Breathing pattern disorders
Also known as dysfunctional breathing, including over breathing or hyperventilation
Key points about breathing pattern disorders (BPDs)
- BPDs are ongoing abnormal patterns of breathing, a common one being over breathing (hyperventilation) when you breathe more and faster than is needed for your body to function normally.
- BPDs result in abnormal breathlessness or air hunger and can include other symptoms such as dizziness, chest tightness, cold hands, tingling or blurred vision.
- Underlying lung conditions such as asthma need to be ruled out before a diagnosis is made.
- BPDs can be associated with health conditions, also your emotions and pain.
- Breathing retraining can improve your symptoms.

Your respiration rate (breathing rate) is measured as the number of breaths you take in a minute. A typical adult takes 12 to 20 breaths each minute when they’re resting. Your breathing rate goes up when you exercise and should come back down to a resting rate afterwards. Read more about breathing rate.
Normal breathing is slow and regular – breathing in and out through your nose only. No effort should be visible, your diaphragm and belly should be moving gently.
The main breathing muscles include your diaphragm, a dome shaped muscle below your lungs and above the organs in your abdomen or belly, and also the muscles between your ribs. Other muscles involved, known as accessory muscles, include some of your neck and shoulder muscles (eg, scalene or sternocleidomastoid or serratus muscles).
If you're in good health, your accessory muscles are not active during regular breathing. However, you may use these muscles when you're breathing hard or deliberately taking a deep breath. Breathing out or exhaling is generally passive (without active muscle activity) and is caused by the natural elastic recoil (or deflation) of your lung tissue accompanied by the relaxation of all breathing muscles.
The following video shows how your respiratory system works when you’re breathing in (inhaling) and out (exhaling).
Video: How do lungs work? Emma Bryce
Sometimes a normal breathing pattern is disrupted, such as by health conditions, an emotional response or pain. However, the atypical breathing pattern can become a habit without there being a cause for it and then it can become a breathing pattern disorder (see below). Next to over-breathing or hyperventilation you may develop a pattern of frequent deep sighing and over-use your chest or neck muscles rather than using your diaphragm.
- Dyspnea or air hunger is a feeling of being short of breath or feeling like you can’t get enough air in. It may be due to a heart or a lung condition such as asthma. If you’re short of breath very suddenly get medical help.
- It may be normal to feel short of breath if you’re at a very high altitude where there’s less oxygen in the air.
- If breathlessness only occurs when your body is in a certain position and moving can relieve it, there should be less concern.
- Tachypnea is a word used to describe when you breathe faster than normal. It may be because your lungs can’t take in as much air as they should (eg, if you have pneumonia or a chronic lung condition) but it may be perfectly normal when exercising. It can also happen more quickly if you are very overweight.
- Hyperpnea is a word used to describe when you breathe in more air than usual but you’re not necessarily breathing faster. This may be normal when you’re exercising but may occur if you have a condition that makes it hard for your body to get oxygen, such as heart failure or a chronic lung condition.
Breathing pattern disorders (BPDs), also known as dysfunctional breathing, are ongoing or recurrent abnormal patterns of breathing. A common type is over breathing, called hyperventilation, which is breathing more often than is needed for your body to function normally. Disordered breathing can lead to a feeling or sensation of difficult breathing and other symptoms that aren’t fully explained by an already existing or underlying medical condition.
Over breathing
Over breathing (commonly known as hyperventilation) is when you breathe more, and more quickly, than you need to. This moves more air through your chest than is needed. Your lungs swap the oxygen in the air that you breathe in for the carbon dioxide that your body makes when 'burning' nutrients and creating energy for your body to function. If you over breathe (hyperventilate) you lose too much carbon dioxide. This causes changes in the chemistry of your blood and your body (respiratory alkalosis) and affects the balance of different blood minerals such as calcium or potassium. This then will result in changes to nerve cells and the blood flow to your heart and different organs including your hands, feet and brain due to a tightening of the muscles of blood vessels (vasoconstriction).
Over breathing is a common breathing problem and may happen when you’re in an exciting or stressful situation. However, when hyperventilation is chronic (ongoing) or keeps coming back often, and you experience symptoms such as a racing heart, tingling in your fingers, or breathlessness, or anxiety, it’s known as hyperventilation syndrome.
You might change the way you breathe, your breathing pattern, from normal abdominal (belly) breathing to upper chest breathing and also draw in the air through your mouth instead of your nose. This leads to changes in upper chest and neck muscles, which in turn causes pain, tension and headaches.
Natural anxiety over these symptoms leads to further over-breathing, creating a vicious cycle. This new breathing pattern becomes a major stress all by itself. You might not always notice that you’re over breathing. Instead you might notice lots of different symptoms, and you and your healthcare provider might wonder if you have a serious disease.
Other disordered breathing patterns
Hyperventilation syndrome is one type of BPD. Other types include:
- Simple upper chest or thoracic breathing where you breathe shallowly just using your chest muscles without engaging your diaphragm and tummy muscles.
- Periodic deep sighing which is when you take a long deep breath or a second breath in before you exhale (breathe out). It may also happen when you’re feeling emotional (eg, anxious or sad) or when you're in pain.
- Forced abdominal exhalation or expiration – inappropriate or excessive use of your belly muscles when breathing out. This should be a passive process not requiring any effort.
- Asynchrony or poor coordination between your rib cage and your belly or abdominal muscle contractions
Another condition that can cause breathlessness is inducible laryngeal obstruction or vocal cord dysfunction. It's when your larynx (throat) temporarily narrows also affecting the breathing passages above your lungs. It's usually accompanied by symptoms of throat irritation and air hunger. It can happen in response to environmental triggers (eg, temperature change, smells or sprays), physical triggers (eg, exercise, laughing or eating) or psychosocial triggers (eg, stress o anxiety).
Medical conditions should treated or ruled out before it's decided that you have a BPD..
A breathing pattern disorder may be the main problem but possible underlying causes related to BPDs include:
- depression, anxiety, prolonged stress
- ME/CFS or long COVID
- chronic pain
- chronic lung or respiratory conditions such as asthma.
Other causes of over-breathing include:
- fever
- being at high altitude
- abnormal hormone levels
- exercise.
Medicines such as salbutamol (Ventolin, Salair) inhalers, progesterone, excess alcohol, caffeine or nicotine will result in an increased breathing rate. So will medical conditions such as anaemia, asthma or COPD, blood clots in your lungs or weakness of your heart.
Symptoms differ from person to person. If you have a breathing pattern disorder you might experience:
- headache
- air hunger (the feeling of shortness of breath or not getting enough air)
- frequent sighing or yawning
- tight chest, chest pain
- upset tummy, nausea, frequent feelings of bloating or belching
- clammy or cold hands
- light-headedness or dizziness
- palpitations (a feeling of your heart racing or pounding)
- weakness
- tingling in your fingers and toes or around your mouth
- blurred vision.
You may also notice that:
- you breathe through your mouth rather than your nose
- your breathing is noisy
- your breathing is fast or shallow
- your upper chest moves outwards more than your tummy when you breathe in
- you find it hard to coordinate your breathing when you talk or eat
- you have muscle tension or aches and pains around your shoulder, neck and jaw
- you feel exhausted all the time and find in hard to concentrate.
During an acute hyperventilation episode you may also have ringing in your ears, a sense of impending doom or that something terrible is going to happen, sweating, or feelings of anxiety or panic.
Your healthcare provider will consider a diagnosis of a breathing pattern disorder if:
- you have breathing signs or symptoms that occur when you’re resting (not exercising)
- the symptoms come and go regularly, and
- underlying medical conditions (eg, asthma in particular, but also other lung, heart, blood or brain problems) have been ruled out or are being treated.
There’s no special medical test to diagnose breathing pattern disorders, but an abnormal result on the Nijmegen questionnaire may be an indication.
If your healthcare provider suspects you have a breathing pattern disorder, they can refer you to a respiratory physiotherapist and sometimes a speech language therapist who can assess your breathing and provide treatment.
Other things you can do if you have a breathing pattern disorder include the following.
- Try to recognise the situations that trigger over breathing. Calm your breathing down before these situations and focus on keeping a steady rhythm until the situation is over. Think about whether you can change or avoid these triggers.
- If certain situations or thoughts lead to feelings of panic which affect your breathing learn how to manage a panic attack.
- Notice if you’re tending to breathe through your mouth rather than your nose and work on changing this.
- If you have problems coordinating your breathing while you’re talking, try to slow down your speech – stop and take a breath after each sentence. A respiratory physiotherapist can help with this.
- Avoid drinks that contain stimulants such as caffeine as these can trigger over-breathing.
- Try to have regular balanced meals as changes in your blood glucose levels can make your symptoms worse. If you tend to snack, avoid foods high in sugar as they make your glucose levels rise and then fall rapidly, and this can act as a trigger that makes you over-breathe.
- Maintain a good posture. Sit and stand up straight so your diaphragm can move freely. Think about getting an ergonomics assessment of your workplace to make sure it’s not adding to physical health or breathing problems.
- If your sleep is disturbed because of your breathing, breathing re-training should help and you can also read these sleep tips.
- Practice relaxation techniques, such as mindfulness or yoga, and do things you enjoy such as hobbies, exercise or having a massage. Taking time to relax can help you gain control of your breathing.
The following video can help you understand and manage a breathing pattern disorder.
Video: Breathing pattern disorders
Apps reviewed by Healthify
You may find it useful to look at some breathing apps, sleep and snoring apps, meditation and mindfulness apps and anxiety management apps.
It’s important to consider things that may trigger your breathing pattern disorder (BPD) and address these in order to help your recovery. Be reassured that your symptoms are treatable.
Remember that normal breathing involves your diaphragm, which is a dome-shaped muscle under your ribcage, rather than just filling your chest with air.
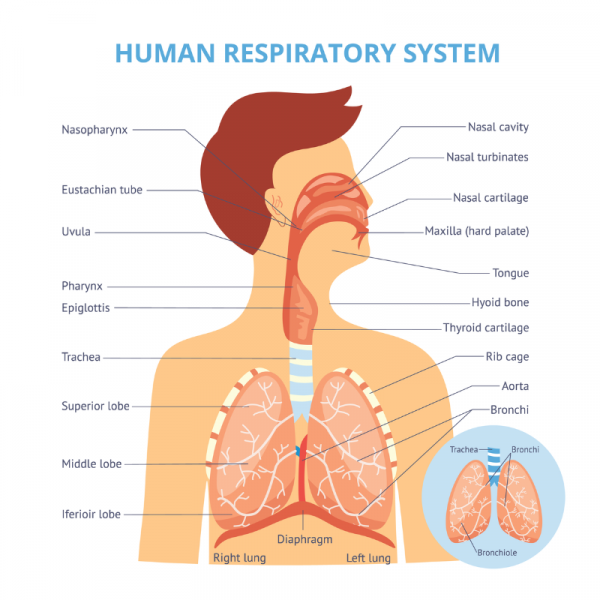
Image credit: Depositphotos
A respiratory physiotherapist can help you with breathing retraining where you learn to recognise and change unhelpful breathing habits. If you're troubled by mainly throat-related breathlessness and other related symptoms, a review by a speech language therapist will be helpful.
During an acute hyperventilation episode
It’s important to understand that the feeling of not being able to breathe isn’t a sign that you will truly stop breathing or that there’s something seriously wrong.
If there's a trigger, or something causing you stress, remove it if possible.
Some people find a breathing exercise helps during an episode. Here's one example:
- While lying or sitting, put one hand on your tummy, the other on your chest.
- Notice which one moves the most. If you’re hyperventilating or have disordered breathing, this will almost always be the hand on your chest.
- Change your breathing so that the hand on your tummy moves more and the hand on the chest hardly moves at all. It takes practice to get the hang of this.
- Breathe in slowly over 4 seconds, pause for a few seconds, and then breathe out over a period of 8 seconds.
- After 5 to 10 breathing cycles, you should start to feel calmer and notice your breathing improves.
You can find a breathing exercise video on our anxiety page.
You might have seen advice to breathe into a brown paper bag if you’re hyperventilating – to normalise the low level of carbon dioxide in your blood. It's best NOT to do this as it's not considered to be safe for all causes of hyperventilation.
After an episode or if you have hyperventilation syndrome or another BPD
Look for ways to reduce stress. If you have anxiety, this should be addressed. Seeing a psychologist may be helpful.
A respiratory physiotherapist can teach breathing pattern retraining and specific ways to relax. You can ask your healthcare provider about a referral, but note that you often have to pay for this yourself. It should be a worthwhile investment.
A structured treatment plan often includes:
- ruling out or addressing underlying health conditions such as asthma
- an upper respiratory health assessment
- postural and upper chest musculoskeletal balancing
- breathing retraining
- breathing through your nose
- stress recognition
- physical coping strategies
- advice on sleep hygiene
- a graduated fitness regimen/lifestyle assessment.
It can take 6 to 8 weeks or longer to change your breathing back to a normal pattern. You'll need to work hard at practicing your breathing.
As you learn to breathe well and restore balanced carbon dioxide and oxygen levels, the unpleasant symptoms which come with over breathing will ease.
Breathing pattern disorders and physiotherapy(external link) Cambridge University Hospital, NHS Foundation Trust, UK, 2024
Brochures
Your guide to over-breathing (also known as hyperventilation)(external link) Physiotherapy for Breathing Pattern Disorders, UK
Breathing pattern disorders – information for patients(external link) University Hospital Southampton, NHS Foundation Trust, UK, 2023
Apps
Breathing apps
Sleep and snoring apps
Anxiety management apps
Meditation and mindfulness apps
References
- Breathing pattern disorders – an overview(external link) Cambridge University Hospital, NHS Foundation Trust, UK, 2023
- Types of breathing problems explained(external link) WebMD, US, 2022
- Hyperventilation(external link) Cambridge University Hospital, NHS Foundation Trust, UK, 2020
- Breathing pattern disorders(external link) Physiopedia, UK
- Why do we sigh and what does it mean?(external link) Cleveland Clinic, US, 2023
- Dysfunctional breathing disorders(external link) Goodfellow Unit, NZ, 2021
- Hyperventilation syndrome / breathing pattern disorders(external link) Family Doctor, NZ, 2015
- Hyperventilation – causes, symptoms and treatment(external link) Patient Info, Doctor, UK, 2021
- Boulding R, Stacey R, Niven R, et al. Dysfunctional breathing – a review of the literature and proposal for classification(external link) ERR 2016;25(141): 287–294
- BTS clinical statement for the assessment and management of respiratory problems in athletic individuals(external link) British Thoracic Society, UK, 2022
- Ludlow S, Daly R, Elsey L, et al. Multidisciplinary management of inducible laryngeal obstruction and breathing pattern disorder(external link) Breathe (Sheff) 2023;19(3):230088
Podcast
Dysfunctional breathing disorders(external link) Goodfellow Unit Podcast, NZ, 2021 Dr Stephen Child discusses assessment, investigation and management of dysfunctional breathing disorders (22 minutes)
Webinar
Understanding breathing pattern disorders(external link) Goodfellow Unit Webinar, NZ, 2023 Scott Pierce (MHSC Physio) (1 hour 9 minutes)
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Roland Meyer, Specialist Physician, Respiratory and General Medicine
Last reviewed:





