- If you’re worried your child or teenager may be depressed, see your family doctor. Depression is a treatable illness and the sooner your child or teenager gets treatment, the sooner they will start to feel better.
- There is a range of effective treatments for depression. These usually focus on talk therapy and lifestyle changes. There are also heaps of great community and online programmes and support groups available.
- There are lots of things you as a parent can do to help: start a conversation if you notice ongoing changes in their mood, support their emotional wellbeing by prioritising a healthy lifestyle at home, and reduce conflict and hostility at home, which are known to make low mood worse in young people.
- Depression is a key risk factor for suicide in young people, especially if they are feeling hopeless or stuck and that things won't change. If they are having thoughts about no longer wanting to be alive, get help from your doctor or free phone or text 1737(external link)(external link)(external link) from any landline or mobile phone, 24 hours a day, 7 days a week.
Low or no data? Visit Zero Data then search for 'Healthify'. Click on our logo to return to our site and browse for free.
Depression – children and teenagers
How to support a child or teenager with depression
Key points about depression in children and teenagers
- Depression (mate pāpouri) doesn't just affect adults – it also happens in childhood and teenage years.
- If your child or teenager is feeling depressed, the sooner they talk to someone who can help them, the better.
- The longer it goes on, the harder it is to recover from.
- There is lots of help available.

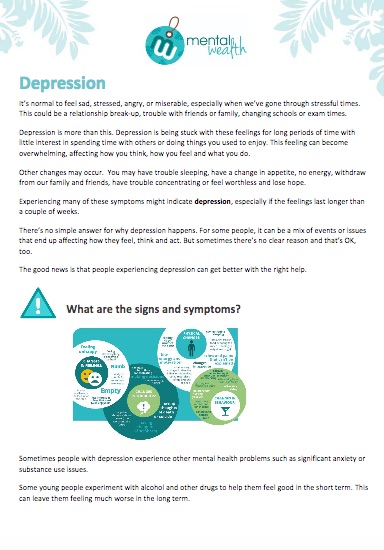
One or two of the following signs of depression may be just part of growing up. However, if your child or teenager has had several of them over the past few months and it’s making they're making it hard for them to do everyday things (like study or socialise), depression is a possibility. However, it’s important to consider other causes too.
Symptoms can include:
- being irritable and snapping at others
- low, sad or depressed mood that doesn't go away
- crying easily and often
- lacking concentration and interest in school work, and may stop wanting to go to school
- feeling tired all the time
- feeling stressed or anxious
- unable to sit still, but pacing and wringing their hands
- lacking interest in usual activities
- being forgetful
- not being able to sleep or wanting to sleep more than usual for their age
- having other sleep problems, eg, staying up late into the night and sleeping during the day, or waking often during the night
- sitting in one place for long periods, moving, responding and talking very slowly
- withdrawing from usual social contact
- being quiet and withdrawn at home
- losing their appetite or eating more resulting in weight loss or gain
- experiencing muscle tension and headaches
- experiencing unexplained physical complaints, especially stomach pains.
Depression in young people can present as irritability and anger. They may ask you to back off or go away. This anger can be mistaken for teenage rebelliousness or an irritable child with behaviour difficulties.
Young people may not recognise their problem as depression or, if they do, may feel unable to talk about it. Often the feelings that come with depression are so strong they do not tell anyone else because they feel no good, they are scared they are going mad, or they think that no one will believe or support them. They may choose to tell their friends before they’re able to talk to adults. Therefore, if you notice these symptoms, ask your children about them.
There is a strong association between depression in young people and anxiety, conduct disorders, substance abuse, attention-deficit/hyperactivity disorder (ADHD) and eating disorders. These other problems can co-exist with depression or present in a similar way to depression. This is another reason to see a doctor as soon as possible if you have any concerns about the mental health of your child or teenager.
Usually, there is no one single cause of depression in children and teenagers. Sometimes depression appears out of the blue, while at other times something seems to trigger it. Often it is a combination of factors. Your child or teenager is more likely to experience depression if they:
- experience a stressful event such as the break-up of parents, loss of a loved one or relationship break-up
- have someone in the family who has depression, such as a parent or sibling
- have experienced trauma, such as a significant injury or accident, or abuse
- are going through major life changes, such as starting a new school or going to university
- have significant physical illnesses
- have a poor daily routine or are not involved in education, training or work
- have been bullied or had other problems with peers
- are LGBTI or feel different in some other way
- use alcohol or recreational drugs.
You can help your child or teenager by starting conversations if you notice ongoing changes in their mood. Even better, create a family culture of talking about feelings – you don’t need to wait for things to be hard to start this.
You can support their emotional wellbeing by making sure you all have a healthy lifestyle at home: having meals together, eating healthy food, having daily physical activity, limiting screen time and making sure they get plenty of sleep. A great way to do this is modelling for your children behaviours you’d like to see them taking on, eg, putting your own phone away at mealtimes, talking about how your day is going, making sure you get some exercise.
Conflict and hostility at home are known factors that can make low mood worse in young people. On the other hand, working together with other family members supports children’s emotional wellbeing. Relationship break-downs do happen, but if you are going through a separation or divorce, do your best to ensure your child feels secure and loved, and speak respectfully about the other parent in front of them.
If you’re worried your child or teenager may be depressed, see your family doctor. They will ask your child questions about their thoughts, feelings and behaviour, including sleeping and eating patterns, as well as how long they have been feeling this way. They will also ask if the young person has had any previous episodes of depression and may ask about what is happening in their life at the moment. They may also do a physical examination and blood tests to rule out other causes for their depression.
It is important to involve family members where possible when assessing and treating depression. This can become more challenging with adolescents, although remains very important. For young people under 16 years old, parents need to be involved in the consent process.
The good news is that there is a range of effective treatments for depression – it's a treatable illness. Treatment usually focuses on psychological therapies and lifestyle changes. Antidepressants are not routinely used for children and young people but may be added in some cases if depression doesn't respond to other treatments. Your GP will be able to talk through options and help work out which are best for your child or teenager. They may also refer them to a mental health specialist. Read more about mental health services for youth below.
Talking therapy
The most common treatment is talking therapy. Counsellors and therapists will be supportive and understand what is happening to your child and know how to help them. They can offer help with thinking patterns and anxiety, problem-solving skills and self-esteem, as well as any other problems that might be contributing to their depression. Some of the therapy sessions may involve the child or teenager on their own and some usually involve meetings with parents and/or other family/whānau members.
Your GP will know what counselling and therapy is available in your local area. This is free for children under 14, while 14 to 25-year-olds can get free primary care services through their local Youth One Stop Shop.
If your child or teenager is at school, they can talk to a school guidance counsellor or your Hauora Youth mental health worker. Some areas in Aotearoa New Zealand have services for Māori, Pacific Peoples and Asian youth – ask your school counsellor about these services.
Online programmes
Your doctor might recommend that your child or teenager access an online skills programme to help with treatment of depression. Some of these have been developed in collaboration with therapists and researchers and have been supported by research. However, one of the downsides to this is that it may take young people away from being able to share problems with others, which can be helpful in its own right.
Evidence-based tools developed for a New Zealand-context include:
- SPARX(external link)(external link) A free online tool to help young New Zealanders learn to deal with depression and anxiety.
- The Lowdown(external link)(external link) A website created to help young people understand and deal with depression, with chat room, personal stories, music and more.
- Aunty Dee(external link)(external link) Online problem-solving tool for young people.
Find more depression apps and e-learning.
Lifestyle changes
Improvements to key aspects of lifestyle can greatly affect mood: sleep, food, exercise and the use of alcohol or drugs. As a parent, you can help your child or teenager by supporting them to have a healthy lifestyle. Focus on their basic needs – healthy eating, physical activity and plenty of sleep. Spend time together as a family, such as daily meals and weekly outings, and limit their screen time.
Medication
Sometimes, with more severe depression, medication may be recommended. While antidepressants do not cure depression, if psychological therapy and lifestyle changes alone have not been effective, your doctor may add an antidepressant to your child or teenager's treatment plan.
Note: The use of antidepressants has been linked with suicidal thoughts and behaviour. Children, teenagers, young adults and people with a history of suicidal behaviour are particularly at risk. This is most likely during the first few weeks of starting the antidepressant or if the dose is changed. It is important to look out for signs of suicidal behaviour such as a young person talking about suicide, an increase in self-harm, worsening of low mood, agitation or aggression. If you notice any of these signs, contact your doctor as soon as possible.
Apps reviewed by Healthify
You may find it useful to look at some Depression apps and Mental health and wellbeing apps.
Find out where you can get support with depression.
Online support
The Lowdown(external link)(external link) website has been created to help youth understand and deal with depression. FREE text 5626 or chat online(external link)(external link)
SPARX(external link)(external link) helps young people learn skills to deal with feeling down, depressed or stressed.
What’s Up(external link)(external link) is a safe place for children and young people to about anything at all. FREE call 0800 WHATS UP (0800 942 8787) from any NZ phone or chat online(external link)(external link)
Small Steps(external link)(external link) Whether you’re looking to maintain wellbeing, find relief or get help, Small Steps can support you and your whānau with practical tools, strategies and advice.
Helplines
The following numbers are free to call from a New Zealand landline:
Free call or text 1737(external link)(external link) any time, 24 hours a day
Youthline(external link) (0800 376 633) Free helplines 24/7 – free TXT 234, free call 0800 37 66 33, chat online(external link) (10am – 10pm) or email. Youthline provides access to support and help for young people, as well as youth development and leadership programmes. They also offer a counselling service(external link) with up to 8 free counselling sessions (over the phone, face-to-face or via video call), in Auckland.
Kidsline(external link)(external link) 0800 543 754 (4pm–9pm weekdays)
Depression line(external link) 0800 111 757 (24 hours, 7 days)
Lifeline(external link)(external link) 24 hour telephone counselling 0800 543 354 or 09 522 2999 (within Auckland)
What’s Up(external link)(external link) 0800 WHATS UP (0800 942 8787) 12pm-11pm Monday to Friday, 3pm-11pm Weekends, Free to call from both NZ landlines and mobile phones.
Samaritans(external link)(external link) 0800 726 666 (24 hours, 7 days)
What to do if you or a friend is depressed
Living well with depression
Antidepressants
Suicide prevention
Kessler-10 (K10) distress scale
Anxiety | Mate māharahara
Stress | Mate māharahara
Addiction
Eating disorders
Self-harm
ADHD in children | Aroreretini
Physical activity and mental health
Alcohol and mental health
Mental health for kids
The following links provide further information about depression in children and teenagers. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Common ground(external link) A website for parents, whānau and friends to recognise and understand the difficult situations that young people go through in their lives
Depression(external link) KidsHealth, NZ, 2016
Find out how to tell if someone is struggling with their mental health(external link) BBC, UK, 2021
Depression(external link) Black Dog Institute, Australia
Depression – youth(external link) Mental Health Foundation, NZ, 2014
depression.org.nz(external link)
Depression - for young people(external link) Women and Children's Health Network Australia
Understanding and dealing with depression – for young people(external link) Headspace Australia
Kick depression(external link) Download a free e-book of scientifically proven ways to get through stuff
Mental Wealth(external link) NZ
Just a thought(external link) NZ
Brochures
- How you can help someone with depression(external link) The Lowdown, NZ
- Facts about young New Zealanders and depression(external link) The Lowdown, NZ
- Supporting young people with stress, anxiety and/or depression(external link) Ministry of Social Development, NZ, 2015
- Helplines and local mental health services (external link)Mental Health Foundation, NZ, 2021
- Depression in adolescents and young people(external link) Black Dog Institute, Australia, 2012
Note: This resource is from overseas so some details may be different in New Zealand, eg, phone 111 for emergencies or, if it’s not an emergency, freephone Healthline 0800 611 116. - There is a way through(external link) Health Promotion Agency, NZ, 2019
- Depression factsheet(external link) Mental Wealth, NZ, 2019
- How you can help someone with depression(external link) The Lowdown, NZ
- Options for dealing with depression(external link) The Lowdown, NZ
- Help for the tough times(external link) Health Promotion Agency, NZ, 2016
- A guide to talking therapies in NZ(external link) Te Pou, NZ
- Talking mental health with young people at secondary school(external link) Anna Freud, National Centre for Children & Families
Apps/tools
Kessler scale
General anxiety scale (GAD-7)
Depression apps
Mental health and wellbeing apps
References
- Facts about young New Zealanders and depression(external link) the Lowdown, NZ
- Depression in the LGBT population(external link) Healthline, US, 2016
- Online insomnia treatment also prevents depression(external link) Black Dog Institute, Australia, 2016
- One hour of exercise a week can prevent depression(external link) Black Dog Institute, Australia, 2017
Resources
The role of medicines in the management of depression in primary care(external link) BPAC, NZ, 2017
The role of medicines for the treatment of depression and anxiety in patients aged under 18 years(external link) BPAC, NZ, 2016
Addressing mental health and wellbeing in young people(external link) BPAC, NZ, 2015
Managing frequently encountered mental health problems in young people - non-pharmacological strategies(external link) BPAC, NZ, 2015
Depression information sheets(external link) Centre for Clinical Interventions, Australia
PHQ-9 (Patient Health Questionnaire 9)
Kessler-10 (K10) depression scale
General anxiety disorder scale (GAD-7)
See our page Depression for healthcare providers
Stay alert for suicidal thoughts with SSRIs
Concerns have been raised about the potential for antidepressants, particularly SSRIs, to cause suicidal thoughts and behaviour especially in adolescents and young adults. These concerns have prompted regulatory authorities in many countries to issue warnings. Australian and New Zealand Journal of Psychiatry 2015, Vol. 49(12) 1-185.
A consensus statement by the World Psychiatric Association (WPA) (Möller et al., 2008) concluded that in the absence of randomised controlled trial evidence, the risk is difficult to assess but that the available data indicated that there was a small risk of SSRIs inducing suicidal thoughts in patients up to the age of 25.
The WPA advised that this risk needed to be balanced against the known benefits of treating depression and in preventing suicide. Clinicians should therefore advise young patients and their families of the small chance of suicidal thoughts emerging during the early phase of treatment with SSRIs and monitor all patients for the emergence or worsening of suicidal thoughts during the first 2–4 weeks of treatment.
The activation/agitation observed with the initial stages of taking an SSRI can be managed with a low dose of a benzodiazepine prescribed for a limited period of time. Clinical practice guidelines for mood disorders(external link) Royal Australian and New Zealand College of Psychiatrists, 2015
Podcast
Depression in adolescents – Sally Merry(external link) Goodfellow Unit, 2017
Professor Sally Merry talks about depression in adolescents. Sally holds the Cure Kids Duke Family Chair and is head of Department of Psychological Medicine at The University of Auckland.
Apps
Brochures
Mental Wealth, NZ, 2019

Mental Health Foundation, NZ, 2022
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr David Chinn, child and adolescent psychiatrist; Tania Stanton, clinical psychologist; and Rewa Murphy, clinical psychologist
Last reviewed:
Page last updated:





