Naloxone for opioid overdose
Key points about naloxone
- Naloxone is a medicine used to treat opioid overdose.
- If taken soon enough after an opioid overdose, it can save a life
- In New Zealand naloxone is available as injection. It is free and easy to access, so anyone can give naloxone in an emergency.
- Find out how to use naloxone safely and possible side effects.

Naloxone is a medicine that can save someone’s life if they’ve had an opioid overdose. Opioids are strong pain medicines, and drugs such as heroin. Examples of opioids include codeine, morphine, oxycodone, methadone, fentanyl, tramadol and heroin. Opioids slow your breathing and affect your consciousness. Taking too much can stop your breathing and cause death. Read more about opioids and who is at risk of opioid overdose.
Naloxone blocks the effects of opioids and helps a person start breathing normally again if their breathing has slowed or stopped from an overdose. It’s given as an injection and starts to work quickly, usually within a few minutes.
Opioid overdose is an emergency because it causes life-threatening problems such as slow or stopped breathing and unconsciousness.
If you are taking opioids, have a plan. Talk about overdose with people you trust before it happens. Ask your healthcare provider whether you need an emergency naloxone kit.
Note: Naloxone is only effective against an opioid overdose. It doesn't work for an overdose of other types of medicines, illicit drugs or alcohol. But, in an emergency, if you don't know the exact cause of the overdose and think it could be from opioids, it is safe to use naloxone. See below can naloxone harm someone?
Availability of naloxone in New Zealand
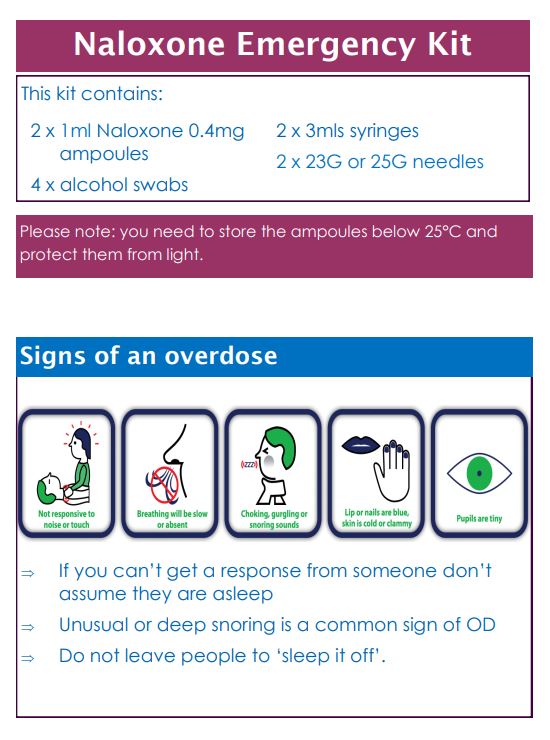
In Aotearoa New Zealand, only injectable naloxone is currently available. It works very quickly, usually within 2 to 5 minutes. The medication comes in a glass ampoule and must be injected into the muscle of a person experiencing an overdose.
You can get free injectable naloxone kits from:
- Your local needle exchange.
- Your doctor, who can prescribe it to you.
- Opioid substitution services.
Note: Nasal spray naloxone (known as Nyxoid or Narcan) is currently unavailable in New Zealand.
Naloxone is used when a person shows signs of an opioid overdose. A person may have overdosed if they:
- are very sleepy or hard to wake up (passed out)
- have little or no breathing
- are snoring deeply or making gurgling sounds
- have blue lips or nails
- have tiny pupils.
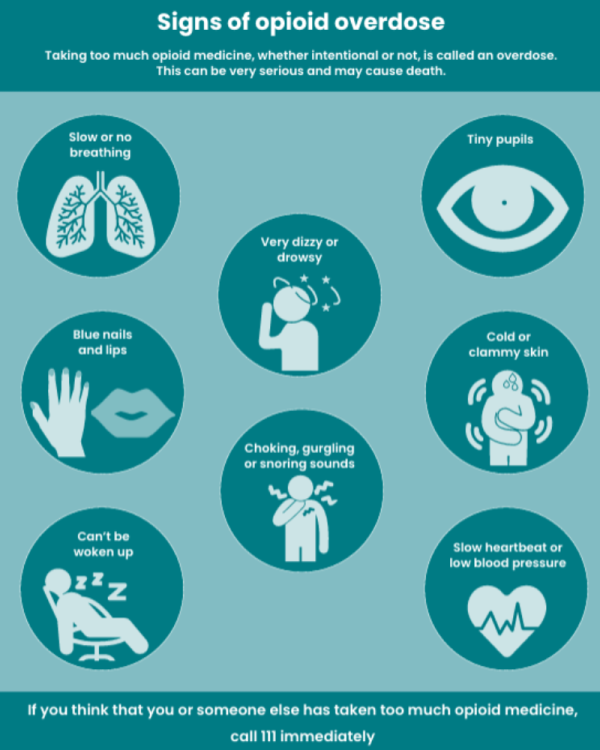
Image credit: Risks of opioid medicines Medsafe
Video: How to use injectable naloxone
For detailed instructions on how to give naloxone also see the leaflet in the emergency kit or the guides: Naloxone Injection Emergency Kit [PDF, 412 KB].
Things to remember when using naloxone
- Check the person is in a safe place and that you can't wake them up.
- Always call an ambulance (dial 111) and stay with the person until the paramedics arrive.
- Turn them on their side to prevent choking (recovery position).
- Take note of the time you give the first and second naloxone dose so you can tell the paramedics.
- A second dose is necessary if the person does not respond to the first dose. Naloxone takes a few minutes to work – allow at least 2 to 5 minutes between the first and second dose.
- If after giving the second dose the person is not breathing, apply rescue breathing (2 breaths every 5 seconds). You need to get the person breathing.
- If the person wakes up stay with them until the paramedics arrive. Naloxone only lasts 20 minutes and they could drop again.
Naloxone is active in the body for only 20 to 90 minutes, but the effects of most opioids can last longer. This means that the effects of naloxone are likely to wear off before the opioids are gone from the body, which could cause breathing to stop again. Naloxone may need to be used again, depending on the amount and type of opioids taken or the way they have been taken, either swallowed, inhaled or injected.
In Aotearoa New Zealand, only injectable naloxone is currently available. It works very quickly, usually within 2 to 5 minutes. The medication comes in a glass ampoule and must be injected into the muscle of a person experiencing an overdose.
You can get free injectable naloxone kits from:
- Your local needle exchange.
- Your doctor, who can prescribe it to you.
- Opioid substitution services.
Note: Nasal spray naloxone (known as Nyxoid or Narcan) is currently unavailable in New Zealand.
If you are taking opioids, have a plan. Talk about overdose with people you trust before it happens. Ask your healthcare provider whether you need an emergency naloxone kit.
Once you have the kit, always keep the naloxone in a place where family, friends, and close contacts can find it in an emergency. Let them know:
- that you have it, and where you keep it
- to call 111 or get emergency medical help straight away for known or suspected overdose, even if naloxone has been given
- how to recognise the signs of an overdose
- how to give naloxone in the event of an overdose
- to read the leaflet that comes with naloxone before an opioid emergency, so everyone knows what to do.
Naloxone is safe to use if you think someone might be having an opioid overdose. If it turns out not to be an overdose, it won’t cause any harm.
After receiving naloxone, the person may wake up suddenly and experience withdrawal symptoms. Symptoms of withdrawal include:
- feeling nervous, restless or irritable
- body aches
- dizziness or weakness
- diarrhoea (runny poos), stomach pain or feeling a little sick
- fever, chills or goose bumps
- sneezing or runny nose
- anxiety
- fast heart beat
- confusion.
Talk to your healthcare provider if you have questions about withdrawal symptoms.
Very rarely, people who take opioids can have more serious side effects following naloxone such as seizures, pulmonary oedema, and ventricular arrhythmias if a large dose of naloxone is given.
Research has found that having naloxone available does not encourage people to use opioids more. The goal is to prevent deaths from opioid overdose by making naloxone available and educating people about how to prevent, recognise and intervene in overdose situations.
- Community Alcohol Drugs Support Auckland(external link) NZ
- NZ Drug Foundation(external link) NZ
- Alcohol Drug Helpline(external link) general freephone 0800 787 797, text 8681, Māori, Pacific Peoples, Youth helplines.
- Alcohol and drug services(external link) Health New Zealand | Te Whatu Ora
Resources
Naloxone injection pamphlet [PDF, 412 KB] Waitematā District Health Board (WDHB), NZ
References
- Naloxone hydrochloride(external link) NZ Formulary, NZ
Brochures
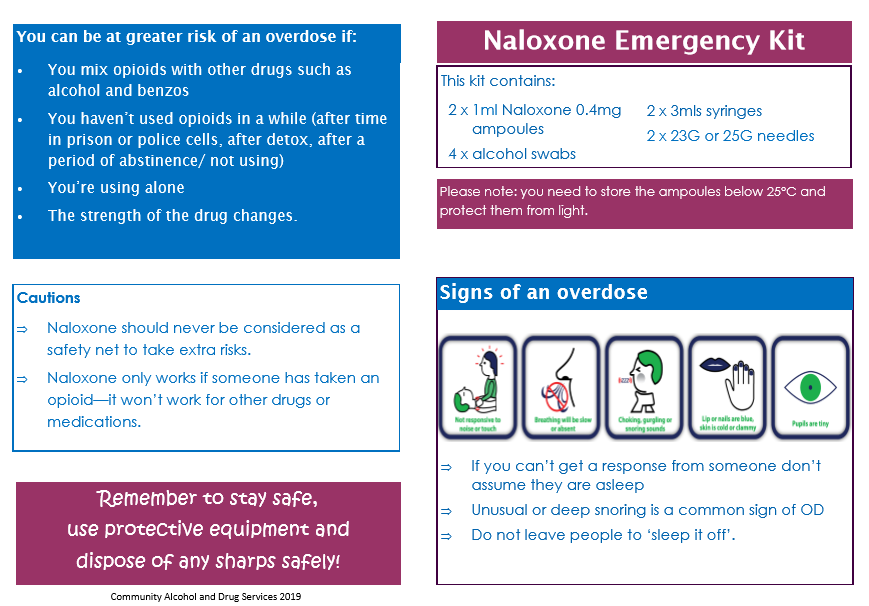
Waitematā District Health Board (WDHB), NZ
Community Alcohol and Drug Services, NZ, 2019
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated:





