If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Medicines for type 2 diabetes
Also called anti-diabetic medicines
Key points about medicines for type 2 diabetes
- Diabetes medicines help reduce your blood glucose levels. Eating well and staying active can make your treatment work even better and improve your overall health.
- Constantly raised blood glucose levels damage your blood vessels and nerves, leading to problems affecting your kidneys, feet and eyes, and your risk of stroke and heart attacks also increases significantly.
- Find out more about medicines for type 2 diabetes.

When you have type 2 diabetes (mate huka), your body does not make enough insulin or does not use it well enough. This leads to raised blood glucose levels. Having constantly raised blood glucose levels damages your blood vessels and nerves, leading to problems affecting your kidneys, feet and eyes and your risk of stroke and heart attacks also increases significantly.
Diabetes medicines can effectively lower your blood glucose levels, especially when used with a healthy diet and exercise.
Every person’s diabetes care plan is different. Your healthcare provider will work with you to find out the best treatment plan for you.
- Diabetes medicines are used to lower blood glucose levels in combination with exercise and weight management. Most people with type 2 diabetes will need diabetes medicines to control their blood glucose.
- There are a variety of medicines to treat type 2 diabetes. Most are available as tablets, but some come as injections.
- Usually tablets are started first, but insulin may also be started straight away if your blood glucose levels are very high.
- Your diabetes may be well controlled on one medicine, or you may need a combination of medicines. It can take a few adjustments to find the right dose that keeps your blood glucose in range.
- For the best results, continue to eat a healthy, balanced diet, stay active, and manage your weight while taking diabetes medicines.
Diabetes medicines available as tablets
Most people with type 2 diabetes are started on metformin tablets. Other diabetes medicines are usually prescribed if you're unable to take metformin or if your blood glucose levels have not been lowered successfully with metformin alone. Combining medicines can be a more effective way to lower your blood glucose levels. Click on the links below to find out more about each medicine.
- Metformin.
- Vildagliptin (Galvus®).
- Vildagliptin + metformin (Galvumet®).
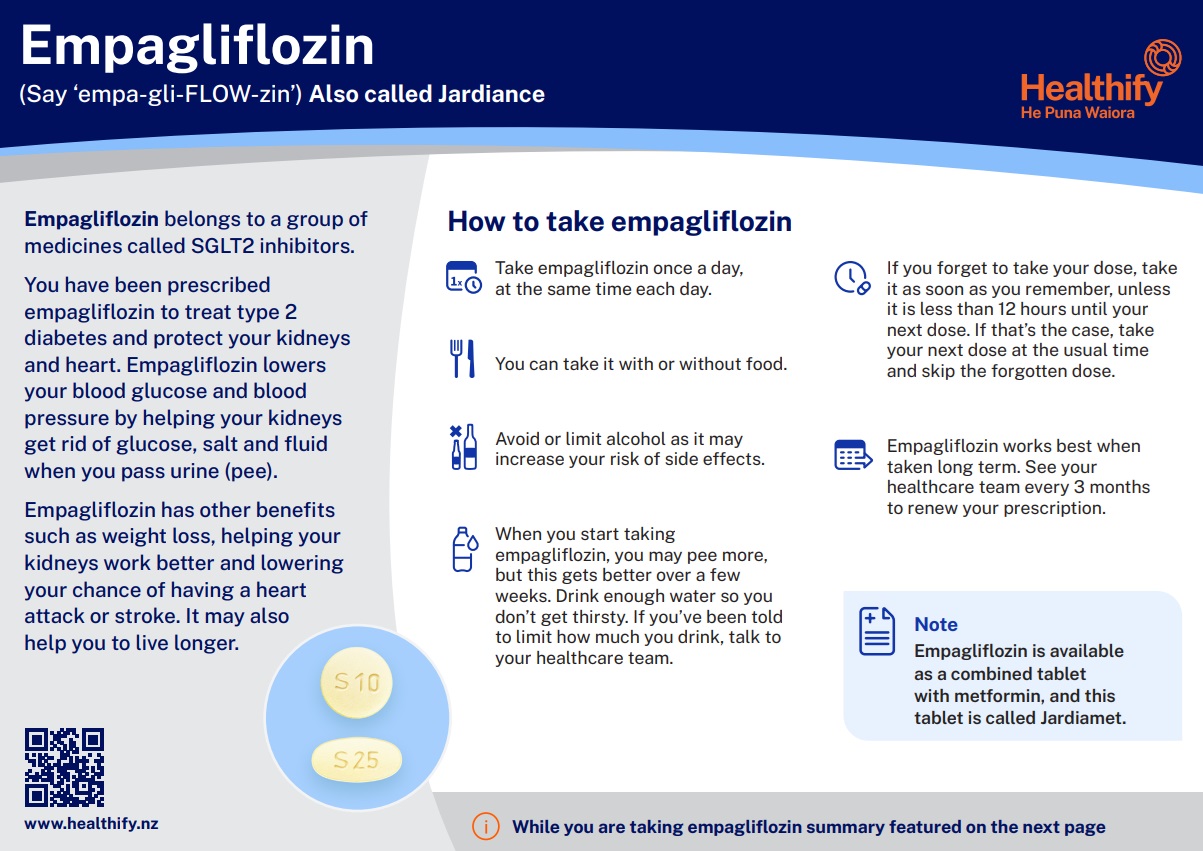
- Empagliflozin (Jardiance®).
- Empagliflozin + metformin (Jardiamet®).
- Gliclazide (Glizide®).
- Glipizide (Minidiab®).
- Glibenclamide (Daonil®).
- Acarbose (Glucobay®, Accarb®).
- Pioglitazone (Vexazone®).
Diabetes medicines available as an injection
The following medicines for type 2 diabetes are available as injections which are given under your skin.
- Dulaglutide (Trulicity®).
- Liraglutide (Victoza®).
- Insulin.
Dulaglutide and liraglutide are available as injections but they are NOT the same as insulin. They work in a different way, by increasing the release of insulin from the pancreas when blood glucose is high. They also slow down how quickly food is absorbed and reduce your appetite. These medicines help to reduce blood glucose levels, and promote weight loss. Dulaglutide is given once a week.
Insulin injections are used when your blood glucose levels have not been lowered successfully with other medicines. This is usually when your body no longer produces enough insulin. Insulin as a medicine is very similar to natural human insulin. It cannot be given as tablets because enzymes in your stomach destroy it. There are different types of insulin. Read more about insulin.
Taking diabetes medicines as prescribed, especially with a healthy diet, exercise and weight management, can make a big difference in your overall health and wellbeing. Here are the many benefits:
Better glucose management
Diabetes medicine helps to keep glucose within the target range, preventing levels that are too high (hyperglycemia) and too low (hypoglycemia). Stable blood glucose can lead to more energy, better mood, and fewer diabetes-related symptoms.
Weight loss
Some diabetes medicines such as metformin, empagliflozin, liraglutide and dulaglutide can help you lose weight. If you're overweight, weight loss makes it easier to control your blood glucose and improve your overall health.
Prevent or delay complications of diabetes
People with poorly managed diabetes have a higher risk of major health complications. Many complications develop slowly and without clear symptoms, which is why taking your diabetes medicines as prescribed and keeping regular healthcare provider visits, even if you feel well, are so important. Early care and proper medicine use can prevent or delay these problems and help you stay healthier longer.
- Heart disease and stroke: People with diabetes are twice as likely to have heart problems or a stroke compared to those without diabetes.
- Eye problems: Diabetes can damage the tiny blood vessels in the eyes, causing diabetic retinopathy. It can also lead to cataracts (cloudy lenses) and glaucoma (increased pressure inside the eye).
- Kidney disease: High blood glucose can harm the kidneys and cause chronic kidney disease (CKD). If untreated, CKD can lead to kidney failure. About 1 in 3 adults with diabetes develop CKD.
- Nerve damage (neuropathy): Nerve damage is common in diabetes and can cause numbness, tingling, or pain, usually in the feet and legs. It may also affect digestion, blood vessels, and the heart.
- Risk of infections: People with diabetes are more likely to get infections because high blood glucose weakens the immune system, making it harder for the body to fight germs. This means infections can happen more often and may be more serious or take longer to heal. Cuts, sores, or blisters are more likely to get infected. You're more likely to get the flu, chest infections and urinary tract infections.
- Amputations: Damage to blood vessels and nerves in the feet can cause serious infections that are hard to treat. Sometimes, amputation is necessary to stop infections from spreading.
- Gum disease: This can cause tooth loss and make blood sugar harder to control.
- Low mood: Diabetes raises the risk of depression, especially as more health problems develop.
Improved overall health
Many diabetes complications share similar risk factors, and having one complication can make others worse. For example, high blood pressure is common in people with diabetes and can make eye and kidney problems more severe. Diabetes also tends to lower “good” cholesterol (HDL) and raise triglycerides and “bad” cholesterol (LDL), which increases the chance of heart disease and stroke. Also, if you have diabetes and smoke, your risk of heart disease is twice as high.
Taking diabetes medicines along with managing your blood pressure, controlling high cholesterol, and quitting smoking can greatly reduce your risk of serious complications like heart disease, stroke, kidney problems, and vision loss. This helps protect your whole body by keeping your blood glucose, blood pressure, and cholesterol at healthy levels, to give you the best chance to live a longer, healthier life with diabetes.
Here are some of the things you and your healthcare provider may consider when deciding on the best treatment for you.
Your blood glucose levels: Most people with type 2 diabetes are started on metformin tablets. If you're unable to take metformin because of side effects or other reasons, or if your blood glucose level is not successfully lowered with metformin alone, your healthcare provider may add in other medicines that act in different ways to lower your blood glucose levels.
Other health conditions: Some other conditions you might have along with diabetes can affect how well your medicines control your blood glucose, including:
- obesity
- high blood pressure
- high cholesterol
- heart disease
- kidney disease.
Funding: Some newer diabetes medicines such as empagliflozin, liraglutide and dulaglutide are funded for people with diabetes if they meet certain criteria (also called a special authority). Read more about a special authority.
Side effects: When deciding on the best medicine for you, discuss with your healthcare provider the possible side effects of the medicine and how these are likely to affect you or your lifestyle, such as weight changes or the risk of hypoglycaemia (low blood glucose).
Understanding what your medicines are for and how to take them helps ensure you get the most benefit from them. Here are some questions that you might ask your healthcare provider.
About your medicine
- What's the name of my medicine and what does it do?
- What's the strength (eg, how many milligrams or units)?
- How much should I take for each dose?
- When and how often should I take my medicine?
- Should I take it with food?
- Is it okay to take with other medicines, alcohol or natural remedies?
- Will this medicine affect other health conditions I have?
- How should I store this medicine (eg, room temperature, refrigerator)?
Missed meals or doses or feeling unwell
- What should I do if I forget to take a dose?
- What should I do if I miss a meal?
- Do I still keep taking these medicines when I'm sick and not eating normally?
Monitoring
- How soon should I expect the medicine to start working, and how will I know it is working?
- What should I do if the medicine doesn’t seem to be working?
- Do I still need to keep taking the medicine if I feel better?
Side effects
- Are there any side effects to watch out for?
- Can my diabetes medicine cause low blood glucose?
- What should I do if my blood glucose is too low?
Learn more
Return to the main diabetes page.
Brochures
Empagliflozin factsheet – English(external link), Chinese (traditional), (external link)Chinese (simplified), (external link)Hindi,(external link) Samoan(external link), Te reo Māori(external link), Tongan(external link)
Sick day management with type 2 diabetes(external link) Aotearoa Diabetes Collective, 2025
References
- Treatment of diabetes(external link) NZ Formulary
- Type 2 Diabetes Management Guidance(external link) New Zealand Society for the study of diabetes (NZSSD)
Brochures
Healthify He Puna Waiora, NZ, 2025
English, Te reo Māori, Samoan, Tongan,Chinese (simplified), Chinese (traditional), Hindi

Sick day management – Type 2 diabetes
Aotearoa Diabetes Collective, 2025

At home sick day advice
Health New Zealand | Te Whatu Ora, 2023
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Claire Salter, Clinical Pharmacist, Tauranga; Angela Lambie, Pharmacist, Auckland
Last reviewed:





