Morphine is used for the relief of moderate to severe pain such as:
- after an injury or operation
- pain caused by a terminal illness such as cancer.
It's usually used when milder pain medicines such as paracetamol or non-steroidal anti-inflammatories (NSAIDs), don’t work well enough.
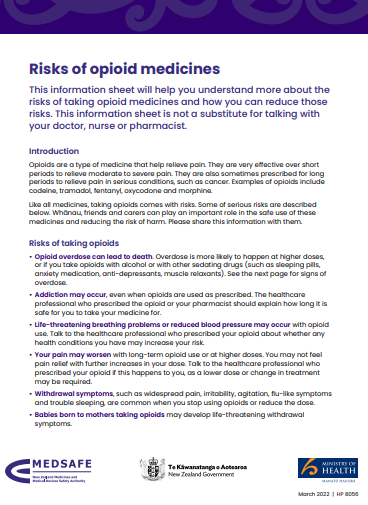
- Morphine belongs to a group of medicines called opioids. They act on your brain and nervous system to reduce pain.
- Other types of pain relievers such as paracetamol and NSAIDs (ibuprofen, diclofenac, naproxen) may also be used with morphine.
- Read more about pain, pain-relief medication, and opioids.
Morphine is also used to treat breathlessness and cough in palliative care. A regular small dose may help to ease symptoms of shortness of breath. Learn more about breathlessness in palliative care and cough in palliative care.
Morphine is also called:
- Sevredol tablets
- m-Eslon SR capsules
- RA-Morph liquid
- Wockhardt morphine liquid
- Oramorph.
Some types of morphine are short-acting or immediate release (eg, Sevredol tablets and morphine liquid) – they work quickly to ease your symptoms. Long-acting or slow release morphine (eg, m-Eslon SR capsules) works slowly over several hours to give a constant and more even pain control.
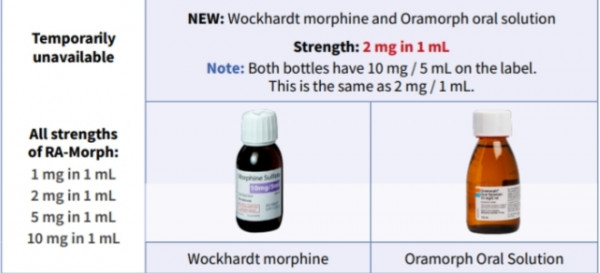
From March 2024, ALL strengths of RA-Morph morphine liquid will be temporarily unavailable, eg, 1 mg, 2 mg, 5 mg and 10 mg in 1 mL
|