Fibromyalgia | Mate tārūrū
.
Key points about fibromyalgia
- Fibromyalgia (mate tārūrū) is a condition where pain and stiffness is felt around your joints and in your muscles and bones.
- Symptoms include widespread pain, fatigue and sleep disturbances.
- A good first step for self-management is to learn more about how pain is produced by your body.
- Treatment aims to improve your sleep, increase your ability to do the things you want to do while also reducing your pain.

- Fibromyalgia is a term used to describe widespread pain and tenderness in different areas of your body.
- It is thought to be a disorder of the way your brain and nervous system receive and interpret signals for your body, resulting in pain.
- Fibromyalgia is very common, with a prevalence of about 2%. Women are 7 times more likely than men to be affected.
- Fibromyalgia is a long-term (chronic) condition – pain and discomfort often extends beyond 3 months. There may be periods when symptoms flare up or times when they become more manageable.
- People with fibromyalgia often experience other symptoms, eg, fatigue, poor sleep, difficulty concentrating and sensitivity of their bladder and bowels.
- Fibromyalgia can be hard to understand and difficult to explain to those close to you. Some people might find the diagnosis difficult to accept. Most people find ways to feel well and take note of what exacerbates their symptoms, so they can continue to do what they love while living with fibromyalgia.
- The goals of treatment are to avoid triggers that flare up bouts of pain and to feel supported in activities that improve your sleep and increase your ability to do the things you want to do, while also reducing your pain and other symptoms.
- Medicines are not effective in treating fibromyalgia but may play a role in reducing the associated symptoms. With the right combination of therapies and lifestyle changes, it's possible to live well and manage the symptoms of fibromyalgia.
Fibromyalgia is not your fault
You haven't caused this condition yourself, nor is it 'caused' by anxiety or depression. Instead, recurring pain is a neurophysiological problem of the nervous system or pain system that can be identified and treated.
- Your pain and/or symptoms are totally real – they're not made up or in your head.
- It's not your fault that you have fibromyalgia.
- You're not psychologically unwell.

Image credit: Canva
What it is
Fibromyalgia is a condition where people experience multiple tender or painful areas across the body that don't clearly follow a pattern of previous injury and are not explained by another condition. While much is still to be learnt about fibromyalgia, it's thought to be a disorder of the way the brain and nervous system receive and interpret signals from the body, resulting in felt sensation of pain.
Previously, fibromyalgia was called myofibrositis, but no clear link between inflammation (which the suffix ‘itis’ refers to) and the disorder has been found. No other biochemical or tissue markers have been identified either to assist in understanding the cause or for assisting in the diagnosis of fibromyalgia.
The main neurophysiological problem appears to be what is known as ‘central sensitization’, where your nervous system (below the level of voluntary or conscious control) has become over-active, out of proportion to what is usually required. A common metaphor is that it is a bit a like a faulty fire-alarm, going off when there is no fire.
It's likely that fibromyalgia is a dysfunction of how the central nervous system (brain and spinal cord) processes pain which may contribute to the severe fatigue that's also often experienced. Fibromyalgia and myofascial pain syndrome are not exactly the same, but they're similar in that they are both “central pain” syndromes. Myofascial pain syndrome involves mostly muscle pain, and fibromyalgia causes more widespread body pain as well as other symptoms.
While fibromyalgia doesn't cause joint inflammation, there have been small studies demonstrating differences in the function of pain receptors, the regulation of reward and stress hormones, and even the structure of the brain for people affected by fibromyalgia. This research is ongoing but supports the benefits of current recommended treatments. See the treatment section below.
What it isn't
Fibromyalgia is not an autoimmune disorder, but people who have fibromyalgia may also have chronic inflammatory or autoimmune disorders.
Fibromyalgia is different to polymyalgia rheumatica (PMR), a type of inflammatory arthritis with similar symptoms. PMR mainly affects older people and responds well to anti-inflammatory medicines.
What causes it
There's no single cause of fibromyalgia. Researchers think it may involve genetic and environmental factors, alone or in combination. For example, factors including infectious illness, physical trauma, emotional trauma or hormonal changes may contribute to the generalised pain, fatigue and sleep disturbances. However, for many people, fibromyalgia starts without any obvious cause.
Fortunately, fibromyalgia doesn't directly cause further serious illness and there's no indication that it causes ongoing harm to your body. Nonetheless, persistent symptoms can be distressing or disruptive and can greatly affect some people.
Pain
The main symptom of fibromyalgia is widespread pain. Some degree of pain may always be present and may be associated with fatigue and stiffness. People with fibromyalgia often say the pain begins or flares in 1 area and spreads to others. It may be exacerbated (made worse) by physical tasks, illness or stressful situations.
You're encouraged to track your “triggers” to minimise these or find sustainable ways of completing tasks you wish to. Lifestyle changes, (eg, alterations to your home, car or workplace) may help to manage your pain. Many people find mindfulness, regular exercise or psychotherapy assist with living alongside the symptoms. Understanding the mechanisms of chronic pain provides a useful rationale for why these activities can be beneficial.
Fatigue
Most people with fibromyalgia have fatigue and the kind of tiredness felt with flu or lack of sleep. Sometimes the fatigue is severe and is a greater problem than the pain. Tiredness may always be present or it may ‘sweep’ over you in waves.
Tender points
A characteristic of fibromyalgia is a number of ‘tender points’ at common locations in your body. A muscle examination reveals these tender areas which can be extremely painful when pressed but otherwise may not hurt at all. You may not even be aware of the presence of these tender points until a doctor performs a ‘tender point evaluation’. These tender points are not required for a diagnosis of fibromyalgia, although researchers may use them to identify who might participate in a research study.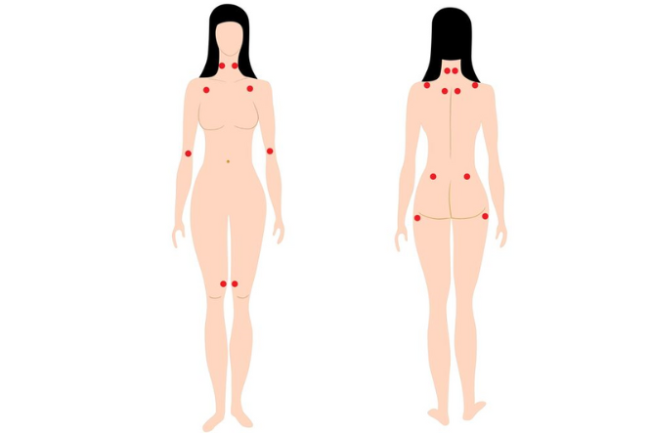
Image credit: 123rf
Problems with thinking
Researchers have found that people with fibromyalgia are more likely than others to have their cognition (thinking) affected. This can include problems with memory, concentration and decision-making. This is known as 'fibro fog'. It's also associated with illnesses that have central sensitisation as a significant feature, eg myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) or other chronic primary pain syndromes, eg, chronic pelvic pain.
Experiencing ‘fibro fog’ may make it difficult to do things you would like to do, and may make you feel frustrated or depressed. Depression can also make the ‘fibro fog’ worse, so if you experience both you may find ‘fibro fog’ to be a significant problem.
Sleep disturbances
Sleeping problems are common and you can wake up feeling tired, even after sleeping through the night. This tiredness can range from becoming fatigued quickly, to exhaustion – it can vary from one day to the next. Disturbed sleep is also common.
Depression and anxiety
It's more common for people with long-term pain conditions to also experience depression and/or anxiety, because of how pain can affect your life. This doesn't mean that fibromyalgia symptoms are an indication of mental illness, nor that a mental illness has caused fibromyalgia.
Some of the therapies for mental health conditions and fibromyalgia overlap where the focus is to improve satisfaction and quality of life. Improving mental health with therapy and/or medicine may greatly improve your ability to manage the symptoms of fibromyalgia.
Other symptoms
You may experience:
- headaches (especially migraine and tension headaches)
- abdominal pain
- muscle tension
- allergies
- dry eyes
- tender lymph nodes
- irritable bowel syndrome
- an overactive bladder.
Fibromyalgia is common. About 2% of the world’s population experience it (1 in 50) and it's about 7 times more common among women. It usually affects young or middle-aged women but can also occur in men, children and adolescents.
It doesn't seem that fibromyalgia is inherited, but you're at a greater risk of developing fibromyalgia if one of your parents or siblings also has the condition.
There's evidence that people with other rheumatology conditions (eg, rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis) may be at greater risk of developing fibromyalgia as well, but this doesn't mean they cause fibromyalgia.
Fibromyalgia is diagnosed, usually by a GP, based on your symptoms, a physical examination (which may include checking for tender points) and tests to exclude other causes of ongoing pain and fatigue.
Fibromyalgia is diagnosed based on criteria that include:
- having experienced widespread pain that's been present for at least 3 months
- sleep disturbance
- feeling “foggy” in your head.
A diagnosis is only made when other possible causes of these symptoms have been eliminated. There is no blood test, X-ray or scan to diagnose for fibromyalgia.
Occasionally, tests may reveal other health conditions or deficiencies (not related to fibromyalgia) that need to be treated. These will be managed by your healthcare provider and you may receive a diagnosis of fibromyalgia as well depending on what happens to your symptoms with treatment over time.
There has been a lot of research into chronic pain over the last 20 or so years, and this knowledge is now gradually finding its way into clinical practice of both doctors and other health professionals. However you may need to find a health professional who understands the modern neuroscience and who can explain it to you.
So an important first step is to learn more about how pain is produced by the body. Persistent pain clinics (whether in public or private health systems) can provide this sort of understanding, especially if you join one of the well-facilitated treatment groups.
Most people live well with fibromyalgia once they have learned ways of coping with the problems it can pose – even if the pain is still there.
The goals of treatment are to improve your sleep, increase your ability to do the things you want to do, while also reducing your pain as much as possible. For many people, a unique combination of these recommended treatments and even additional treatments are required so it's important to work with your healthcare provider in creating a plan to move forward.
Self-management
Fibromyalgia can persist throughout your life, however it's possible to live well and manage the symptoms through self-help techniques, therapy and occasionally with the use of some medicines. Guidelines from Europe and Canada suggest the most effective, evidence-based treatments include the following. These activities are logical conclusions from understanding how pain is generated.
Exercise
- Exercise can lift your mood, promote muscle health, improve blood flow, ease digestive symptoms and help regulate hormonal patterns which help with sleep.
- With fibromyalgia, it can be challenging to exercise if you are in pain. The key is to start at a low level, and gradually increase.
- Ideally, you should work with an exercise professional or physiotherapist to create a plan that includes low impact stretching, strengthening and aerobic exercises for cardiovascular health.
- Water based exercise plans (eg, aquaerobics and swimming classes) have the best evidence for reducing symptoms associated with Fibromyalgia.
- Other forms of exercise that have shown some benefit in fibromyalgia include tai chi and yoga. Trials have shown tai chi to result in similar or greater symptomatic improvement as aerobic exercise.
Relaxation techniques
- Relaxation therapies, eg, acupuncture, massage, infra-red heat, hot packs and manipulation may help ease symptoms associated with fibromyalgia (eg, muscle tension, fatigue, poor sleep, depression or anxiety).
Psychological therapies and counselling
- Cognitive behavioural therapy (CBT) has been shown to reduce pain and disability in a sustainable way.
- Working with a health professional, eg, health improvement practitioner (HIP), psychologist, or counsellor, can help support you in adjusting to your diagnosis and planning for living life with fibromyalgia.
Activity management and preventing triggers
- Maintaining a regular pattern of activity and rest can reduce the peaks and troughs of fluctuating fatigue and pain. This means planning daily and weekly schedules.
- A HIP or occupational therapist can help you adapt your daily routine.
Reducing stress
- As with most health conditions, stress can aggravate your symptoms.
- While stress is often an unavoidable part of life, it's important to look at ways you can reduce your exposure to stress and its effects.
- Read more about beating stress.
Mindfulness
- Learning a variety of ways to relax reduces pain and promotes restful sleep.
- Mindfulness reduces stress, tension and anxiety. It can help you to reframe your symptoms and to direct your thoughts in a way that is helpful for everyday life.
- Read more about mindfulness.
Medicines
Medicines may be useful for treating pain and fatigue associated with fibromyalgia.
- Traditional pain relief (eg, paracetamol, ibuprofen) are unlikely to effectively treat symptoms but may be something that's worked well for you in the past.
- Medicines that work on the brain to alter the perception of pain (eg, low dose tricyclics) may be effective in reducing the symptoms. Other medicines may be considered by your doctor depending on your symptoms and other aspects of your health.
- The class of medicines including gabapentin are only helpful for a few people, so if you're considering them, try them for a time-limited period only and stop them if they haven't substantially improved your symptoms.
- Medicines to treat other symptoms that may go along with fibromyalgia (eg, depression, anxiety, bladder irritability) are available and may be helpful.
- Opioids (morphine, codeine, tramadol, fentanyl) are not indicated for fibromyalgia. Unfortunately many people use opioids without any long-term benefit. This is because opioids are only effective for pain from acute injury or cancer. They're not effective in central sensitisation and may cause further problems.
As with all medicines, the side effects may cause more issues or discomfort than the symptom they treat therefore it's important to discuss these things with your healthcare provider:
- Any concerns you have.
- New symptoms.
- Medicines that could also be prescribed to reduce their risk of harm (eg, taking omeprazole if you're taking anti-inflammatories).
Read more about how chronic pain is treated and non-medicine treatments for pain.
Apps reviewed by Healthify
You may find it useful to look at some Pain management apps and Meditation and mindfulness apps.
If you've been diagnosed with fibromyalgia, you may have some concerns about telling any healthcare providers you see about your condition. However, they are better able to support and treat you if they know your full medical history. It's important to know that:
- Fibromyalgia isn't responsible for the development of other conditions and is unlikely to make them worse.
- If you suffer an injury, become unwell or require surgery you should still receive pain relief where indicated for your condition. Discuss this with your healthcare team.
- A diagnosis of fibromyalgia won't stop you having investigation, diagnosis and treatment of other conditions.
Complex chronic illness support(external link) Phone 07 281 1481. Information, support and practical advice for people, families and carers affected by fibromyalgia.
Arthritis New Zealand(external link) provides support for people with arthritis as well as those with conditions that aren't always classified as types of arthritis, including fibromyalgia. Freephone 0800 663 463.
Fibromyalgia Facebook Support Group(external link) Arthritis NZ
Fibromyalgia(external link) Arthritis NZ
Physical activity(external link) Arthritis NZ
Complex chronic illness support(external link)
Apps
Pain management apps
Meditation and mindfulness apps
Brochure
Fibromyalgia(external link) Arthritis New Zealand
References
- Fitzcharles M-A, Ste-Marie PA, Goldenbery DL, et al. 2012 Canadian guidelines for the diagnosis and management of fibromyalgia syndrome – executive summary(external link) Pain Res Manag 2013;18(3):119–126
- Macfarlane GJ, Kronisch C, Dean LE, et al. EULAR revised recommendations for the management of fibromyalgia(external link) Ann Rheum Dis 2017;76:318-328
- Bidonde J, Busch AJ, Schachter CL, et al. Aerobic exercise training for adults with fibromyalgia(external link) Cochrane Database of Systematic Reviews, 2017
- Løge-Hagen JS, Sæle A, Juhl C, et al. Prevalence of depressive disorder among patients with fibromyalgia – systematic review and meta-analysis(external link) J Affect Dis 2019;245:1098–1105
- Bhargava J, Hurley JA. Fibromyalgia(external link) StatPearls Publishing, US, 2022
- Wang C, Schmid CH, Fielding RA, et al. Effect of tai chi versus aerobic exercise for fibromyalgia – comparative effectiveness randomized controlled trial(external link) BMJ (Clinical research ed.) 2018;360:k851
- Busch AJ, Webber SC, Richards RS, et al. Resistance exercise training for fibromyalgia(external link). Cochrane Database of Systematic Reviews, 2013
- Bidonde J, Busch AJ, Webber SC, et al. Aquatic exercise training for fibromyalgia(external link) Cochrane Database of Systematic Reviews, 2014
- Häuser W, Klose P, Langhorst J, et al. usch, A. (2010). Efficacy of different types of aerobic exercise in fibromyalgia syndrome – a systematic review and meta-analysis of randomised controlled trials(external link) Arthritis Res Ther 2010;12(3):R79.
Brochures
Arthritis NZ, 2014

Te Kete Haerenga – Wellness Toolkit
Healthify He Puna Waiora, NZ, 2022
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Hamish Wilson, Associate Professor, Department of General Practice and Rural Health, University of Otago
Last reviewed:





