If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Overactive bladder
Also known as irritable bladder or detrusor instability
Key points about overactive bladder
- An overactive bladder is when your bladder contracts suddenly without you having control, and when it's not full.
- It's a common condition where no cause can be found for the repeated and uncontrolled bladder contractions. For example, it's not due to a urine infection or an enlarged prostate gland.
- Overactive bladder syndrome is sometimes called an irritable bladder or detrusor instability (detrusor is the name of a bladder muscle).
- Treatment includes bladder training, medicines and, in some cases, surgery.

Your kidneys make urine all the time. A trickle of urine is constantly passing to the bladder down the ureters, the tubes from the kidneys to the bladder. You make different amounts of urine depending on how much you drink, eat and sweat.
The bladder is made of muscle and stores the urine. It expands like a balloon as it fills with urine. The outlet for urine, the urethra, is normally kept closed. This is helped by the muscles beneath the bladder that sweep around the urethra, the pelvic floor muscles. 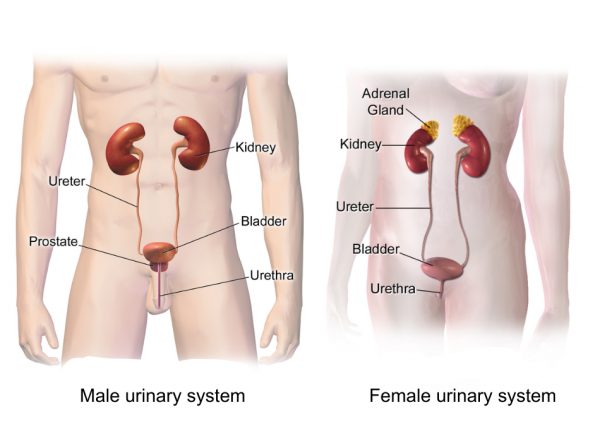
Image credit: Wikimedia Commons
When a certain amount of urine is in the bladder, you become aware that the bladder is getting full. When you go to the toilet to pass urine, the bladder muscle squeezes (contracts) and the urethra and pelvic floor muscles relax.
Complex nerve messages are sent between the brain, the bladder, and the pelvic floor muscles. These tell you how full your bladder is, and tell the right muscles to contract or relax at the right time.
An overactive bladder is when your bladder contracts suddenly without you having control, and when your bladder isn't full. Overactive bladder syndrome is a common condition where no cause can be found for the repeated and uncontrolled bladder contractions. For example, it's not due to a urine infection or an enlarged prostate gland.
Overactive bladder syndrome is sometimes called an irritable bladder or detrusor instability. Detrusor is the medical name for the bladder muscle.
The cause is not fully understood. The bladder muscle seems to become overactive and contract when you don't want it to. Normally, the bladder muscle is relaxed as the bladder gradually fills up. As the bladder is gradually stretched, we get a feeling of wanting to pass urine when the bladder is about half full.
Most people can hold on quite easily for some time after this initial feeling until a convenient time to go to the toilet. However, in people with an overactive bladder, the bladder muscle seems to give wrong messages to the brain. The bladder may feel fuller than it actually is. The bladder contracts too early when it is not very full, and not when you want it to. This can make you suddenly need the toilet. In effect, you have much less control over when your bladder contracts to pass urine.
In most cases, the reason why an overactive bladder develops isn't known. This is called overactive bladder syndrome. Symptoms may get worse at times of stress. Symptoms may also be made worse by caffeine in tea, coffee, cola, etc, and by alcohol (see below).
In some cases, symptoms of an overactive bladder develop as a complication of a nerve- or brain-related disease such as following a stroke, with Parkinson's disease, with multiple sclerosis or after spinal cord injury. Also, similar symptoms may occur if you have a urine infection or a stone in your bladder. These conditions are not classed as overactive bladder syndrome as they have a known cause.
How common is the problem?
Approximately 1.1 million New Zealanders don't have full bladder control and experience leakage of urine, in amounts that vary from a few drops to large volumes, twice or more a month. Overactive bladder is one of the causes of these symptoms and it can affect both men and women. In 2 large studies it was found that about 1 in 6 adults reported some symptoms of an overactive bladder. Symptoms vary in their severity. About 1 in 3 people with an overactive bladder have episodes of urge incontinence.
Incontinence in particular can be embarrassing for the person and many people don't seek the help that's available, thinking that nothing can be done for them. However, most men and women with overactive bladder can be helped, so it's important to talk about any bladder problems with your healthcare provider.
- Urgency: This means that you get a sudden urgent need to pass urine. You are not able to put off going to the toilet.
- Frequency: This means going to the toilet often – more than seven times a day. In many cases it is a lot more than seven times a day.
- Nocturia: This means waking to go to the toilet more than once at night.
- Urge incontinence: This is a leaking of urine before you can get to the toilet when you have a feeling of urgency.
- Bladder training is a main treatment. This can work well in up to half of cases.
- Pelvic floor exercises may also be advised for some people.
- Medication may be advised instead of, or in addition to, bladder training.
- Surgery is sometimes recommended if the above methods have been unsuccessful.
Bladder training – sometimes called bladder drill
The aim of bladder training is to slowly stretch the bladder so that it can hold larger and larger volumes of urine. In time, the bladder muscle should become less overactive and you should become more in control of your bladder. This means that more time can pass between feeling the need to pass urine, and having to get to a toilet. Leaks of urine are then less likely. A doctor, nurse or continence advisor will explain how to do bladder training. Read more about bladder training.
Pelvic floor exercises
Many people have a mixture of overactive bladder syndrome and stress incontinence. Stress incontinence is urine leakage during physical exertion that raises abdominal pressure (eg, coughing, sneezing, exercising or lifting). If you have weak pelvic floor and urethral muscles this can force urine out of your urethra. Pelvic floor exercises are the main treatment for stress incontinence. Briefly, this treatment involves exercises to strengthen the muscles that wrap underneath your bladder, uterus (womb) and rectum.
It's not clear if pelvic floor exercises help if you just have overactive bladder syndrome without stress incontinence. However, pelvic floor exercises may help if you are doing bladder training. Read more about pelvic floor training for women and pelvic floor training for men.
Medicines for overactive bladder
If there's not enough improvement with bladder training alone, medicines in the class of drugs called antimuscarinics (also called anticholinergics) may also help. They include oxybutynin, tolterodine, trospium chloride, propiverine, and solifenacin. These also come in different brand names. They work by blocking certain nerve impulses to the bladder, which relaxes the bladder muscle and so increases your bladder capacity.
Medication improves symptoms in some cases, but not all. The amount of improvement varies from person to person. You may have fewer toilet trips, fewer urine leaks, and less urgency. However, it's uncommon for symptoms to go away completely with medication alone. A common plan is to try a course of medication for a month or so. If it is helpful, you may be advised to continue for up to six months or so and then stop the medication to see how symptoms are without the medication. Symptoms may return after you finish a course of medication. However, if you combine a course of medication with bladder training, the long-term outlook may be better and symptoms may be less likely to return when you stop the medication. So, it is best if the medication is used in combination with bladder training.
Side effects are quite common with these medicines but are often minor and tolerable. Read the information sheet, which comes with your medicine, for a full list of possible side effects. The most common is a dry mouth, and simply having frequent sips of water may counter this. Other common side effects include dry eyes, constipation and blurred vision. However, the medicines have differences, and you may find that if one medicine causes troublesome side effects, a switch to a different one may suit you better.
Surgery
If the above treatments are not successful, surgery is sometimes suggested to treat overactive bladder syndrome. Procedures that may be used include:
Sacral nerve stimulation
An overactive bladder can be treated by sacral nerve stimulation. A small pulse generator device is implanted under the skin of your buttock to send a burst of electrical signals to the nerves that control the bladder.
Augmentation cystoplasty
In this operation, a small piece of tissue from the intestine is added to the wall of the bladder to increase the size of the bladder. However, not all people can pass urine normally after this operation. You may need to insert a catheter (a small tube) into your bladder in order to empty it.
Urinary diversion
In this operation, the ureters (the tubes from the kidneys to the bladder) are routed directly to the outside of your body. There are various ways that this may be done. Urine doesn't flow into your bladder. This procedure is only done if all other options have failed to treat your overactive bladder syndrome.
Treatment with botulinum toxin A
This is an alternative treatment to surgery if other treatments including bladder training and medication haven't helped your symptoms. The treatment involves injecting botulinum toxin A into the sides of your bladder. This treatment has an effect of damping down the abnormal contractions of the bladder. However, it may also damp down the normal contractions so that your bladder isn't able to empty fully. If you have this procedure you usually need to insert a catheter (a small tube) into your bladder in order to empty it.
Note: Botulinum toxin A has now been licensed (approved) for the treatment of overactive bladder syndrome. Make sure that you discuss this procedure fully with your healthcare provider and understand all of its risks and benefits before you go ahead with it.
Continence adviser
Your healthcare provider may refer you to the local continence adviser. Continence advisers can give advice on treatments, especially about bladder training and pelvic floor exercises. If incontinence remains a problem, they can also give lots of advice on how to cope. For example, they may be able to supply various appliances and aids to help, such as incontinence pads, etc.
Getting to the toilet
Make this as easy as possible. If you have difficulty getting about, consider special adaptations like a handrail or a raised seat in your toilet. Sometimes a commode in the bedroom makes life much easier
Effects of caffeine and alcohol
Tea, coffee, cola, and some pain relieving tablets contain caffeine. Caffeine has a diuretic effect and will make more urine. Caffeine may also directly stimulate the bladder to make urgency symptoms worse. It may be worth trying without caffeine for a week or so to see if your symptoms improve. If so, you may not want to give up caffeine completely but you may wish to limit the times that you have a caffeine-containing drink. Also, you will know to be near to a toilet whenever you have caffeine.
For some people, alcohol may make symptoms worse. The same advice applies as with caffeine drinks.
Drink normal quantities of fluids
It may seem sensible to cut back on the amount that you drink so your bladder doesn't fill so quickly. However, this can make your symptoms worse as the urine becomes more concentrated, which may irritate the bladder muscle. Aim to drink normal quantities of fluids each day. This is usually about 2 litres of fluid per day – about 6 to 8 cups of fluid, and more in hot climates and hot weather.
Go to the toilet only when you need to
Some people get into the habit of going to the toilet more often than they need. They may go when their bladder only has a small amount of urine so as not to be 'caught short'. This again may sound sensible, as some people think that symptoms of an overactive bladder won't develop if their bladder doesn't fill very much and is emptied regularly. However, again, this can make symptoms worse in the long run. If you go to the toilet too often the bladder becomes used to holding less urine. The bladder may then become even more sensitive and overactive at times when it is stretched a little. So, you may find that when you need to hold on a bit longer (for example, if you go out), symptoms are worse than ever.
Apps reviewed by Healthify
You may find it useful to look at some pelvic floor exercise apps.
Good bladder and bowel health(external link) NZ Continence Association
Pelvic Floor First(external link) Australia
Apps
Credits: New Zealand Continence Association, adapted for Healthify. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed:





