Aims of treatment
While asthma can't be cured, the correct use of medicine combined with other self-care measures means that symptoms can be well controlled for most people.
Asthma treatment aims to keep your symptoms under control and prevent asthma attacks, or sudden worsening of symptoms. This is so that your asthma doesn't interfere with your daily activities and you can enjoy a full and active life.
Treatment
Treatment of asthma consists of inhaled medicines. It's crucial to receive good education on how to use the different inhalers properly.
There are 2 types of inhalers:
- Metered dose inhalers (MDIs), and
- dry powder inhalers.
MDIs are best used with a spacer to make sure the medicine is delivered to your small airways or breathing tubes.
Generally there are 2 main approaches to the treatment of asthma, depending on whether you are using a budesonide/formoterol inhaler or a steroid inhaler with/without long-acting bronchodilator.
Budesonide/formoterol
Examples of Budesonide/formoterol inhalers:
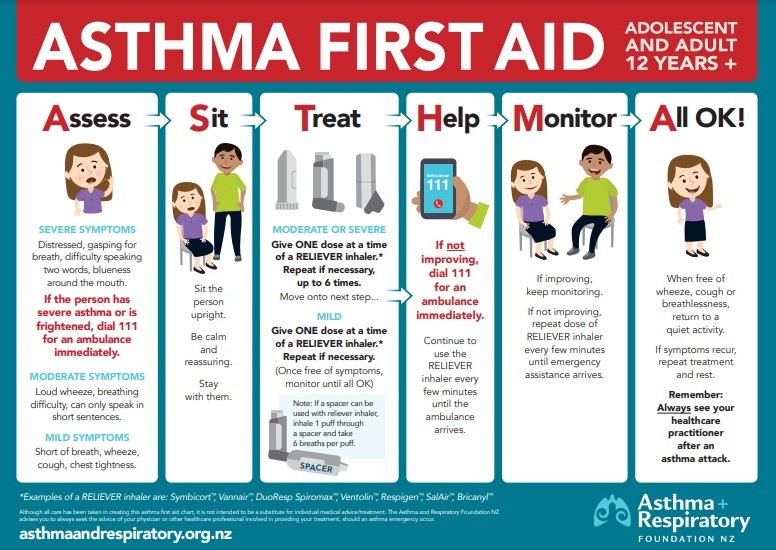
Mild symptoms
- Use budesonide/formoterol when required for relief of asthma.
- This is also called anti-inflammatory reliever (AIR) therapy or single-inhaler maintenance and reliever (SMART) therapy.
Moderate to severe symptoms
- Use budesonide/formoterol every day PLUS when required for relief of asthma symptoms.
- Also called single-inhaler maintenance and reliever (SMART) therapy.
Steroid inhaler with/without long-acting bronchodilator
Mild symptoms
- Use your steroid inhaler every day, even when you're not having symptoms.
- Examples of steroid inhalers include:
- Use salbutamol or terbutaline for symptom relief when needed.
- If you’re using them more than twice a week, see your healthcare provider to review your treatment.
Moderate to severe symptoms
- Use your steroid inhaler PLUS long-acting bronchodilator every day, even when you're not having symptoms.
- For examples of steroid inhalers and long-acting bronchodilator inhalers, see asthma medications.
- Use salbutamol or terbutaline for symptom relief.
- If you're are using them more than twice a week, see your healthcare provider to review your treatment.
For severe flare ups or exacerbations of asthma or for asthma attacks your healthcare provider will prescribe prednisone for a short period. Prednisone is a tablet to help reduce inflammation. It shouldn't generally be used long term for asthma treatment. If you need prednisone regularly each year you should be referred to a specialist clinic. Extra inhaler treatment might be needed or, for some people, new generation biological treatments (eg, benralizumab, mepolizumab).
After each flare up you should have your inhalers reviewed – including your preventer treatment and your asthma action plan.
There are other less commonly used medicines for asthma prevention such as montelukast tablets.
Flu and COVID-19 vaccines
People with asthma are at increased risk of complications from the flu, even if their symptoms are mild or well-controlled by medicine. Complications include pneumonia (lung infection), heart failure and worsening asthma symptoms. The flu is also associated with increased risk of hospitalisation for people with asthma.
- Ask your healthcare provider about getting the flu vaccination to reduce your risk of flu.
- The flu vaccine is usually free for people with asthma, if you are on regular preventative therapy.
- It is best to get vaccinated before the start of the winter season, before the flu enters the community.
- It’s important to get the flu jab every year because each year the flu vaccine is developed to match the different strains of flu virus you are likely to come across.
- Have your COVID-19 booster vaccination if you can.
- Some people are eligible for the respiratory syncytial virus (RSV) vaccine.
- Read more about influenza and the flu vaccine and the COVID-19 vaccine.