You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Migraine medicines
Key points about migraine medicines
- Migraine treatment is aimed at stopping symptoms and preventing attacks.
- There are many medicines available to help ease the symptoms of migraine.
- It may take time to work out the best way to manage your migraines. Management can include lifestyle changes and medicines.
- You may need to try different types or combinations of medicines before you find the most effective ones.

Medicines for migraine are aimed at stopping an attack once it starts and preventing attacks in the future. It’s a good idea to talk to your healthcare provider about a migraine plan to show you which medicines to take and how often, and any lifestyle changes you can make.
You may need to try different types or combinations of medicines before you find which ones work best for you. Some people have migraines several times a week. Other people only have occasional migraines. It's also possible for years to pass between migraine attacks. Read more about migraine.
Medicines to treat a migraine
- If you feel a migraine attack starting, you may be able to stop the attack by taking pain-relief medicines, eg, paracetamol, NSAIDs, and triptans.
- The earlier you take them, the more likely they are to work.
- You may need a combination of pain medicines.
- Many people get nausea or vomiting when their migraine starts. Anti-nausea medicines (also called antiemetics) can be effective even if you don't experience nausea or vomiting. They can be taken together with pain-relief medicines and triptans.
- It's important not to take pain-relieving medicines too often since this can make things worse and lead to 'medication-overuse headache'.
- If you need to take migraine relief medicine several times a month, talk to your doctor about preventive treatments.
- Read more below about pain relief medicines – paracetamol, NSAIDs and triptans.
Medicines to prevent migraine
- If you get 2 or more migraines a month, your healthcare provider may suggest you try a preventive medicine.
- There are many different medicines that can reduce how often you get a migraine attack and how severe they are.
- Read more below about medicines to prevent migraine.
Paracetamol
Paracetamol can be an effective pain reliever, especially for mild symptoms. It can be used alone or in combination with another medicine, eg, ibuprofen. Paracetamol and ibuprofen are available in different strengths and brand names.
Paracetamol is mostly a safe option if you don't take more than 4 grams (or 8 tablets) per day. Too much paracetamol can harm your liver and may cause severe liver damage. Accidental overdose can happen because many different products include paracetamol so, if you are taking more than 1 medicine, make sure you check the label for ingredients. Read more about paracetamol.
Note: Paracetamol shouldn't be taken for headaches on more than 15 days per month. Frequent use can cause medication-overuse headache. Read more about medication-overuse headaches below.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Examples of NSAIDs are ibuprofen, diclofenac, naproxen and aspirin.
NSAIDs are most effective if taken at the first signs of a migraine. It's best not to wait until the headache worsens before taking NSAIDs. Some people find one type of NSAID to be more effective than another, so it's worth trying different ones to find what's best for you.
Some NSAIDs need to be prescribed and some can be bought from a pharmacy or supermarket. There are some risks with taking NSAIDs so check with your healthcare provider whether NSAIDs are a safe option for you. Read more about NSAIDs.
Note: NSAIDs shouldn't be taken for headaches on more than 15 days per month. Frequent use can cause medication-overuse headache. Read more about medication-overuse headaches below.
Triptans
Examples of triptans are rizatriptan, sumatriptan tablets and sumatriptan injection.
Triptans are a group of medicines used for migraine attack and cluster headaches. Triptans are most effective if they're taken early in a migraine attack while the pain is still mild. It's not clear whether treatment during the aura phase is as effective. Triptans work by stimulating serotonin receptors causing certain blood vessels to contract (narrow) and stopping other chemicals called neurotransmitters being released.
Triptans aren't suitable for everyone. They shouldn't be taken by people with heart disease, chest pain (angina), and severe high blood pressure.
Read more about triptans.
Note: Triptans shouldn't be taken for headaches on more than 9 days per month. Frequent use can cause medication-overuse headache. Read more about medication-overuse headaches below.
Examples of medicines for nausea (feeling sick) are metoclopramide, domperidone and prochlorperazine.
These medicines are called anti-sickness medicines or antiemetics. They're prescribed by your healthcare provider and can be used together with other pain relievers and triptans. Many people get nausea or vomiting when their migraine starts. Anti-sickness medicine can be effective in treating migraine (even if you don't experience nausea or vomiting).
As with pain relievers, anti-sickness medicines work better if taken as soon as your migraine symptoms begin. They usually come as tablets to swallow, but some tablets are made to dissolve in the mouth and some medicines come as suppositories inserted into your rectum (bottom).
Some people with migraine are given strong painkillers, called opioids, to treat migraines. Examples of opioid painkillers available in Aotearoa New Zealand include codeine, tramadol, morphine, oxycodone, fentanyl and pethidine. However, opioids aren't the preferred medicine to relieve migraines:
- They can make headaches worse: Using opioids for migraine can cause more headaches and migraines than you had to begin with. This is called ‘medication-overuse headache’. It's possible with all pain medicines but is more likely with opioids.
- They aren't as effective as other migraine medicines: There are medicines that are better than opioids to reduce the number of migraines you have and how severe they are. More effective medicines are triptans which work directly on the blood vessels in your head to relieve the pain from migraine.
- They can be harmful: Opioids are strong medicines that may cause you harm, including dependence and addiction. Opioids can cause serious withdrawal symptoms if you stop taking them suddenly. People who use high doses for a long time may need to go to hospital to stop using them. Opioids, even at low doses, can make you feel sleepy or dizzy. Other side effects include constipation and nausea. Using them for a long time can lower your sex drive and cause depression and sleep problems.
But, opioids may be needed in some cases
- For some people, other medicines don’t work. Opioid painkillers may be a short-term ‘rescue’ option for these people. If you need opioids for migraine, you shouldn't take them for more than 9 days per month. At the same time, you and your healthcare provider should focus on other strategies to help you prevent and manage your migraines. Long-term follow-up is needed to make sure you don't develop complications from taking opioids.
- If you have certain medical conditions (eg, some heart diseases) or if you're pregnant, you may not be able to take other migraine medicines. Talk to your healthcare provider if this applies to you.
Read more about treating migraine headaches and why some drugs should rarely be used(external link).
Medication-overuse headache can occur if you use pain relief medicines to treat headaches and migraines over a long time. If you've been using triptans, paracetamol, NSAIDs or opioid medicines regularly for 3 months or more, and you're having headaches more than 15 days per month, then you may be experiencing medication-overuse headache. It may feel like a tension-type headache or migraine-like attack.
Medication-overuse headache is sometimes called medication adaptation headache or rebound headache. Headaches often improve within 2 months of withdrawal of the overused medicine but can feel worse before improvement is seen. If you think you might have medication adaptation headaches it's really important to keep a detailed history of your headaches and how often you're taking medicines for the headaches. You can use a headache diary to help you keep a record. You can also talk to your healthcare provider about medicine to prevent migraines. See the section below.
To avoid medication-overuse headache:
- triptans and opioids shouldn't be used for more than 9 days per month
- paracetamol and NSAIDs shouldn't be taken for headaches more than 14 days per month.
Preventive medicines are taken daily to stop migraine attacks from happening. They're not used to treat an acute attack. Medicines to prevent migraines are an option if you:
- have at least 2 attacks a month
- have a significantly reduced quality of life even with treatment for migraine
- can't take treatment for migraine attacks.
Preventive medicines help to lessen the severity, the length of attacks, and how often you get them. They reduce disruption to your daily activities and reduce overuse of acute medicines. They must be taken every day to be effective and they may take a few weeks to start working. Many different preventive medicines are available. Which one is best for you depends on things such as:
- other medical conditions you have, including high blood pressure, asthma, diabetes or pregnancy (among others)
- the potential side effects of the medicine
- your response to preventive medicines if you've used them before.
Beta-blockers
- Examples include propranolol, atenolol, nadolol, metoprolol and timolol.
- These medicines are mostly used to treat high blood pressure but they do have other uses.
- Common side effects include tiredness and depression.
- Read more about beta-blockers.
Candesartan
- Candesartan is usually used for high blood pressure.
- It should not be used if you're pregnant or trying for a baby.
- Candesartan can cause dizziness and falls (due to low blood pressure), tiredness and cough.
- Read more about candesartan.
Antidepressants
- Examples include amitriptyline and nortriptyline.
- These medicines are also used to treat depression, pain and other conditions.
- Common side effects include weight gain, dry mouth, feeling sleepy, tiredness and decreased libido (sex drive).
Anti-seizure medicines
- Examples include topiramate and sodium valproate.
- These medicines are mostly used to treat epilepsy but they have many other uses.
- Common side effects include weight gain or loss, drowsiness and skin rash.
- Sodium valproate and topiramate must NOT be taken during pregnancy and should be avoided in any person who could become pregnant or cause a pregnancy, because of the risks of birth defects. For more detailed information, read:
- If you're taking anti-seizure medicines for migraine prevention and could become pregnant, it's recommended you use 2 forms of contraception.
CGRP inhibitors
CGRP inhibitors are medicines that block the action of calcitonin gene-related peptide (CGRP). Increased levels of CGRP have been linked to migraine. There are two types of CGRP inhibitors. They are not funded in Aotearoa New Zealand.
- CGRP receptor blockers: For example, atogepant (Aquipta), which comes as tablets. It’s used in people who have 4 or more migraine days per month.
- CGRP monoclonal antibodies: Examples include erenumab and galcanezumab (Emgality). They are both injections.
Pizotifen
- Some people find pizotifen (Sandomigran) tablets helpful in preventing migraine.
- Common side effects include an increased appetite, weight gain and feeling sleepy.
Supplements
- Some people may find taking supplements such as magnesium, Coenzyme Q10 or riboflavin (vitamin B2) helpful, but there is limited evidence for their effectiveness.
- If you're considering taking a supplement, let your healthcare provider know. They can check interactions with your prescribed medicines or other treatments and any safety concerns.
Brochures
Medicines and side effects [PDF, 91 KB] Healthify He Puna Waiora, NZ, 2024
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
- Treatment of acute migraine(external link) NZ Formulary(external link)
- Prophylaxis of migraine(external link) NZ Formulary(external link)
- The role of triptans in the treatment of migraine in adults(external link) BPAC, NZ, 2014(external link)
- Medication overuse headache(external link) The Migraine Trust, UK
Brochures
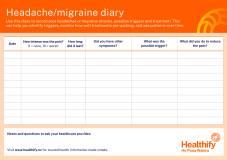
Headache/migraine diary
Healthify He Puna Waiora, NZ, 2026
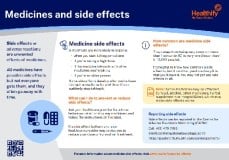
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024

Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Ray Bose, Neurologist, Auckland
Last reviewed:
Page last updated:





