You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Anticoagulants and antiplatelets
Key points about anticoagulants and antiplatelets
- Anticoagulants and antiplatelets are medicines used to prevent blood clots from forming and stop existing clots from getting bigger.
- Examples of anticoagulants are warfarin, dabigatran, rivaroxaban, enoxaparin and heparin.
- Examples of antiplatelets are aspirin, clopidogrel and ticagrelor.
- Anticoagulants and antiplatelets may be used alone or in combination with each other.
- Find out about the different anticoagulants and antiplatelets, and possible side effects.

Anticoagulants help prevent blood clots from forming and stops existing clots from growing bigger. They work by interrupting the clot-forming process and increase the time it takes for blood clots to form.
- Blood clots are clumps of blood that can be useful for stopping bleeding wounds.
- Blood clots can also block blood vessels. Blood vessels transport blood around the body, if they're blocked, blood won’t be able to reach places it needs to, including your heart or brain. Learn more about blood clots.
Anticoagulants available in Aotearoa New Zealand
| Anticoagulants that come as tablets or capsules | Anticoagulants given by injection |
|
|
| Dabigatran and rivaroxaban are also called direct oral anticoagulants (DOACs). | These are commonly used in hospital. Some people may be given these to inject at home. If you need to do this, your healthcare provider will show you how. |
When are anticoagulants used?
Anticoagulants have a variety of uses, including:
- For people with atrial fibrillation (AF), because atrial fibrillation increases the risk of stroke. A stroke is caused by AF when a blood clot forms in your heart and travels to your brain.
- For people with artificial heart valves, to protect clots developing on the valves.
- For the prevention and treatment of deep vein thrombosis, where blood clots form in veins deep within your arms, legs and pelvis. From here, the clots can travel to your lungs and cause a pulmonary embolism.
- After hip or knee surgery or some cancer therapies when your risk of blood clots is increased.
How long you need to take an anticoagulant will depend on what you're taking it for:
- Some people only need it for a few weeks (eg, after surgery), or for a few months (eg, for deep vein thrombosis).
- Others may need to take an anticoagulant for the rest of their lives (eg, people with atrial fibrillation or a mechanical heart valve).
- Your doctor will advise on what's best for you.
Anticoagulants may be used alone or in combination with antiplatelets. Read more below about antiplatelet medicines in combination with anticoagulants.
Video: How do novel oral anticoagulants (NOACs) work?
The following animation describes how anticoagulants (eg, dabigatran, rivaroxaban and apixaban) work in your body.
(British Heart Foundation, UK, 2018)
Antiplatelets are medicines that prevent blood clots from forming by stopping blood platelets from sticking together. Examples of antiplatelets include low dose aspirin, clopidogrel, ticagrelor and prasugrel (not funded).
When are antiplatelet medicines used?
Antiplatelet medicines are used to prevent blood clots in people who have:
- chest pain (from angina)
- had a stroke or mini stroke (TIA, transient ischemic attack)
- had a heart attack (myocardial infarction) and had a coronary stent fitted
- had ‘bypass surgery’ – after CABG (coronary artery bypass graft)
- peripheral vascular/arterial disease (with a stent fitted).
Antiplatelet medicines may be used alone or in combination
Depending on what it's being used for and your risk of blood clots, your healthcare provider may prescribe antiplatelets alone OR in combination.
- Antiplatelets in combination with each other: For example after a heart attack, you will usually be prescribed aspirin for life, along with another antiplatelet medication, such as clopidogrel for up to one year. This is especially important if you had a stent, as the risk of further blood clots, heart attack or stroke are higher during this period. Each medicine prevents blood clots by working in slightly different ways, which is why you may be asked to take two types.
- Antiplatelets in combination with anticoagulants: For example if you have atrial fibrillation and have had a heart attack, you are at increased risk of having a blood clot. Antiplatelet medicines work differently to anticoagulants to prevent clots.
- These medicines taken together are effective at preventing blood clots, but there’s a higher risk of bleeding. This risk increases with age. See below for signs of severe bleeding.
Depending on the treatment you're prescribed, you may take it for a few weeks or months. After this, your specialist will tell you which medicines to stop.
It’s important to check with your healthcare provider which of these medicines you need to stop and when.
When taking anticoagulants or antiplatelets, it's important to use the medicine safely and correctly. The benefits of these medicines need to be carefully balanced with possible side effects. Not enough can lead to a blood clot or stroke, but too much can lead to serious bleeding. Both anticoagulants and antiplatelets can cause bleeding, so the risk of bleeding is increased when they are taken together.
Here are some things you can do to reduce your bleeding risk when you're taking anticoagulants and antiplatelets.
- Avoid contact sports, tattoos, piercings and deep massage: These activities can increase your risk of bruising and bleeding.
- Tell all healthcare providers that you're taking anticoagulants and antiplatelets (eg, your doctor, dentist, pharmacist or podiatrist): You may need to stop taking them before surgery, dental care and some tests.
- Taking other medicines: Anticoagulants and antiplatelets can interact with some medicines and herbal supplements, so check with your doctor or pharmacist before starting them and before starting any new products. This includes over-the-counter anti-inflammatories including diclofenac (eg, Voltaren Rapid), ibuprofen (eg, Nurofen) and naproxen (eg, Naprogesic).
- Pregnancy: Warfarin, dabigatran, rivaroxaban, clopidogrel and ticagrelor aren’t usually given during pregnancy. If you're taking any of these medicines and could become pregnant, you should make sure you use contraception. If you're on these medicines and find out you're pregnant (or you're planning a pregnancy) talk to your healthcare provider.
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
References
- Rivaroxaban – a fully-subsidised oral anticoagulant(external link) BPAC, NZ, 2018
- The safe and effective use of dabigatran and warfarin in primary care(external link) BPAC, NZ, 2017
- An update on managing patients with atrial fibrillation(external link) BPAC, NZ, 2017
- Guidelines for management of bleeding with dabigatran or rivaroxaban(external link) Pharmac, NZ, 2018
- Dabigatran revisited(external link) BPAC, NZ, 2013
- Dabigatran etexilate(external link) NZ Formulary
- Oral anticoagulant selection in primary care(external link) BPAC, NZ, 2023
- Ziser K, Rahman S, Soro R, et al. The role of triple antithrombotic therapy in patients with atrial fibrillation and coronary stent insertion(external link) Aust Prescr. 2025;48:18–22
Brochures
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
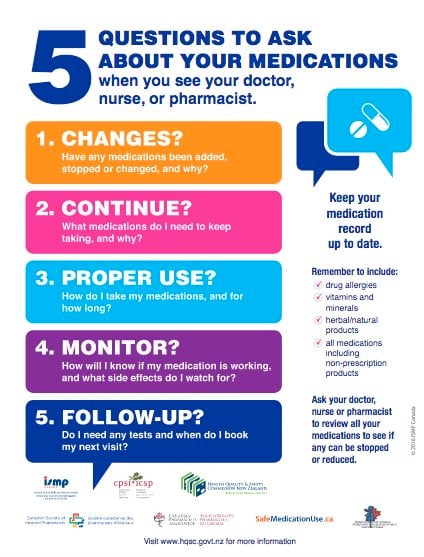
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Johanna Lim, Clinical Pharmacist – Cardiology Expert, Health New Zealand | Te Whatu Ora Te Matau a Māui Hawke’s Bay
Last reviewed:





