You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Kidney disease – chronic
Also known as CKD
Key points about chronic kidney disease
- Kidney disease (mahe tākihi) is any condition that affects how well your kidneys work.
- Chronic kidney disease (CKD) refers to kidney damage that causes you to lose kidney function gradually over time.
- Diabetes and high blood pressure are the most common causes of CKD.
- Māori and Pacific Peoples with diabetes have an increased risk of CKD.
- Because most people don’t have symptoms in the early stage, see your healthcare provider regularly if you’re at risk of CKD. Finding and treating it early can prevent or slow the condition.
- Treatment includes changes to your lifestyle, medication and possibly dialysis or a kidney transplant.

Kidney disease is any condition that affects how well your kidneys work. It includes acute kidney injury and chronic kidney disease (CKD).
Chronic kidney disease (CKD) refers to kidney damage that causes you to lose kidney function gradually over time and generally can't be reversed. It includes any long-term condition that causes abnormalities in kidney structure or function for more than 3 months.
Diabetes and high blood pressure are the most common causes of CKD, and Māori and Pacific Peoples with diabetes have an increased risk of CKD.
CKD is associated with an increased risk of cardiovascular disease.
Because most people don’t have symptoms in the early stage, see your healthcare provider regularly if you’re at risk of CKD (see the risk factors below). If it’s found and treated early, it can be prevented or slowed down.
Treatment includes changes to your lifestyle, treating the underlying cause of the chronic kidney disease, such as with medicines for high blood pressure and diabetes. For severe or end stage kidney disease dialysis or a kidney transplant may be required.
Video: Understanding kidney disease
This video is also available in the following languages:
Your kidneys filter and remove waste products and excess water from your blood. Your urine (pee) is the water containing these wastes. Read more about how kidneys work.
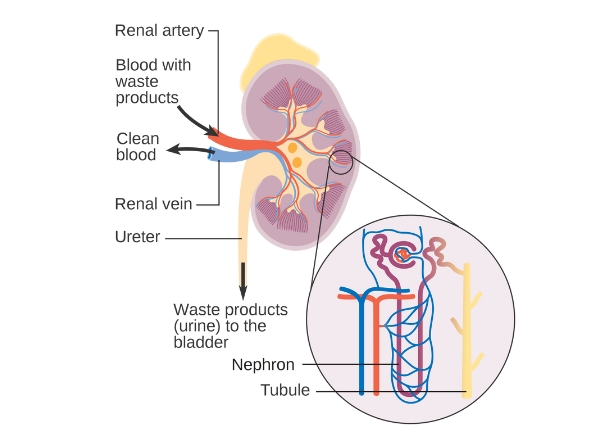
Image credit: CRUK via Wikimedia Commons(external link)
The 2 most common causes of chronic kidney disease (CKD) are diabetes and high blood pressure as they damage parts of your kidneys and limit their ability to filter your blood.
Diabetes
High levels of glucose in your blood damages many blood vessels in your body, including the blood vessels in your kidneys. About 1 in 3 people with diabetes will end up with some kidney damage. Diabetic kidney disease is also called diabetic nephropathy.
High blood pressure
High blood pressure (hypertension) damages the small vessels that take blood to the filters in your kidneys and can also damage the filters themselves.
Other causes
- Glomerulonephritis is a group of diseases that affects the filtering units in your kidneys.
- Polycystic kidney disease causes cysts to form in your kidneys. It's an inherited disease, which means that it's passed down from your parents.
- Lupus and other diseases that affect your body’s immune system can also affect your kidneys.
- Blockages caused by abnormally shaped ureters (the tubes that carry urine from your kidneys to your bladder), kidney stones, tumours or an enlarged prostate gland can affect your kidneys.
- Repeated urinary tract infections (UTIs) can also affect your kidneys. Find out about UTIs in women and UTIs in men.
You are at a higher risk of getting kidney disease if you:
- have diabetes
- have high blood pressure (hypertension)
- are extremely overweight
- have cardiovascular disease, such as coronary heart disease, cerebrovascular disease or peripheral vascular disease
- have a family history of kidney disease
- take medicines that affect your kidney health
- have some prostate conditions, such as an enlarged prostate gland
- are Māori, Pasifika or South/Indo-Asian
- are over 60 years of age
- smoke
- have previously had an acute kidney injury.
Many people with reduced kidney function don’t have any symptoms so it’s important to be tested for CKD if you have any of the above risk factors. Read more about what you can do to prevent or slow damage to your kidneys.
Chronic kidney disease (CKD) is called a silent disease because it often causes no symptoms. It's not uncommon to lose up to 70% of kidney function before developing symptoms.
The first signs of CKD may be general symptoms and can include:
- tiredness
- poor appetite and weight loss
- puffiness or swelling around your eyes and ankles
- muscle cramps
- a need to pee more often than usual
- blood in your pee
- puffiness or swelling around your eyes and ankles.
If you have symptoms or risk factors that indicate you may have chronic kidney disease (CKD), your healthcare provider will measure your blood pressure and send blood and urine samples to the lab to find out your serum creatinine, eGFR and urine ACR (see below).
Urine tests for protein
One of the main ways kidney disease is diagnosed is by the presence of albumin in your pee (urine). This is called albuminuria. Albumin is a protein found in your blood. A healthy kidney doesn’t let albumin pass from your blood into your urine, but a damaged kidney lets some albumin pass into your urine. The less albumin in your urine, the better. Sometimes albuminuria is also called proteinuria.
Your urine will also be tested in the lab to measure your urine ACR (urine albumin-creatinine ratio). Creatinine is a waste product that your kidneys usually filter out of your blood into your urine. A high urine ACR may be a sign of kidney disease.
Blood tests for kidney function
Your blood will be tested to measure creatinine and eGFR (estimated glomerular filtration rate). If your kidneys aren’t working well, the creatinine level in your blood will be higher than normal. The eGFR measures your kidney function – the lower your eGFR, the less normal kidney function you have. Read more about kidney function blood tests.
CKD is diagnosed if you have consistently decreased eGFR and/or increased urine ACR over a 3-month period, so you may have these tests done more than once. Your eGFR and urine ACR results will indicate what stage of CKD you have (its severity) which will help your healthcare team decide how it should be managed.
Other tests
If the reason for your CKD isn’t clear from your history or other health conditions, you may have other tests done. These may include:
- an HbA1c test to diagnose diabetes or to check your blood glucose level if you have diabetes
- a cholesterol test
- a full blood count
- a check for inflammation or infection with a CRP blood test, or
- testing your urine for infection or blood.
In some circumstances your healthcare provider may suggest a kidney ultrasound to look at the structure of your kidney or see if there's a blockage.
When kidney disease is detected early, changes to your lifestyle and what you eat can slow down the progress of kidney failure and prevent serious problems. See the self-care section below for information about changes you can make to your lifestyle.
Kidney disease is classified into 5 stages based on the amount of kidney damage you have and how well your kidneys are working. Your treatment will depend on what stage of kidney disease you have and what caused it in the first place.
Treatment
Depending on your individual circumstances and the severity of your kidney disease, treatment may include the following:
- Medicines to treat diabetes and hypertension, which will help reduce further damage to your kidneys. Lowering blood glucose prevents ongoing damage to kidney blood vessels by reducing inflammation and scarring. Lowering blood pressure reduces stress on kidney blood vessels. Medicines called ACE inhibitors and angiotensin receptor blockers (ARBs) help protect your kidneys by lowering blood pressure and reducing protein in the urine, slowing kidney disease progression. They are often the first choice when protein is found in your urine.
- Dialysis which is where special equipment takes over the job of filtering and cleaning your blood.
- A kidney transplant which is an operation that involves putting someone else’s healthy kidney into your body.
- Conservative treatment (also called palliative care or supportive care) includes medical care to manage your symptoms, as well as emotional, social, spiritual and practical care for you and your whānau, if dialysis or a kidney transplant aren’t appropriate.
If you have CKD your risk of cardiovascular disease is greater, so you should also have a cardiovascular risk assessment.
If you have CKD and cardiovascular disease, you may be given long-term aspirin to reduce your risk of heart attack and stroke. You may also be started on a statin (lipid-lowering treatment), especially if you have high triglyceride and low HDL cholesterol levels.
Your healthcare provider should also check any medicines you’re already taking. This includes over-the-counter medicines, such as NSAIDs, and complementary or alternative medicines. Some may need to be adjusted, switched or stopped depending on whether they have the potential to cause kidney damage. Taking certain blood pressure medicines such as ACE inhibitors and diuretics along with NSAIDs can damage your kidneys – this is called the 'triple whammy' effect. It’s important to be aware of this combination to protect your kidney health. Read more about the triple whammy.
You may be referred to a nephrologist (kidney specialist) for further assessment and management, especially if you have severe kidney disease.
If your kidney disease is detected early, lifestyle changes are important as they can help slow the progress of kidney damage and reduce your overall risk of cardiovascular disease.
Here are some things you can do.
- Avoid getting dehydrated – drink water to manage your thirst but avoid drinking too much.
- Contact your healthcare provider if you have diarrhoea (runny poo), vomiting (being sick) or other illness such as a respiratory or urinary tract infection. They may have to make changes to some of your medicines and make sure you have adequate fluid intake to reduce your risk of acute kidney injury.
- Avoid medicines that could damage your kidneys, eg, NSAIDs such as ibuprofen..
- Follow a low-salt diet, and possibly a low-potassium diet if your potassium is high, and aim to eat more plant-based than animal-based foods. You may be referred to a dietitian to help you with this and any other dietary changes needed.
- Get regular flu vaccinations.
- Check with your healthcare provider and pharmacist before you take any over-the-counter medicines or supplements.
- Have your blood pressure checked at least once a year.
Your healthcare provider may also talk to you about:
- getting support to quit smoking if you smoke
- drinking less alcohol
- doing more physical activity
- eating healthy food
- losing weight if you’re overweight.
Read more about how to protect your kidneys and chronic kidney disease and nutrition(external link).
There are traditional rongoā Māori treatments for kidney and urinary complaints, including Kawakawa (Māori Pepper Tree), Karamu (Coprosma), Manuka (Red tea tree) and Kanuka (White tea tree). If you use these, talk to your healthcare provider to check that they’re safe to use with other medicines you’re taking.
If you have severe kidney disease, you can talk to your healthcare provider about future planning. This may include creating an advance care plan.
Videos
Here are some videos on exercising when you have chronic kidney disease(external link) from the Kidney Society.
Apps reviewed by Healthify
You may find it useful to look at some diabetes apps, blood pressure apps, kidney disease apps, quit smoking apps and nutrition, exercise and weight management apps.
If you have risk factors for chronic kidney disease (CKD) but don’t have any evidence of kidney damage yet, there are things you can do to prevent or slow the development of CKD. If you are in the early stages, finding out will mean treatment can be started to prevent or slow down further damage to your kidneys.
- Ask your healthcare provider to check your kidney function – this will involve blood and urine tests. They should be done every 1 to 2 years if you have any risk factors for CKD. Ask for your urine to be checked for blood, protein and glucose.
- Have your blood pressure checked every 1 to 2 years.
- Have your blood glucose level checked for diabetes.
- Take your blood pressure and diabetes medicines if you have these.
- Don't smoke – there is no safe level of smoking and it damages your blood vessel walls.
- Have your cholesterol levels checked – high cholesterol damages blood vessels in your kidneys.
- Keep your weight within a healthy range for your height with a well-balanced diet.
- Regular exercise also helps control your weight.
- Read more about how to protect your kidneys.
Early diagnosis and treatment of chronic kidney disease can prevent or slow the progression to severe end-stage kidney disease.
If your kidney disease gets worse over time, and makes you feel very unwell because of severe kidney damage, you’ll need dialysis or a kidney transplant to treat kidney failure, or you may decide to have palliative care instead. This is when you are supported to live as well as possible for the rest of your life.
Kidney Health NZ has peer support groups(external link) around the country for people with kidney failure. These are run by trained volunteers who have experienced kidney failure in their own families/whānau, and who offer their time to talk and share stories.
Kidney Health NZ also has lots of information and resources(external link) available on their website.
The Kidney Society(external link) provides support across the Northland, Auckland, Waikato, Bay of Plenty, Tairawhiti, Hawkes Bay and Lakes regions. They can organise home visits, social work support or phone support(external link) for people with kidney disease.
The Christchurch Kidney Society(external link) provides support for patients and families of patients with advanced renal failure, including those who’ve received a successful transplant. There is a renal educator available to provide support and education to patients and whānau.
The following links provide further information on kidney disease. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
Chronic kidney disease(external link) Health New Zealand | Te Whatu Ora, NZ, 2024
Brochures
My kidney health plan(external link) NPS MedicineWise, Australia
At home sick day advice [JPG, 55 KB] Health New Zealand | Te Whatu Ora
Treatments options for chronic kidney disease(external link) Kidney Health New Zealand
Conservative treatment(external link) Kidney Health New Zealand
Looking after yourself with chronic kidney disease(external link) Kidney Health Australia
Living with kidney disease – a comprehensive guide for coping with chronic kidney disease(external link) Ministry of Health and Kidney Health New Zealand, 2018
A decision-making guide for the treatment of kidney failure – My kidneys, my choice(external link) Kidney Health Australia, 2024
Apps
Diabetes apps
Quit smoking apps
Blood pressure apps
Kidney disease apps
Nutrition, exercise and weight management apps
References
Chronic kidney disease (CKD) in adults(external link) Auckland Community HealthPathways, NZ, 2021
Chronic kidney disease – the canary in the coalmine(external link) BPAC, NZ, 2022 (updated 2024)
See the chronic kidney disease section on the kidney topics for healthcare providers page.
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Grace Lee, FRNZCGP and Clinical Educator
Last reviewed:





