ACE inhibitors
Also called angiotensin converting enzyme inhibitors
Key points about ACE inhibitors
- ACE inhibitors may be used for high blood pressure, heart failure diabetic kidney disease, chronic kidney disease and after a heart attack (myocardial infarction.
- ACE inhibitors aren't suitable if you're pregnant or planning a pregnancy or if you have had angioedema, or swelling from an ACE inhibitor in the past.

Most ACE inhibitors have names that end in ‘pril’. The following ACE inhibitors are available in Aotearoa New Zealand:
- Captopril (Capoten)
- Enalapril (Acetec, Renitec)
- Lisinopril
- Perindopril (Coversyl)
- Quinapril (Accupril)
- Ramipril (Tyzan).
ACE inhibitors have many different effects on the body and are used to treat a variety of conditions. They may be used for:
- High blood pressure by relaxing and widening your blood vessels and lowering your blood pressure.
- Heart failure to help the heart pump blood more easily. This can help to relieve symptoms such as shortness of breath and swelling of feet, legs and abdomen (tummy/puku).
- Diabetic kidney disease (diabetic nephropathy) to protect your kidneys and help them to function.
- Chronic kidney disease to slow the progress of kidney disease.
- After a heart attack (myocardial infarction) to protect your heart.
ACE inhibitors can work very quickly for high blood pressure (hypertension). However, if you have heart failure it may be a few weeks or months before you notice an improvement in your symptoms. Once you have started taking an ACE inhibitor you will generally keep taking it for life unless you have a side effect.
The following animation describes how ACE inhibitors work in your body.
(British Heart Foundation, 2018)
If you're pregnant or planning a pregnancy
ACE inhibitors can affect your baby's kidneys, especially if it's taken in the second and third trimesters of pregnancy. This can result in long term damage to your baby's kidneys.
If you're already pregnant, talk to your doctor straight away. Usually your doctor will be able to prescribe a different medicine that's safe to take in pregnancy. ACE inhibitors should be stopped by the time you're 12 weeks pregnant at the latest.
Use contraception if you're taking ACE inhibitors and carefully plan any pregnancy with your GP, pregnancy specialist (obstetrician) or hospital doctor. They will want to review your medical condition and medicine before you get pregnant.
Most women stop taking ACE inhibitors before getting pregnant, but some may continue until they have a positive pregnancy test and then stop. Your doctor will discuss what's best for you, based on your medical condition and the risks and benefits of ACE inhibitors.
Severe allergic reaction (angioedema)
You shouldn't take ACE inhibitors if you've had a severe allergic reaction to an ACE inhibitor in the past, eg, swelling of your face, lips, mouth or tongue (called angioedema). Angioedema is a rare but potentially serious side effect and it can be fatal. It can occur at any time, including in people who have been taking ACE inhibitors for years. Read more about angioedema from ACE inhibitors in the side effects section below.
A blood test is usually done before starting an ACE inhibitor, and about 1 to 2 weeks after the first dose. You may also require further blood tests as your dose increases. These tests are done to check how well your kidneys are working and your sodium and potassium levels. The kidneys are affected in a small number of people who take an ACE inhibitor. While you are taking an ACE inhibitor you will need to have blood tests every few months.
Here are some things to know when you're taking ACE inhibitors. Other things may be important as well, so ask your healthcare provider what you should know about.
Have a sick day plan
If you have diarrhoea (runny poo) or vomiting (being sick) from a stomach bug, or you're dehydrated from another illness, it’s important to let your healthcare provider know. They may advise you to stop taking your ACE inhibitor for a few days, or decrease the dose and start again when you feel better. The reason for this is that ACE inhibitors can increase the amount of potassium salts in your blood, particularly if you're dehydrated.
Be careful when taking some pain relief medicines
ACE inhibitors can be used to protect your kidneys from damage if you have diabetes. However, if you're taking an ACE inhibitor and a diuretic (water pill), the combination of these with NSAIDs (anti-inflammatory pain relief medication) can be very harmful to your kidneys. It can cause acute kidney injury. This combination is called the 'dangerous trio' or 'triple whammy'. You have a higher risk of harm to your kidneys if you're also an older adult (over 65 years) or you're dehydrated.
If you are taking an ACE inhibitor with a diuretic, do not use NSAIDs for pain relief. Talk to your healthcare provider about safe pain-relief options for you. Read more about NSAIDs and protecting your kidneys.
- Examples of NSAIDs are ibuprofen (Nurofen, Brufen SR), diclofenac (Voltaren), naproxen (Noflam, Naprosyn), mefenamic acid (Ponstan), celecoxib (Celebrex), tenoxicam (Tilcotil).
- Examples of diuretics are furosemide, bumetanide, bendroflumethiazide, chlortalidone, hydrochlorothiazide, indapamide, spironolactone, eplerenone and metolazone.
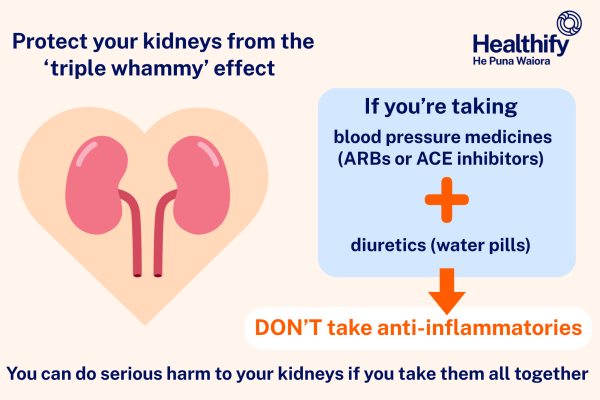
Image credit: Healthify He Puna Waiora
Read more about the triple whammy effect.
Other medicines
Let your prescriber and pharmacist know about all the other medicines you are taking. Some medicines should not be taken together with ACE inhibitors or the dose needs to be adjusted. These medicines include lithium, some types of diuretics and some medicines used for diabetes.
Like all medicines, ACE inhibitors can cause side effects, although not everyone gets them. Often side effects improve as your body gets used to the new medicine. Common side effects include headache and nausea (feeling sick) or vomiting (being sick). Some people may get a change in their taste, but this is rare. Other side effects to be aware of are dizziness, dry cough and allergic reaction.
Dizziness
Dizziness is quite common when you first start taking an ACE inhibitor, especially after the first few doses. Take special care as you're more likely to fall, especially when you stand up from sitting or lying down. You will be started on a low dose which will be slowly increased. When starting an ACE inhibitor, get up slowly out of bed or stand up slowly; take a few minutes to sit on your bed or on a chair first. The dizziness goes away after a while. If the dizziness is severe or ongoing, tell your healthcare provider.
Dry cough
This is quite common with people taking an ACE inhibitor – it happens in about 1 in 10 people. Sometimes this even happens after you have been taking the medicine for months. If you have a dry cough and it's uncomfortable, talk to your healthcare provider They may change you to a different medicine.
Allergic reaction (angioedema)
Some people taking ACE inhibitors can develop a reaction, which causes swelling of your face, eyes, mouth, lips and tongue. Swelling is a sign of a condition called angioedema and it can be dangerous. If you get these symptoms, it’s important you stop taking your ACE inhibitor and seek immediate medical attention straight away.
- Angioedema from ACE inhibitors is quite rare, affecting about 1 to 7 in 1,000 people taking ACE inhibitors (0.1% to 0.7%).
- Swelling can occur without itching, rash or hives. Some people may also have abdominal (tummy) pain and diarrhoea (runny poo). It can also affect your airways and breathing.
- Angioedema usually starts during the first weeks or months of treatment. However, it may happen at any time during the course of treatment – from hours to years after starting it.
- Swelling may still happen, even after you have stopped taking your ACE inhibitor. Seek immediate medical attention straight away.
- If you have had angioedema, or swelling from an ACE inhibitor, before let your healthcare provider know. Restarting an ACE inhibitor can cause a more severe and life-threatening reaction.
- It's very important to tell any healthcare providers that you have had an allergic reaction to your medicine, so that the same group of medicines or similar medicines are not started in the future.
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
Brochures
At home sick day advice(external link) Health New Zealand | Te Whatu Ora, 2023
Medicines and side effects(external link) Healthify He Puna Waiora, NZ, 2024
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
Brochures

At home sick day advice
Health New Zealand | Te Whatu Ora, 2023

Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Sandra Ponen, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Angela Lambie, Pharmacist, Auckland
Last reviewed:
Page last updated:






