can include diarrhoea.
Symptoms may include:
- sweating
- nausea (feeling sick)
- tummy pain/cramping
- diarrhoea (runny poo)
- trouble sleeping
- muscle aches
- fast heartbeat
- anxiety
- runny nose
- goosebumps.
Withdrawal symptoms during tapering can last for 4 to 10 days. They feel unpleasant, but they're not dangerous.
How to manage withdrawal symptoms
Withdrawal symptoms are best managed together with your healthcare provider, who may prescribe medicines to treat symptoms such as nausea and vomiting. It’s important to have a responsible adult with you if you're having withdrawal symptoms to check that your medicines are taken correctly.
Unless advised otherwise by a healthcare provider, there are also strategies that may help with symptoms of opioid withdrawal. General strategies may include:
- relaxation and breathing techniques
- listening to music
- using distraction, such as talking to someone with a positive outlook
- being more active and stretching
- drinking plenty of water to replace any fluids lost through sweating and diarrhoea – people on restricted fluids should check with a healthcare provider about fluid intake.
Strategies and medicines for specific symptoms
These strategies may be helpful, and you can also ask your healthcare provider or pharmacist for advice:
- Nausea and vomiting: eat small, frequent meals, and bland food – avoid spicy, fatty or strong-smelling foods. Some people find ginger can help or your healthcare provider may prescribe a medicine called ondansetron.
- Gut cramps: hyoscine butybromide, a medicine you can buy from your pharmacy.
- Diarrhoea: loperamide, a medicine you can buy from your pharmacy.
- Headaches, muscle aches and pains: paracetamol and/or nonsteroidal anti-inflammatories (NSAIDs) such as ibuprofen oral tablets and gels or creams rubbed into the painful area. Ask your pharmacist if NSAIDs are suitable for you.
- Insomnia (inability to sleep): chamomile tea or sleep hygiene techniques. Read more tips to improve your sleep(external link) and find out more information and a workbook for keeping track of your sleep and sleep-related behaviour.(external link)
- Anxiety/agitation: lavender oil or another complementary medicine.
Opioid medicines and chronic non-cancer pain(external link) NPS Medicinewise, Australia
Brochures
Lowering your opioid dose(external link) NPS MedicineWise, Australia, 2019
Brochures
NPS MedicineWise, Australia, 2019

Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated: