Pain can start suddenly and last for a short time (called acute pain), or it can be ongoing and persistent, lasting months or years (called chronic pain).
Video: Acute vs Chronic pain
Video on understanding acute versus chronic pain developed by Healthify He Puna Waiora with support from PHARMAC. This video may take a few moments to load.
(Healthify He Puna Wairoa, NZ, 2018)
Acute pain
Acute pain usually comes on suddenly and is caused by something specific such as burns or cuts, bee stings, infection, broken bones, surgery, dental work and childbirth.
- The pain occurs for a short period of time (usually less than 3 months) and goes away when there is no longer an underlying cause.
- Acute pain can range from mild to severe and is important for survival as it warns us of actual or potential harm to our body.
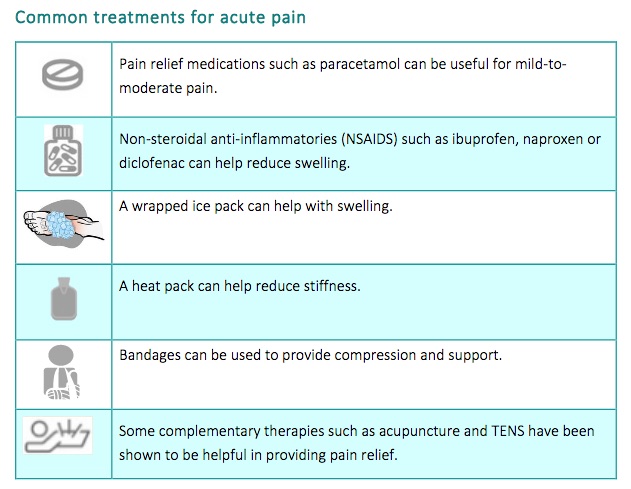
- Treatment: the sort of treatment that you will need will depend on the cause of your pain. For example, treatments for sprains and strains include pain relief medication, R.I.C.E (Rest, Ice, Compression, Elevation) or a support such as a brace or a cast. Find out more at where is my pain.
Chronic pain
Chronic pain is pain that lasts longer than 3 months. It is also called persistent pain or long-term pain. It is often described as pain that does not go away as expected after an illness or injury.
- Examples of causes of chronic pain include fibromyalgia, lower back pain and arthritis pain.
- About 1 in 6 New Zealanders live with chronic pain and no two people are affected in the same way.
- Chronic pain can range from mild to severe and can continue day after day or come and go.
- It can be distressing and can impact on your emotional and physical wellbeing.
- Although it can never be completely cured, it can be managed in ways that improve your quality of life and wellbeing.
- Treatment: medicines alone are not an effective way to manage chronic pain because of the harmful side effects of using them on an ongoing basis. Rather, non-medication treatments and strategies for helping you cope with your pain and come to terms with it are more effective. Read more about chronic pain.