| Common pain relievers | Description |
|---|---|
| Paracetamol | Paracetamol is used to treat mild-to-moderate pain.
|
| Non-steroidal anti-inflammatories |
NSAIDs are used to reduce mild-to-moderate pain and inflammation (swelling).
|
| Opioids | Opioids can be used for moderate-to-severe short-term pain such as after an injury or surgery, or for ongoing pain due to cancer.
|
Steroids
|
Some steroids are used for pain relief by reducing swelling and inflammation when other pain relievers are not effective alone or are not suitable.
|
| Antidepressants |
Tricyclic antidepressants are usually used to treat depression but low doses can relieve some types of chronic pain such as nerve pain. They have also been found to improve sleep and help with relaxation.
|
| Gabapentinoids |
|
| Muscle Relaxants |
|
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Pain relief medicines
Also called pain relievers or analgesics
Key points about pain relief medicines
- Pain relief medicines are best used for short-term pain usually because of surgery, injury or infection. They are usually only needed for a short time while the injury, surgery or infection is healing.
- There are a variety of medicines to relieve pain which can be grouped into different categories, depending on how they work.
- The choice of pain relief medicine can depend on many things, including the type, severity and cause of your pain, other medicines you may be taking and other health conditions you may have.

What is acute pain?
Acute pain usually occurs because of surgery, injury or infection, such as a dental infection or bone fracture (break). It often comes on quickly, lasts for a short time and goes away as the underlying cause resolves. Treatments usually only need to be given for a short time while the injury is healing.
- Paracetamol and NSAIDs are commonly used.
- Opioids are useful and usually only need to be given for a few days. The dose of opioid should be reduced as healing occurs.
- Read more about acute pain.
Severity of the pain
Pain is usually grouped into mild pain, moderate pain or severe pain. The step-wise or ladder approach to managing pain is based on the severity of your pain. It is a 3-step approach.
- Step 1: Mild-to-moderate pain
This type of pain is best treated with paracetamol, ibuprofen and other NSAIDs. Read more about paracetamol and NSAIDs. - Step 2: Moderate-to-severe pain
More intense pain is treated with mild opioid pain relievers such as codeine and tramadol. These may be used together with paracetamol or NSAIDs. - Step 3: Severe pain
Severe pain is treated with strong opioids such as morphine and oxycodone. These may be used together with paracetamol or NSAIDs. Read more about opioids.
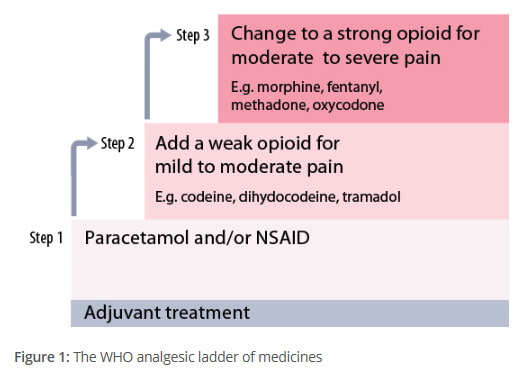
Image credit: Courtesy of BPAC(external link)
Nerve pain is a type of chronic pain from an injury to your nerves or nervous system. Types of nerve pain include sciatica from disc prolapse, nerve injury after spinal surgery, pain after infection such as shingles, pain with diabetes, pain after amputation (phantom limb pain or stump pain) and pain with multiple sclerosis or stroke.
- Medicines used to treat nerve pain include tricyclic antidepressants (amitriptyline, nortriptyline) and gabapentinoids (gabapentin, pregabalin).
- If these medicines help your pain, you can continue to take them for as long as you need to. If you do not feel any improvement in your pain after 6–8 weeks, speak to your doctor.
- Read more about nerve pain.
Chronic pain, also called persistent pain or long-term pain, is pain that lasts longer than 3 months. It is often described as pain that does not go away as expected after an injury or illness.
- Chronic pain is thought to occur when nerves become over-sensitive and send warning messages to your brain even when there is no injury, or the original injury causing pain has healed. In other words, the fire has been put out, but the fire alarm is still going off.
- Chronic pain is complex and can be difficult to treat. The aim of treatment is to find ways to support you and reduce the impact of the pain on your life.
- Medicines generally, and opioids in particular, are often not very effective for chronic pain because they do not greatly improve chronic pain levels or help you to be able to do the things you want to do. However, medication can be used in some situations alongside other strategies, such as physiotherapy, exercise, diet, relaxation, different ways of thinking and responding to pain (mindfulness and cognitive behaviour therapy), or other non-medicine treatments such as electrical stimulating techniques (TENS machine) and acupuncture.
- Read more about chronic pain and medicines for chronic pain.
Medical conditions
Some types of pain medication can worsen some medical conditions and should be avoided. For example, NSAIDS can make stomach ulcers worse, so if you have a history of stomach ulcers, you should avoid them. NSAIDs must also be used with caution by older adults and people with heart disease, type 2 diabetes or kidney problems.
Medications you are taking
Before taking medication for pain relief, it is important to ask if these may interact with medications that you are already taking for another condition. If you are unsure, check with your doctor or pharmacist.
Allergies
Some allergies may prevent you from taking certain types of pain relief medicines. For example, NSAIDs can cause allergic reactions in some people. Soon after taking the medicine, you may develop flushing, itchy rashes (hives), blocked and runny nose, and asthma (sometimes severe). If you have had hives (urticaria), nasal polyps or asthma, your risk of NSAID allergy is much higher compared to people without these conditions.
All medicines have side effects and risks. Sometimes the risks may be small and the benefit to your health may outweigh the risks, while in other cases the risks may be a problem and other medication may be safer. The best choice depends on your situation and the advice of your healthcare professional. Below is a list of the benefits and risks of different pain relief medicines.
Paracetamol
| Benefits and risks |
Benefits
|
Non-steroidal anti-inflammatory drugs (NSAIDs)
Such as ibuprofen, diclofenac, naproxen and celecoxib.
| Benefits and risks |
Benefits
|
Opioids
Such as morphine, codeine, tramadol and oxycodone.
| Benefits and risks |
Benefits
|
Steroids
Such as prednisone and triamcinolone. These may be given as tablets or an injection directly into a painful joint.
| Benefits and risks |
Benefits
|
Managing pain poster(external link) Waitematā DHB, NZ, 2016
Pain management plan(external link) BPAC NZ, 2022
Medicines for chronic pain(external link) Healthify He Puna Waiora and PHARMAC, NZ, 2018
Reducing chronic pain – what you can do to help yourself(external link) Healthify He Puna Waiora and PHARMAC, NZ, 2018
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
- The principles of managing acute pain in primary care(external link) BPAC, NZ, 2018
- Prescribing gabapentin and pregabalin: upcoming subsidy changes(external link) BPAC, NZ, 2018
- Managing patient with neuropathic pain(external link) BPAC, NZ, 2018
- Helping patients cope with chronic non-malignant pain – it's not about opioids(external link) BPAC, NZ, 2014
Brochures

Waitematā DHB, NZ, 2016

Pain management plan
BPAC NZ, 2022

Health Quality and Safety Commission, NZ, 2019
English, te reo MāoriCredits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated:





