Your respiration rate (breathing rate) is measured as the number of breaths you take in a minute. A typical adult takes 12 to 20 breaths each minute when they’re resting. Your breathing rate goes up when you exercise and should come back down to a resting rate afterwards. Read more about breathing rate.
Normal breathing is slow and regular – breathing in and out through your nose only. No effort should be visible, your diaphragm and belly should be moving gently.
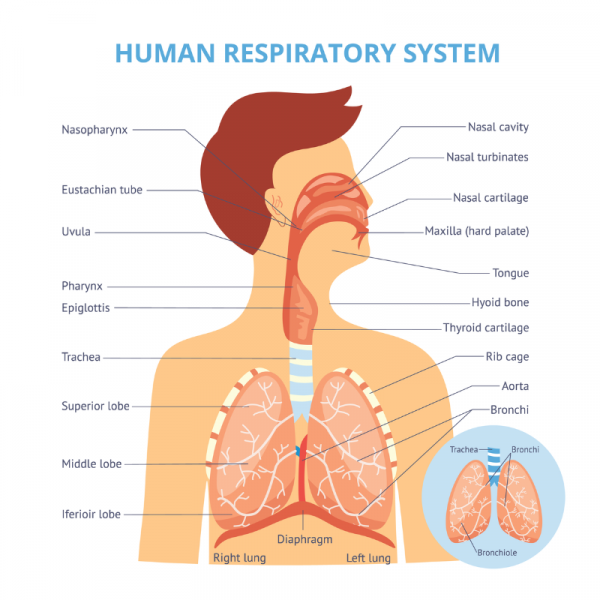
The main breathing muscles include your diaphragm, a dome shaped muscle below your lungs and above the organs in your abdomen or belly, and also the muscles between your ribs. Other muscles involved, known as accessory muscles, include some of your neck and shoulder muscles (eg, scalene or sternocleidomastoid or serratus muscles).
If you're in good health, your accessory muscles are not active during regular breathing. However, you may use these muscles when you're breathing hard or deliberately taking a deep breath. Breathing out or exhaling is generally passive (without active muscle activity) and is caused by the natural elastic recoil (or deflation) of your lung tissue accompanied by the relaxation of all breathing muscles.
The following video shows how your respiratory system works when you’re breathing in (inhaling) and out (exhaling).
Video: How do lungs work? Emma Bryce
Sometimes a normal breathing pattern is disrupted, such as by health conditions, an emotional response or pain. However, the atypical breathing pattern can become a habit without there being a cause for it and then it can become a breathing pattern disorder (see below). Next to over-breathing or hyperventilation you may develop a pattern of frequent deep sighing and over-use your chest or neck muscles rather than using your diaphragm.