Chronic pain is complicated and often doesn't respond to treatments aimed at reducing pain. Where possible, treatments to reduce pain may be offered, but the focus is always on increasing your ability to do the things you want to do. Medicines can be part of your pain management plan, but in general they’re not very effective for reducing chronic pain and often have unpleasant side effects. Some types of chronic pain don't respond to medicines that are helpful for acute pain. Fortunately, there are a number of other strategies to help you live well with pain.
Video: Tips for managing chronic pain
This video may take a few moments to load.
(Healthify He Puna Waiora, NZ, 2018)
Understand what affects your pain
Being informed about pain, and any disease or injury processes involved, and learning about what affects your pain helps you build a personal understanding of what might be going on. It helps to know that you're safe to move because your pain and what's going on in your body are not well related. Getting to know what affects your pain means you can make decisions about whether it’s worth doing something that's important to you – even if your pain may increase. Knowing what settles your pain down means you can use these strategies at times when your pain flares up.
Learn to make room for pain
It can be tempting to look for ways to reduce your pain, but doing this can make it difficult to keep involved in what matters in your life. It helps to weigh up the good (and not so good) in both the short-term and long-term when deciding how much effort to put into reducing or controlling pain intensity. Making room for pain doesn't mean giving up, but it acknowledges the reality that pain is currently part of your life. If you know that you're not doing harm to your body, you can judge whether doing something is worth it even if your pain may increase. Learning ways to calm your nervous system down can help you deal with times when your pain fluctuates.
Stay active
For most types of pain, moving more and doing regular movement practices (eg, walking, swimming, dancing and stretching) can help you keep doing what you value. Short movement 'snacks' throughout the day can be more sustainable than trying to do a larger amount of movement once a week. Using different types of movement activities means you can choose what works for you depending on what else is going on in your life. Ask a member of your healthcare team to help you create a plan for regular movement practices. See our care planning and care plans page to learn how your team and whānau can work with you to make a plan.
Pace yourself
Chronic pain can lead you to re-evaluate your priorities, and create opportunities to think about your pace of life. It can be helpful to look at your week to find ways to have a consistent level of activity. Over-doing things on a day when you feel well can lead you to under-doing the next day, making it hard to make plans. Breaking your daily activities into ‘chunks’ gives you opportunities to change the intensity, movements, and positions you’re in.
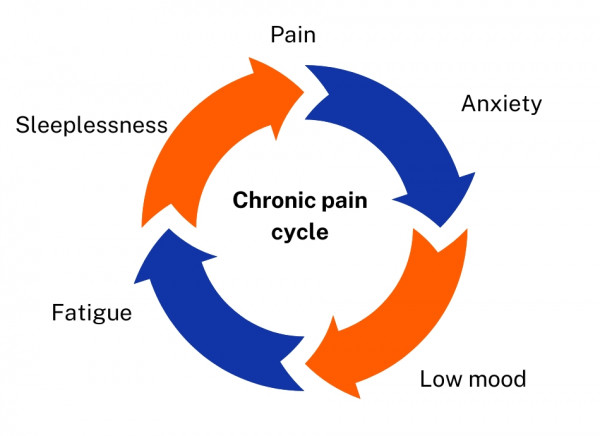
Identify strategies to help you manage stress
Stress can affect your pain and, because pain is stressful, even small stresses can be more difficult to deal with. Healthy stress management practices can help you to cope more effectively with your chronic pain. Problem-solving, communicating your needs, using movement practices, working on sleep, eating healthily, connecting with others and having fun all help with stress. Read more about managing stress.
Do things you enjoy
Doing activities you enjoy can help reduce stress, tension and anxiety, and keep you involved in life. Having a range of activities from relaxing to energetic – alone and with others – gives you options even in times when your pain fluctuates.
Learn about mindfulness
Mindfulness reduces stress, tension and anxiety. People who practice mindfulness can find they worry less about their pain, and can find ways to calm their nervous system down. Read more about mindfulness.
Have a support network
Engage whānau and friends to help you manage your pain. Join a support group or find a hobby that makes you feel good and helps you connect with family, friends or other people. Connecting with healthcare providers who know and understand about chronic pain, and who you feel comfortable with, can be helpful – especially when navigating the health system. Being engaged and connected can help you feel more positive and experience less pain.
Do a pain-management programme
Doing a pain-management programme is a useful way to learn about your pain. Ask your healthcare team if there's a self-management or pain programme in your area. Or you could do an online course, eg, the free Retrain Pain course(external link) from the Retrain Pain Foundation. You can also view the New Zealand version of the Pain Self-Care Toolkit or visit the Pain Toolkit website(external link) and app for more resources.
Apps
Read about some pain management apps that have been reviewed by Healthify.
Consider non-medicine treatments
Chronic pain is best managed with a person-centred approach that takes into account the physical, psychological and environmental factors that influence your experience of pain. This usually involves the use of self-management strategies. Often people find they develop these strategies best when supported by a team of health professionals from different backgrounds (a multidisciplinary team or MDT).
There are a variety of non-medicine-based treatment options to manage pain, including massage, acupuncture, TENS and psychological therapies. Some have limited scientific evidence about their effectiveness and not all of these will be suitable for everyone. Read more about non-medicine treatments for chronic pain.
If your pain persists and is affecting what you can do, ask your healthcare provider about a referral to your local pain service, a pain specialist or pain programme.
Pain relief medicines
Most pain relief medicines are not very effective in treating chronic pain and when used long-term, can have more side effects. However, there are some medicines that can be used alongside self-management strategies. Read more about medicines for chronic pain.
Apps reviewed by Healthify
You may find it useful to look at some Pain management apps and Physiotherapy and exercise apps.