Care planning and care plans
Key points about care planning and care plans
- A care plan is useful if you have an ongoing health condition or have several people involved in your care.
- It’s designed to help you manage your conditions as well as possible, prevent complications, and achieve your health-related goals with the support of your healthcare team and whānau.
- Care planning is what happens when you (and whānau if you wish) talk to your healthcare team about what you want to achieve and how to achieve it.
- A care plan is the written document outlining what's been decided.

A big component of care planning may be self-management, as lifestyle changes such as healthy eating, exercise, and taking your medicines correctly are usually needed.
A care plan is the document that comes from care planning. It's a living document. This means it can, and should, be updated and changed based on discussions with your healthcare team about how to improve the way your look after your health conditions and your overall hauora and wellbeing. It should include what is important to you.
As social circumstances and life events affect your health and wellbeing, the Te Whare Tapa Wha model is often used in Aotearoa New Zealand for healthcare providers to understand your unique situation. The 4 parts of wellbeing are Taha tinana (physical health), Taha wairua (spiritual health), Taha whānau (family health) and Taha hinengaro (mental health). They are all grounded in whenua or the land. Having information about all these aspects of your health/hauora enables a personalised or individualised care plan to be made by you, your healthcare team and your whānau. Read more about Māori models of health and Pasifika models of health.
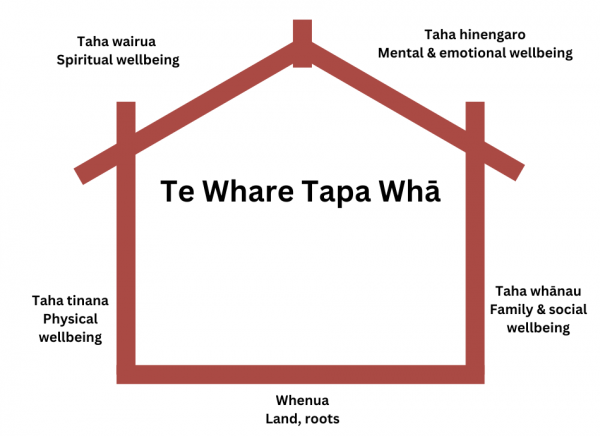
Image credit: Health Navigator NZ
Personalised care planning is a series of conversations, including decision-making and review, between you and any healthcare providers and whānau members you want to be included. You should be involved as an active and equal participant in the conversations.
It takes into account your:
- Life context including challenges such as:
- roles, eg, in your whānau, job and community
- housing
- finances.
- Age, as you may be facing extra challenges as you get older.
- Medical history, including the management of your health condition/s and prevention of complications, self-management skills, knowledge and confidence.
- Health status and what daily activities you can and can’t do.
- Values, beliefs and cultural needs, including the steps you want to take towards hauora along with your whānau.
- Abilities and strengths.
- Choices, goals and lifestyle wishes.
Ask your health care team for information and guidance so you can set your own goals and make your own decisions.
Before attending the first care planning discussion
Think about the following:
- Are you satisfied with your current state of health and wellbeing?
- What do you need?
- What would you like to change or do differently?
- How do you currently look after yourself and your health conditions?
- Are you doing this well?
- Are you getting feedback from your healthcare team that they would like you to do more to help yourself (self-management)?
- Could you put some of their suggestions into your daily routine?
- Would you be willing to work on lifestyle changes, eg, eating a healthier diet, exercising more or practising mindfulness to improve your mental wellbeing?
- Would you be willing to attend a group education or self-management group to increase your knowledge, skills or confidence?
- Potential barriers to making a positive change – how might they be overcome?
- Have there been times when you have successfully made a change in your life, eg, giving up smoking, or losing weight?
- How did you manage it?
Decide if you want to bring a whānau member or friend to your care planning appointment with you for support. It can be useful to have a ‘second pair of ears’ to help you deal with the amount and type of information information involved in discussions with healthcare providers. Let your healthcare team know they'll be coming along.
Check out Te Kete Haerenga our self-management toolkit designed to help you describe what's important to you and your whānau. It includes what you want to achieve in your life and how others can support you on your journey.
Diaries and other tools have been designed to help keep you on track. Just recently we have produced a number of self-management workbooks to help you manage issues such as sleep, pain, medicines, stress and fatigue. These issues can have a really big impact on your wellbeing and often one symptom affects another. For example if you have ongoing pain, and you're not sleeping well, your pain can seem overwhelming and that increases your anxiety or makes you feel down. Working on managing these symptoms is a really good option you could consider when you're setting goals.
Knowing how to set goals is an important part of care planning and it pays to take some time to think about what matters to you and how you might work towards achieving it. People at the Mayo Clinic in the US have come up with an acronym to help with setting SMART goals. The letters in SMART stand for:
- Specific: Eating healthier sounds like a good idea. But what does it really mean? Aim for specific goals instead, such as not having any fizzy drink for the week, filling ½ your plate with vegetables, eating 5 servings of fruit (limited to 2) and vegetables a day, or swapping out sugar for sugar-free options in your coffee/tea or on your breakfast cereal.
- Measurable: Make your goal one you can measure. Walking for 20 minutes 3 days a week is a goal you can track; a goal of ‘walking more’ is less easy to keep track of. Read more about the benefits of walking.
- Attainable: Avoid aiming too high or too low. Think like Goldilocks, and find a goal that feels just right.
- Realistic: Losing a couple of kilos a week sounds great. But it’s an impossible goal that will likely leave you discouraged – and more likely to give up on your efforts. Choosing realistic goals(external link) that you can meet will reinforce your efforts and keep you moving forward. In this case losing half a kilo a week is more likely.
- Trackable/Time-bound: Choosing specific, measurable goals means you can track your progress over time. Write your efforts down in a journal or track them on an app so you can see how far you’ve come. Time-bound means that you set a goal that's achievable within a set time frame, eg, within 3 months or within a year.
Sometimes people set too many goals, which can result in not achieving any of them. Start small and increase the number of goals over time, as you become ready for another one. Achieving the first one, however small, will build your confidence.
Another thing to avoid is setting goals you think your healthcare provider wants you to. It's really important for you to set goals that are meaningful for you as you will be more motivated to achieve them if you are looking forward to getting there.
- A care plan is the actual document that emerges from the care planning process. It should outline the things discussed including the goals or things you want to achieve. These things may not be the same as those your healthcare providers or whānau members want you to achieve. Your goals should be carefully discussed and described so that everyone involved knows exactly what you are aiming for, what you (and others) will do to enable you to achieve it, and how you will know when you have achieved it.
- It should be reviewed regularly and updated to include new goals or conditions.
- A written, or electronic, care plan should be produced to summarise the details and outcomes of the discussion. Ask for a copy to keep and refer to at home.
- Your care plan can include an emergency or acute plan (also known as an an action plan or sick day plan, eg, for people with diabetes). This provides written information about what to do if you get symptoms, if something goes wrong or if you get sick with other illnesses that may have an impact on your ongoing health conditions.
- Your care plan can also include advance care planning. This is a special type of care plan for what you want to happen if your condition becomes life-threatening and what you want to happen at the end of your life. It involves thinking, talking, planning, sharing and reviewing what matters to you so you can prepare yourself, your whānau and healthcare team for the future. Read more about advance care planning.
Note: If you live in the South Island of Aotearoa New Zealand, you can develop an acute plan or a personalised care plan with your healthcare provider which can then be stored electronically on the Health Connect South (HCS) site. HCS is a shared platform meaning that primary, secondary and community care providers can access your plan in order to best support your goals, co-ordinate your care and get valuable information if you need emergency services. Read more about these 2 shared care plans – acute plan(external link) and personalised care plan(external link).
Te Kete Haerenga – Your Journey to Wellbeing Kete Healthify He Puna Waiora, NZ
References
- Setting SMART goals for success(external link) Mayo Clinic, US, 2022
- Francis H, Carryer J, Wilkinson J. Patient expertise – contested territory in the realm of long-term condition care(external link) Chronic Illness 2018;15(3):197-209
- Taylor M, Budge C, Hansen C, et al. F. (2019). Written care plans and support for health goals – important components of long-term conditions care(external link) Kai Tiaki Nursing Research 2019;10(1):29-38
- A practical guide to self-management support(external link) The Health Foundation, UK, 2015
- Burt J, Rick J, Blakeman T, et al. Prevalence and benefits of care plans and care planning for people with long-term conditions in England(external link) Prim Health Care Res Dev. 2014;15(4), 342-354.
See our page Self-management support for healthcare providers
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Melanie Taylor, Nurse Advisor Long Term Conditions, THINK Hauora, Manawatu
Last reviewed:
Page last updated:





