You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Atorvastatin
Sounds like 'a-tor-va-stat-in'
Key points about atorvastatin
- Atorvastatin is used to lower cholesterol and reduce your chance of heart disease and stroke.
- Atorvastatin is also called Lorstat®.
- It belongs to a group of medicines known as statins.
- Find out how to take it safely and possible side effects.

Atorvastatin is a medicine that reduces the amount of cholesterol made by your body by blocking the action of an enzyme needed to make cholesterol. It belongs to a group of medicines known as statins. Taking atorvastatin has many benefits. Apart from lowering cholesterol, it helps protect your heart and reduces the risk of heart attack and stroke.
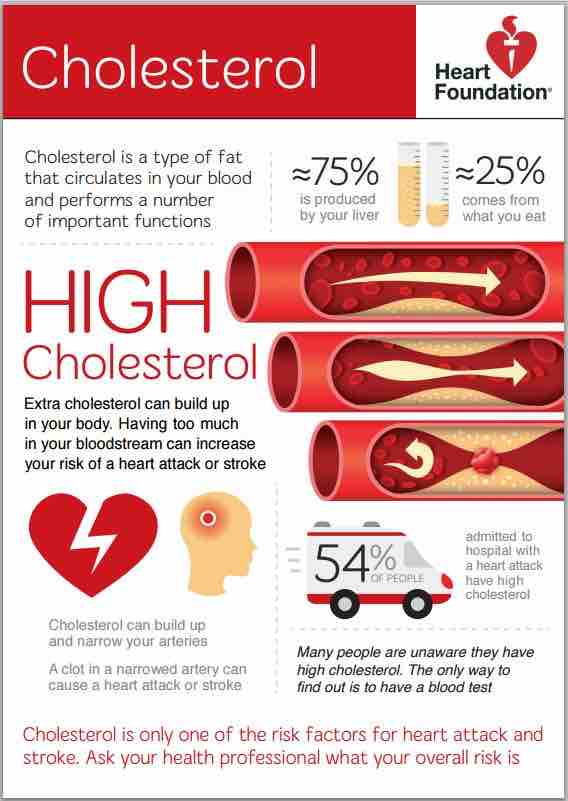
If you have high cholesterol
Atorvastatin is used to lower raised cholesterol. Having high cholesterol increases your risk of cardiovascular disease and having a heart attack or stroke. Read more about high cholesterol.
- Cholesterol is a type of lipid made by your liver and from the fatty foods that you eat. Everyone has cholesterol and triglycerides in their blood. They're needed for many things such as hormone production and brain function.
- Your body needs some cholesterol but if the amount in your blood gets too high, it can cause small fatty patches called plaques (or atheroma) to form.
- Over time, these patches can build up and make the blood vessels narrow and stiff (a process called atherosclerosis). The narrowing reduces the blood flow through your arteries and can cause heart attack, angina and stroke.
- Atorvastatin helps to reduce atherosclerosis and reduces your risk of having a heart attack or stroke.
For people with normal cholesterol who are at risk of heart disease and stroke
Atorvastatin can also reduce your chance of heart disease and stroke if you have an increased risk of it, even if your cholesterol levels are normal. It is especially recommended for people who already show signs of heart disease, such as angina (chest pain), or who have experienced a mini-stroke (also known as a transient ischemic attack or TIA).
- When deciding whether you should take a statin or not, your doctor will look at your overall risk of having a heart attack or stroke in the future.
- They work out your individual risk, including information on your age, sex, ethnicity, blood pressure, whether you smoke and if you have diabetes. Read more about heart risk assessment.
- If your overall risk of having a heart attack or stroke is high, even if your cholesterol level is normal, a statin may be recommended. This is because there may already be fatty plaques in your arteries which increases your risk of cardiovascular disease.
Note: Taking a statin, such as atorvastatin is just one way to reduce your risk of cardiovascular disease. Making lifestyle changes including eating a healthy diet, staying active, staying at a healthy weight, drinking less alcohol, and not smoking can also reduce your risk of cardiovascular disease.
After a heart attack or stroke
If you’ve had a heart attack or stroke, you are at high risk of having another. Keeping your cholesterol low with the help of statins reduces the buildup of plaque (fatty deposits) in your arteries, helping to prevent further heart attacks or strokes. In some people atorvastatin may be used at higher doses soon after a heart attack or stroke. Higher doses reduce the fat content of plaques and stabilises them, making them less likely to rupture (break open) and cause another event.
VIDEO: Statins – What you need to know
Atorvastatin tablets are available in different strengths; 10 mg, 20 mg, 40 mg and 80 mg.
- Always take your atorvastatin exactly as your prescriber has told you.
- The dose of atorvastatin will depend on your cardiovascular disease (CVD) risk, which is calculated by completing a heart risk assessment. Your healthcare provider will discuss your CVD risk with you to determine what dose of atorvastatin is best for you.
- After a heart attack or stroke, you may be started on a high dose of atorvastatin (40 mg to up to 80 mg once daily).
- The pharmacy label on your medicine will tell you how much atorvastatin to take, how often to take it and any special instructions.
- Timing: Take atorvastatin once a day, at around the same time each day.
- Food: You can take atorvastatin with or without food.
- Missed dose: If you forget your dose, take it as soon as you remember that day. But if it's nearly time for your next dose, just take the next dose at the usual time. Don't take double the dose.
Here are some things to know when you're taking atorvastatin. Other things may be important as well, so ask your healthcare provider what you should know about.
- Alcohol: Avoid drinking large amounts of alcohol while you're taking atorvastatin. Heavy drinking can increase your risk of side effects, such as problems with your liver.
- Avoid large quantities of grapefruit: Having large quantities of grapefruit while taking atorvastatin can increase your risk of side effects. But eating 1 serving of marmalade, no more than half a grapefruit or drinking no more than a standard glass (250 mL) of grapefruit juice each day, shouldn't be a problem. It's best to allow 12 hours between having these foods and taking your atorvastatin dose, so if you take your statin in the morning have your grapefruit at night.
- Monitoring: You may need to see your healthcare provider regularly when you first start taking atorvastatin to make sure the dose is right for you. High cholesterol doesn’t have any symptoms so you won’t notice any changes after taking atorvastatin. That's why it’s important to have a blood test to check the changes in your cholesterol levels.
- Keep taking atorvastatin regularly: To reduce your cholesterol effectively, you must keep taking atorvastatin every day. Treatment with atorvastatin is usually long term.
- Get the full benefit: To get the full benefit of a statin, it's important to eat a healthy diet, exercise regularly and limit your alcohol intake. It's best to eat a low-fat diet, and reduce the amount of saturated fat you eat. Read more about fats.
- Other medicines: Atorvastatin interacts with some medicines, herbal supplements and rongoā Māori, so check with your healthcare provider or pharmacist before starting atorvastatin or before starting any new medicines or supplements.
- Pregnancy or breastfeeding: Talk to your healthcare provider if you're pregnant, planning a pregnancy or want to breastfeed.
Like all medicines, atorvastatin can cause side effects, although not everyone gets them. If you're concerned about any symptoms you think might be related to your medicine, talk to your healthcare provider. The following information offers some guidance but doesn't include all possible side effects.
Common side effects
Tell your healthcare provider if they bother you.
- Constipation (hard to poo) or diarrhoea (runny poo), stomach upset, bloating or gas in the tummy, nausea (feeling sick).
- Problems sleeping, headache, dizziness, tiredness.
Muscle aches and pains
Some people will have muscle aches and pains when taking statins. It's difficult to determine if these symptoms are directly caused by the medicine, since aches and pains tends to become more common with age, especially if you're over 50 years of age. This side effect is rarely serious and often goes away with time. If your pain comes on shortly after you start your statin, or gets worse, see your healthcare provider. They'll check an enzyme called creatine kinase to see if the aches and pains are possibly being caused or made worse by the statins.
If so:
- a lower dose or a different statin may be prescribed, or
- you may choose to continue living with the aches because of the benefits of the statin, or
- you may discuss stopping taking your statin with your healthcare provider.
Your healthcare provider will also want to check for a rare but serious condition called rhabdomyolysis (muscle inflammation and damage). They will check any other medicines you're taking. Rhabdomyolysis can be caused by an interaction between statins and some other medicines including antibiotics.
Tell your healthcare provider immediately or phone Healthline free on 0800 611 116 if these occur
- Signs of problems with your liver such as dark coloured urine, yellowing of the skin or eyes, sharp pain in your stomach area.
- Symptoms of a serious muscle problem such as ongoing muscle weakness or pain, dark pee (urine).
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
The following links have more information on atorvastatin.
Atorvastatin(external link) (te reo Māori(external link)) NZ Formulary Patient Information
Lorstat(external link) Medsafe Consumer Information Sheet, NZ
Statins(external link) Heart Foundation, NZ
Brochures
Cholesterol(external link) Heart Foundation, NZ English(external link), Chinese(external link), Hindi(external link), Korean(external link), te reo Māori(external link), Samoan(external link), Tongan(external link)
Atorvastatin in te reo Māori(external link) My Medicines, NZ
Medicines and side effects [PDF, 91 KB] Healthify He Puna Waiora, NZ
References
- Statins(external link) New Zealand Formulary
- Atorvastatin(external link) New Zealand Formulary
- Prescribing statins to reduce cardiovascular risk(external link) BPAC, NZ, 2021
- Investigating myalgia in patients taking statins(external link) BPAC, NZ, 2014
- Cardiovascular disease risk assessment in primary care – managing lipids(external link) BPAC, NZ, 2018
Brochures
Cholesterol Heart Foundation, NZ, 2019
English, Chinese, Hindi, Korean, te reo Māori, Samoan, Tongan
My Medicines, NZ, 2023
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Johanna Lim, Clinical Pharmacist – Cardiology Expert, Health New Zealand | Te Whatu Ora Te Matau a Māui Hawke’s Bay; Angela Lambie, Pharmacist, Auckland
Last reviewed:





