You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Breathlessness
Also known as shortness of breath or dyspnoea
Key points about breathlessness
- Breathlessness is the uncomfortable sensation of having difficulty breathing and feeling short of breath.
- Anyone can feel puffed and out of breath when exercising, but if you get breathless while you’re resting, see your healthcare provider as you may have an underlying health condition.
- There are many causes of breathlessness. Some aren’t serious, but some are.
- Treatment will depend on what’s causing your breathlessness.
- Ways of managing breathlessness include medicine, breathing techniques, changes in position and relaxation exercises.

Breathlessness is the uncomfortable sensation of having difficulty breathing and feeling short of breath. The medical term for breathlessness is dyspnoea. It can be acute, which is when it comes on suddenly (over minutes, hours or days), or chronic, when you’ve had it for a long time.
It’s normal to feel breathless when you do heavy physical activity such as running. However, if you get breathless when resting or doing only gentle activity (such as walking around the house), or if your breathlessness comes on suddenly, it’s important to see your healthcare provider as it could be due to a serious underlying health condition.
You feel breathless when your brain detects that your body isn’t breathing well enough to meet its needs, such as if the oxygen levels in your blood are too low.
Common or important causes of breathlessness include COPD, cancer (or complications of cancer or its treatment), heart failure, obesity and anxiety.
Breathlessness may be acute, when it comes on suddenly over a short time, or it may be chronic, when it can develop slowly and is ongoing.
Some acute causes of breathlessness
- Asthma – wheeze and breathlessness are caused by triggers, which can include allergy, exercise or infections such as a cold.
- A flare-up of COPD.
- Pneumonia – a severe chest infection.
- Pneumothorax – a collapsed lung.
- Pulmonary embolism – a blood clot in your lung.
- Pulmonary oedema – fluid inside your lungs.
- Heart attack or flare-up of heart failure.
- Anxiety can cause breathlessness, along with a rapid heartbeat (palpitations), sweating and feelings of panic.
- Some medicines, such as beta-blockers and aspirin, can trigger asthma symptoms or make them worse.
Some chronic causes of breathlessness
- COPD.
- Asthma that's not well controlled.
- Other lung conditions such as bronchiectasis or lung cancer.
- Heart failure.
- Heart rhythm problems, such as atrial fibrillation – this means blood isn’t pumped around your body properly so your breathing becomes more rapid to try and get more oxygen into your lungs.
- Anaemia – the low iron levels in your blood means there’s not enough haemoglobin in your blood to transport enough oxygen around your body.
- Being obese or not very fit.
- Some cancers, complications of cancer or treatment for cancer.
Video: What being breathless could mean
(Patient Info, UK, 2018)
The experience of breathlessness can range from mild shortness of breath to very fast gasping breaths. You may also feel:
- dizzy
- chest discomfort and/or tightness
- anxious or scared.
You may feel like you can’t get enough air when you breathe in or you’re having to work hard to take a breath.
Seek immediate medical attention from the nearest emergency department or call 111 if you or someone you care for has the following symptoms:
- Sudden breathlessness that develops over hours or days.
- Shortness of breath at rest.
- Severe breathlessness stopping you from being able to speak in full sentences.
- Confusion or drowsiness.
- Chest tightness or sudden chest pain at rest.
If you have a lung condition that makes you breathless from time to time, such as asthma or COPD, use your reliever inhaler immediately and follow the action plan written by your doctor or nurse. Read more about asthma and COPD.
If your breathlessness has come on slowly and has been happening for more than a month, it’s a good idea to see your healthcare provider and get checked to make sure it’s nothing serious.
If you have infectious symptoms (eg, cough, fever, sore throat) ask your medical clinic about how you can get an appointment without putting other people at risk of infection.
To diagnose the underlying cause of your breathlessness, your healthcare provider may ask:
- how often it happens, how quickly it comes on and how long it lasts
- if anything in particular causes you to become breathless or makes it worse
- if anything relieves your breathlessness, or makes it feel better
- if it happens at rest or with activity
- if you can sleep flat at night or if it gets worse lying down
- if you wake up overnight feeling suddenly breathless
- if you’ve been unwell with a fever
- if you’ve been coughing any mucus or have any discomfort in your chest
- if you’ve been having issues with high stress, anxiety or low mood.
If you’re known to have a condition that causes breathlessness, your healthcare provider will review your medicines and/or inhalers. They may ask you how you’ve been using them and may explain how to use them to make sure they’re working well.
Your healthcare provider may also listen to your heart and lungs, look at your lower legs or feel your tummy. If the cause of your breathlessness isn’t obvious from your history and examination, you may need further tests. These include:
- blood tests, eg, to look for causes such as heart failure or low iron
- a chest X-ray
- spirometry
- ECG or electrocardiogram.
You may be referred to a heart specialist (a cardiologist) or a lung (respiratory) specialist, depending on the most likely underlying cause of your breathlessness.
Treatment will depend on what’s causing your breathlessness. You may be given medicines, such as:
- antibiotics to treat pneumonia or another chest infection
- diuretics for conditions such as heart failure
- inhalers or nebulisers if you have asthma or COPD
- medicine for anxiety
- chemotherapy or other treatment for lung cancer.
If you have a serious life-threatening cause for your breathlessness, such as a heart attack, worsening heart failure, sudden worsening of asthma or COPD, or severe pneumonia, this will be treated urgently.
If you’re a smoker, you’ll be strongly encouraged to stop. Losing weight if you’re overweight will also help. See the self-care section below for other things you can do to help ease your breathlessness.
If your healthcare provider thinks that you might have low oxygen levels, they may consider whether home oxygen therapy is suitable for you. You’ll have a blood test to check your blood oxygen levels. Oxygen therapy can provide relief from breathlessness, but it will only help if you're low in oxygen.
If you have a breathing pattern disorder that’s contributing to your breathlessness this will also be investigated and managed.
You can also read about treatment of breathlessness in palliative care.
There are a number of things that can help if you’re living with ongoing (chronic) breathlessness.
- If you’re a smoker, get help to stop smoking.
- Try to lose weight if you’re overweight.
- Keep as active as possible. If you’re able, you could try activities such swimming, yoga, pilates, or tai-chi, walks and exercise classes in your community.
- Make changes to make daily activities easier eg, plan your day so you have plenty of time to rest, break activities into smaller tasks, put frequently used items in easy-to-reach places.
- Use a wheeled walking frame with a seat if you need a walking aid.
- Learn breathing exercises to help you relax and control your breathing (see the video below for an example). Ask your healthcare provider about getting a referral to a physiotherapist to learn about breathing techniques and exercises. You can also look for a physiotherapist who specialises in respiratory conditions. Find a physio(external link).
- Cardiac and respiratory rehabilitation classes can help you learn how to manage your breathlessness if you have a relevant condition – ask in clinic or your healthcare provider if you qualify.
- Find a comfortable body position that supports you when you’re breathless.
- Use a hand held fan or a standing or desk fan to blow air towards you as this can reduce feelings of breathlessness. Sitting near an open door or window may also help.
- Practice relaxation or mindfulness exercises – these can help you feel calmer and slow your breathing, especially if your breathlessness makes you feel anxious. Read more about mindfulness.
- Have a plan for when you get very breathless:
- Try to keep calm.
- Use positive, reassuring self-talk (eg, “This will pass, slow down ... stay calm ... I can slow my breathing.”).
- Find a comfortable position.
- Don’t talk.
- Sit near an open window or use a fan.
- Use your relaxation and breathing techniques to slow your breathing.
- Find a distraction (such as listening to music or watching TV).
- Take your breathlessness medicine.
- Call 111 if you have severe sudden breathlessness with no obvious cause.
- Find ways to manage anxiety.
- Ask for support or help if you need it.
See the more information below for resources to help when you’re breathless.
Video: Positions to relieve breathlessness
(Cancer Society of New Zealand, 2021)
Video: Guided square breathing exercise in 2 minutes
Apps reviewed by Healthify
You may find it useful to look at some anxiety management apps, breathing apps, meditation and mindfulness apps, COPD apps, heart failure apps and nutrition, exercise and weight management apps.
Breathlessness can’t always be prevented but some things might help.
- If you smoke, get help to stop. All common serious causes of breathlessness are more likely to affect you if you’re a smoker.
- If you’re overweight, try to lose weight. If you can maintain a healthy weight and do regular exercise, you’re less likely to get breathless.
- Exercise regularly. Even if you have a lung condition, exercise and pulmonary rehabilitation can help. It strengthens your muscles and helps you manage your daily activities. Being fit also improves your heart and lung function, which helps to provide your body with the oxygen it needs. If you’re struggling to exercise due to breathlessness, talk to your doctor as there may be an exercise/rehabilitation programme you can be referred to (depending on your health condition). Read about pulmonary rehabilitation and green prescriptions.
- If you’re on medication for your breathing, make sure you take it as prescribed. If you’re still getting symptoms, see your healthcare provider or pharmacist for a medication review.
- Practice mindfulness and relaxation techniques.
Living with breathlessness can be frightening. It’s also challenging to do things physically. Talk through your feelings with your whānau and friends to get the support you need.
There are asthma and COPD societies(external link) around the country that offer support groups for people with respiratory conditions and their family/whānau.
The Cancer Society Cancer helpline(external link) on 0800 226 237 puts you in touch with a cancer support nurse and there also support groups throughout the country.
Heart Foundation NZ has a list of heart support groups(external link) for people living with a heart condition.
The following links provide further information on breathlessness. Be aware that websites from other countries may contain information that differs from New Zealand recommendations or emergency contact details. In New Zealand, call 111 or go to your hospital emergency department if it’s an emergency.
Shortness of breath(external link) NHS, UK
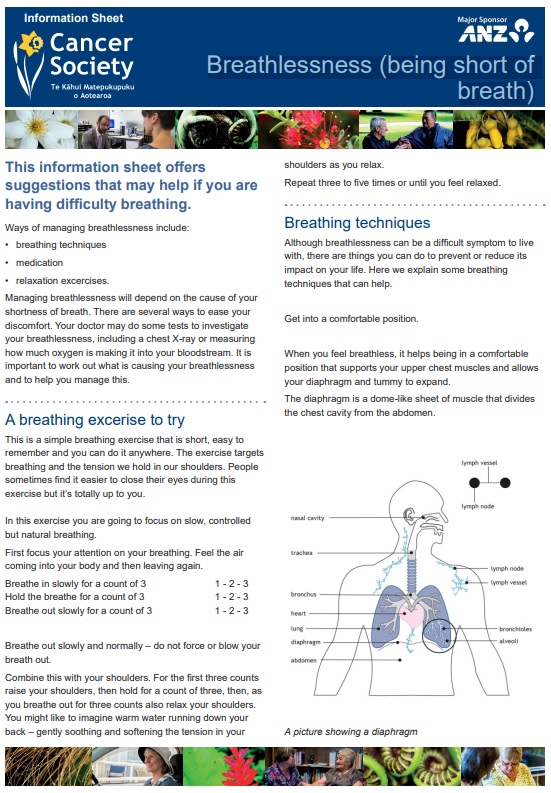
Breathlessness(external link) Cancer Society, NZ
Supporting someone with breathlessness(external link) Supporting Breathlessness, UK
Living well with breathlessness(external link) Asthma and Lung UK, 2024
Ten tips for managing breathlessness(external link) Cambridge University Hospitals, NHS, UK, 2023
Apps
Anxiety management apps
Breathing apps
COPD apps
Heart failure apps
Meditation and mindfulness apps
Nutrition, exercise and weight management apps
Brochures
Breathlessness – shortness of breath(external link) American Thoracic Society, US, 2020
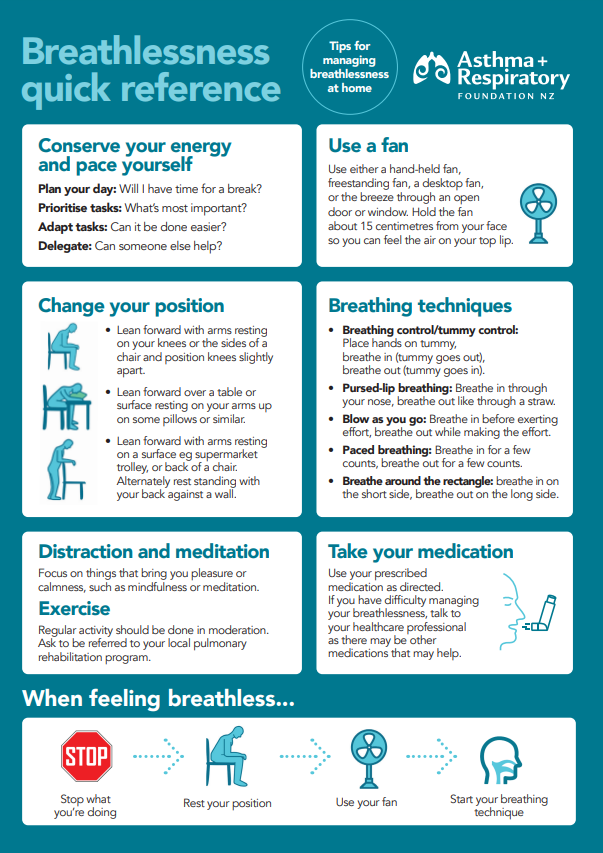
Breathlessness – strategies for COPD(external link) Asthma and Respiratory Foundation, NZ
Breathlessness – being short of breath(external link) Cancer Society NZ, 2016
Breathlessness and how to manage it(external link) West Suffolk NHS Foundation Trust, UK, 2025
Breathlessness quick reference(external link) Asthma and Respiratory Foundation, NZ
References
- Dyspnoea(external link) Auckland Regional Health Pathways, NZ, 2024
- Breathlessness(external link) Patient Info, UK, updated 2024
- Shortness of breath(external link) NHS, UK, 2024
- Supporting someone with breathlessness(external link) Supporting Breathlessness, UK
Adult breathlessness pathway (pre-diagnosis): diagnostic pathway support tool(external link) NHS, UK, 2023
Video consultations: Clinical modules – respiratory assessment(external link) ProCare, NZ, 2021
Managing breathlessness in palliative care(external link) BPAC, NZ
Breathlessness(external link) Patient Info Doctor, UK, 2025
Breathlessness in palliative care(external link) Marie Curie, UK, 2021
Supporting someone with breathlessness(external link) Supporting Breathlessness, UK
It can be difficult to think and talk about the future, but doing this helps you and your carer for being better prepared.
Talking about the future
Talking about the future helps be better prepared for the future. However, having these conversations is not always easy.
It is also useful to talk about having an advanced directive or advance care plan, which can help you decide what to do if you become unwell. Read more about talking about the future with others(external link).
For carers: common changes if the person you care for get sicker
As the condition of the person you care for progresses, you may notice changes in their symptoms and that they can be more difficult to manage. They may also need more support as the condition worsens.
Some of the common changes that you may notice include:
- more breathlessness
- loss of appetite and weight loss
- pain
- tiredness
- difficulty sleeping
- having frequent infections
- more flare-ups, wheezing, chest tightness, phlegm in COPD.
If you are unsure or having difficulties managing any symptoms of someone you care for, talk to their healthcare provider. Sometimes, it may be recommended that they have a respite stay.
For carers: ways to cope with these changes
It may be hard for you to see how things change and how someone you care for gets sicker on a daily basis. It is also common that you as a carer feel drained and upset about what has happened. At times like these, you need to look after your physical and mental wellbeing as the person you care for will require more support from you.
Similarly, the person you care for will also struggle with difficult emotions and slowly withdraw from their daily life as the condition progresses. You can encourage them to talk through their feelings with you, other family members and friends, a trained counsellor or one of the healthcare team members. You can ask their healthcare provider for a referral to a trained professional.
Accessing care and support
Knowing where and how to access care and support is important.
It is common to have more than one healthcare professional taking care a person with breathlessness. Depending on the condition, some of the healthcare team members involved can include:
- a specialist doctor, eg, a respiratory specialist if the condition is COPD or a cancer specialist (oncologist) if it is cancer
- radiologist – a doctor who diagnoses diseases by using imaging such as x-ray, ultrasound scan or CT scan
- specialist nurse, practice nurses or district nurses
- surgeon – a doctor who performs surgery in the operating theatre
- GP
- physiotherapist
- occupational therapist
- psychologist
- palliative care team – the team consists of doctors, nurses, and other allied health professionals to help manage symptoms nearing the end of life that aims to keep patients as comfortable as possible.
For carers: talking to the healthcare team
Sometimes, it may feel challenging to talk to the healthcare team about the person you care for because:
- the needs of the person you care for have not been heard by the healthcare team
- you and the person you care for don't understand what the healthcare team is saying
- you and the person you care for don't want to ask too many questions
- you feel left out about your patient's care (you need to understand that there are things the healthcare team can't talk to you about regarding the person you care for without their permission).
However, to make sure they get the best possible care, you need to understand what the healthcare team is saying and you need to express your concerns and the needs of the person you are caring for.
Here are some tips to help you talk to the healthcare team:
- Prepare a list of questions you or the person you care for may have and bring to their appointment.
- Ask questions – you need to understand what is happening and how you can help.
- Ask questions which are most important first.
- You may need to ask a question more than once to make sure you understand fully.
- You can keep a note or record the conversation during the appointment.
- If the person you care for is receiving palliative care, let all the healthcare professionals involved in their care know so everyone is aware of the type of support they need.
Read more about talking to the healthcare team(external link).
For carers: when someone dies
It can be a difficult time for you when the person you care for dies. You may find it hard to cope with and may experience grief and bereavement.
Common emotions or feelings you may notice include:
- loneliness
- guilt
- shock or numbness
- anger
- fear
- longing
- sadness.
Some of the bodily changes you may also notice include:
- being tearful
- difficulty sleeping
- weight loss or weight gain
- loss of appetite or increased appetite
- tiredness
- lack of energy
- headaches.
These feelings and bodily changes can come on early or later when all the practical matters such as organising a funeral have been done.
You may find it helpful to talk things through to help you manage grief and bereavement. You can talk to your family/whānau, friends or relatives, people in a support group, or a trained professional such as a counsellor.
There are many organisations in New Zealand that provide support, advice and counselling to help those affected by loss and grief, including:
National grief support groups Healthify, NZ
The Grief Centre(external link) The Auckland-based centre provides counselling, support groups and training in the Auckland region, and also has information and resources available on their website
Skylight NZ(external link) Offers grief counselling in some centres and also has information and resources available on their website.
Hospice NZ(external link) ph 04 381 0266
Helplines and local mental health services(external link) Mental Health Foundation, NZ
Talk to your doctor if you have difficulty coping with daily life and you are having these grief feelings longer than expected. Read more about when someone dies(external link) and about grief and loss.
Brochures
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Sara Jayne Pietersen, FRNZCGP, Auckland
Last reviewed: