Interstitial cystitis
Also known as painful bladder syndrome or bladder pain syndrome
Key points about interstitial cystitis
- Interstitial cystitis is a chronic (long-term) bladder condition that causes discomfort or pain in your bladder and pelvic areas.
- Symptoms can range from mild discomfort to severe pain. They differ from person to person and may change over time.
- You may feel an urgent need to pass urine (pee), and you may need to pee often during the day and night.
- Some things may make your symptoms worse, such as stress and certain foods and drinks.
- Treatment aims to relieve symptoms, rather than achieve a cure, and there are things you can do to help.

Interstitial cystitis is a chronic (long-term) bladder condition that causes discomfort or pain in your bladder and pelvic areas.
The image below shows the anatomy of the male and female pelvic areas.
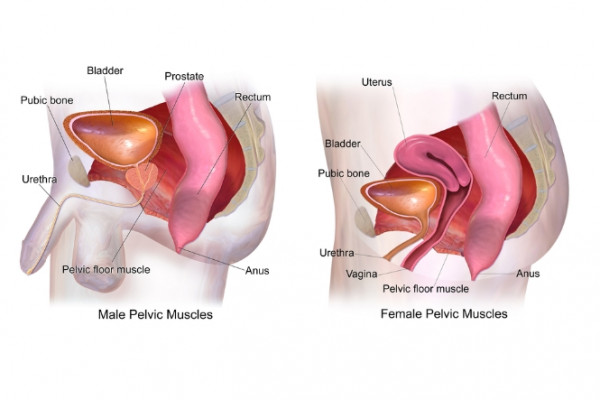
Image credit: Bruce Blaus(external link) via Wikimedia Commons
Interstitial cystitis is also known as painful bladder syndrome or bladder pain syndrome. It's more common in women than men.
Symptoms include pain when weeing and needing to wee urgently and often. You may feel pressure, discomfort or pain in your bladder and pain may get worse as your bladder fills up. Certain things may trigger your symptoms (that is, make them worse), such as stress and some foods and drinks.
Treatment for interstitial cystitis aims to relieve your symptoms and there are also things you can do yourself to help reduce them.
The cause of interstitial cystitis isn’t known, but it's not due to an infection in your bladder.
There may be a weakness in the protective lining of your bladder that means toxic substances in your urine can irritate your bladder wall.
Other things that might contribute include infection, inflammation, genetics, allergy or changes in the nerves that sense bladder changes. Sometimes stress or worries can bring on the symptoms of interstitial cystitis as well.
Risk factors for interstitial cystitis include:
- your sex – interstitial cystitis is more common in women than men
- your age – it’s more often diagnosed in people 30 years of age or older, but it can occur at any age
- having another chronic condition – people with interstitial cystitis may have other chronic pain disorders, such as irritable bowel syndrome or fibromyalgia.
The symptoms of interstitial cystitis can differ from person to person and may change from day to day. Symptoms can include:
- feeling a strong need to pee (pass urine) right away even if you’ve just passed urine (this is called urinary urgency)
- needing to pee more often than usual, sometimes as often as every 10 to 15 minutes (this is called urinary frequency)
- discomfort, pressure, tenderness or intense pain in your pelvic area (lower tummy) – this may get worse when your bladder is filling up and then goes away when you empty your bladder
- needing to get up during the night more often than usual to pee
- pain during sex.
It’s unusual to leak urine if you have interstitial cysitis.
See your healthcare provider urgently if you have pain in your lower tummy or blood in your urine as this may be a sign of a different condition.
Some people have symptom flares (when their symptoms get worse) in response to things including:
- stress
- having sex
- menstruating (having a period)
- urinary tract infection
- taking certain medicines or forgetting to take medicines
- some foods or drinks.
Foods that may make your symptoms worse include:
- citrus fruits and juices
- tomatoes
- chocolate
- coffee and caffeinated drinks
- alcohol
- spicy foods
- carbonated drinks (sodas)
- acidic foods
- artificial sweeteners
- preserved foods such as packaged meats.
There’s no single test to diagnose interstitial cystitis. Diagnosis can be difficult because the symptoms of interstitial cystitis can happen with other conditions, such as chronic urinary tract infections, prostatitis and endometriosis. Your healthcare provider will need to exclude these based on your history and investigations.
Your healthcare provider will ask you about your symptoms and may ask you to keep a bladder diary where you record the amount of fluids you drink and the amount of urine you pass/pee out. The types of questions your healthcare provider may ask include:
- How often do you feel the urge to pee with little or no warning?
- Do you feel the urge to pee straight after you’ve been to the toilet to pass urine?
- Do you ever have to pee less than 2 hours after you finished peeing?
- Do you have to get up at night to pee?
- Do you have pain or burning in your bladder area (lower tummy)?
They will also do a pelvic exam (examination of your external genitals, and vagina and cervix in females) and feel your tummy to check your internal pelvic organs (bladder, uterus). They may also examine your bottom (anus and rectum).
You’ll be asked to give a sample of your urine/pee so that a urinary tract infection can be ruled out.
You may need more tests including:
- Cystoscopy – where a small telescope is used to look inside your bladder. If a biopsy is needed (where a small piece of tissue is taken from your bladder) you will usually be given a general anaesthetic for the cystoscopy.
- Ultrasound.
- Urodynamic testing to test the function of your bladder and urethra (the tube that lets urine travel from your bladder to the outside of your body).
Video: So you have IC, now what?
There's no single treatment that works for everyone with interstitial cystitis. Treatment aims to relieve your symptoms and it may take weeks to months before your symptoms improve.
Your healthcare provider will create a treatment plan for you that may include some of the approaches described below. You may need a combination of these and, even then, your symptoms may come and go. However, over time you should be able to find treatments that give you relief and help you cope with interstitial cystitis.
Lifestyle changes
See the self-care section below for things you can do to help manage your symptoms.
Bladder training
Keep a bladder diary to record how often you pee and how often you have the urge to pee. You can then use this to train yourself to hold in your pee for longer periods so that you can gradually increase the time between bathroom visits. See the resources in the more information section below for examples of bladder diaries.
Bowel training
Some people find their interstitial cystitis symptoms improve if they have regular bowel movements, so it may help if you can train yourself to have a bowel movement (poo) at the same time each day.
Physiotherapy
A physiotherapist who specialises in pelvic floor muscles (the muscles between your pubic bone at the front and your tail bone at the back) can work with you to stretch these muscles and teach you how to keep them relaxed. This may help reduce any pelvic floor tenderness.
Other non-medicine pain treatments
Treatments such as acupuncture or transcutaneous electrical nerve stimulation (TENS), may be helpful.
Counselling
Professional counselling can help you learn ways to cope with your pain and any stress and anxiety that may be contributing to, or caused by, your symptoms. If you have other stress or worries in your life, such as work, study, money-problems or relationship issues, counselling can be very helpful and can have a positive impact on your interstitial cystitis symptoms as well.
Oral medicines
Although there isn’t any definite evidence that these work for interstitial cystitis, some people find these medicines helpful:
- Painkillers such as paracetamol and ibuprofen.
- Medicines for nerve pain such as amitriptyline, gabapentin and pregabalin.
- Medicines that reduce the urgency to pee, such as oxybutynin and solifenacin.
- Antihistamines, which can block the effect of histamine in the bladder if your symptoms might be due to an allergic reaction.
Bladder procedures
Procedures that may help include:
- ladder instillation where medicines, such as dimethyl sulfoxide (DMSO), steroid or a numbing medicine, are placed into your bladder through a thin tube called a catheter
- cytoscopy with bladder stretching (where your bladder is filled with water), which may temporarily relieve symptoms and may also detect ulcers that can be treated
- botulinum toxin (Botox) injections into the bladder
- neuromodulation therapy which uses harmless electrical impulses to change how the nerves going to and from your bladder work.
Supplements and herbal medicines
Supplements that may help you manage your symptoms include calcium glycerophosphate, glucosamine, chondroitin, quercetin complex, or aloe capsules.
Surgery
Bladder surgery is only considered if other treatments don’t provide symptom relief.
- Keep a food diary and avoid any foods or drinks that trigger your symptoms.
- Try an elimination diet(external link). This is where you stop eating foods that could trigger your symptoms and then reintroduce each food one by one and note whether your symptoms return. This should be done with supervision from your healthcare provider or a dietician.
- Your healthcare provider may recommend taking an antacid with meals if you notice that your symptoms get worse with acidic foods or drinks such as citrus fruits, peppers, carbonated drinks or tomatoes.
- Keep well hydrated by drinking enough water.
- Avoid smoking. The chemicals in cigarettes can irritate your bladder, and even if smoking doesn’t trigger your symptoms, it’s a major cause of bladder cancer so stopping smoking is a good decision.
- Be active. Even easy activities like walking or gentle stretching can help relieve symptoms.
- Try relaxation techniques, such as mindfulness, as stress can trigger symptoms in some people.
- Put an ice-pack or heat pad on your lower tummy or perineum. Your perineum is the area between your genitals (scrotum in males and vulva in females) and the opening of your rectum (anus).
- Take a warm sitz bath. This is a shallow warm water bath that you sit in to relieve pain in your perineum. Read more about sitz baths(external link).
- Relax your pelvic floor muscles by squatting with your legs wide apart.
- Try the ‘happy baby’ yoga pose. Lie on your back, press your knees against your chest, point the bottoms of your feet towards the ceiling and grab the outsides of your feet. See the image below.
- Avoid tight clothes that press on your tummy.
- If sex makes your symptoms worse, you can take pain killers beforehand and use lubricants during sex to reduce discomfort.
- Reach out for support from family and friends and other people with interstitial cystitis.

Image credit: Depositphotos
Read more about how to do the happy baby yoga pose(external link).
Apps reviewed by Healthify
You may find it useful to look at some Pain management apps and Meditation and mindfulness apps.
Some people find their interstitial cystitis symptoms get better over time and may even disappear completely with treatment. However, for many people, the symptoms come and go and treatment is needed on and off throughout their life. To help stop your symptoms coming back, it’s a good idea to continue your treatment plan even when you feel better.
Most people with interstitial cystitis can get good relief from their symptoms and live well once their pain is managed effectively with a combination of treatment approaches that have been specifically chosen for them.
The Interstitial Cystitis Association(external link) provides advocacy, information and an online support community(external link).
The NZ Painful Bladder Support Group(external link) provides a range of support and services for people with interstitial cystitis/painful bladder syndrome and their whānau.
Resources
Interstitial cystitis/bladder pain syndrome patient guide(external link) Urology Care Foundation, US
Interstitial cystitis(external link) The Royal Women’s Hospital, Victoria, Australia
Bladder diary(external link) Southland District Health Board, NZ
Your daily bladder diary(external link) National Institute for Diabetes and Digestive and Kidney Diseases, US
Apps
Pain management apps
Meditation and mindfulness apps
References
- Interstitial cystitis(external link) Mayo clinic, US, 2021
- Interstitial cystitis (painful bladder syndrome)(external link) National Institute of Diabetes and Digestive and Kidney Diseases, US, 2017
- Interstitial cystitis/bladder pain syndrome(external link) Cleveland Clinic, US, 2022
- Interstitial cystitis – painful bladder syndrome(external link) Patient Info, UK, 2021
- Bladder pain syndrome (interstitial cystitis(external link)) NHS, UK, 2022
- Interstitial cystitis(external link) Urology Care Foundation, US, 2023
Clemens JQ, Erickson DR, Varela NP, et al. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome (external link)J Urol. 2022;208(1):34–42
Interstitial cystitis/painful bladder syndrome(external link) Patient Info, UK
Interstitial cystitis, painful bladder syndrome, Hunner lesion – an overview of diagnosis and treatment(external link) International Painful Bladder Foundation
Brochures
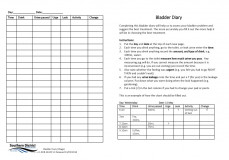
Bladder diary
Southern DHB, NZ, 2018
Interstitial cystitis/bladder pain syndrome patient guide
American Urological Association, US, 2022

Interstitial cystitis
The Royal Women's Hospital, Australia, 2018
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Mr Giovanni Losco, Adult and Paediatric Urological Surgeon, Health New Zealand | Te Whatu Ora Canterbury
Last reviewed:





