IMPORTANT: Some Health NZ hospital staff are planning to strike from Thursday 23 October to 7am Friday 24 October. Emergency departments will treat emergencies only. Find out where to get medical help.
Hyperparathyroidism
Also called parathyroid disease
Key points about hyperparathyroidism
- The parathyroid glands in your neck produce parathyroid hormone which helps control your levels of calcium and phosphorus.
- Hyperparathyroidism is when the parathyroid glands secrete too much parathyroid hormone.
- This leads to calcium coming out of your bones and into your blood and urine. This can lead to osteoporosis.
- It's most common in women after menopause.

Your parathyroid glands are 4 small glands (each about the size of a grain of rice) found in your neck close to your thyroid gland. They produce a hormone called parathyroid hormone (also called PTH).
PTH is important because it helps control the amount of calcium and phosphorus in your body. Calcium and phosphorus combine to form calcium phosphate which is the main mineral needed to make your bones and teeth hard and strong. Parathyroid hormone controls how much calcium is taken from bones and absorbed in the gut.
Hyperparathyroidism is when your parathyroid glands secrete too much parathyroid hormone. This causes levels of calcium in your blood rise, and your bones may lose calcium phosphate, leading to osteoporosis (loss of bone density). The phosphorus released is lost in your urine (pee/mimi). Calcium going through your kidneys and out into your urine can also cause kidney stones.
This picture shows where the parathyroid glands (yellow) are located in your body in relation to the thyroid gland (pink) at the base of your neck.
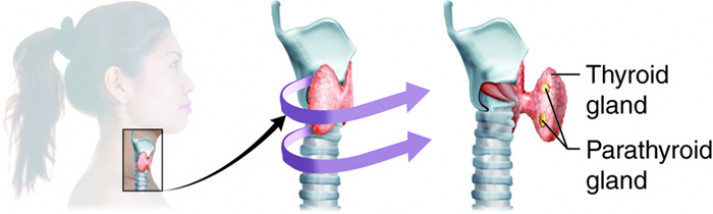
Image credit: Colorado Community College System, Anatomy & Physiology
Note: The parathyroid glands are nothing to do with the thyroid gland. Parathyroid means near the thyroid. Parathyroid disorders shouldn't be confused with an underactive thyroid or overactive thyroid.
Video: Parathyroid Glands and Hyperparathyroidism: Amazing Animation.
The video below gives a summary of hyperparathyroidism and its treatment. It may take a few moments to load.
(Norman Parathyroid Center, US, 2012)
Causes
For most people the cause of hyperparathyroidism is unknown. It may be caused by:
- benign (non-cancerous) tumours, called adenomas, in the parathyroid gland
- the parathyroid gland becoming overactive (called hyperplasia).
- cancer of the parathyroid gland, but this is rare.
Who is at risk?
Hyperparathyroidism is most common in women between 50–60 years old (after menopause). People who've had radiation therapy to their neck have a higher chance of getting hyperparathyroidism.
Many people with hyperparathyroidism have mild symptoms or none at all. Healthcare providers often diagnose the condition when high levels of calcium are found with routine blood tests.
When symptoms do occur, they're usually due to ongoing high levels of calcium. Symptoms may include:
- pain in your joints
- feeling tired
- having weak muscles
- loss of bone leading to osteoporosis
- tummy pain, nausea (feeling sick) and vomiting (being sick)
- constipation (not being able to pass poos)
- lack of appetite
- kidney stones
- feeling thirsty all the time
- passing urine more often than usual
- fast, irregular heartbeats
- depression or low mood.
Diagnosis
Healthcare providers usually diagnose hyperparathyroidism after finding a high level of calcium on a blood test. You may also be asked to take a urine test. If your bones have become weak because of abnormal calcium levels you may need to have a bone density scan.
Treatment
There are different options for treating hyperparathyroidism. The treatment you have will depend on your condition.
- Watch and wait: If the levels of calcium in your blood are only slightly high, and you don't have any symptoms, then your healthcare provider will monitor your condition on an ongoing basis. This will involve having blood tests every 6 months to check your calcium levels and how well your kidneys are working. You may also be advised to do some things to look after yourself (see below).
- Surgery: The main treatment for hyperparathyroidism is an operation to remove the gland or glands. In most cases, the operation can cure hyperparathyroidism. You are most likely to need surgery if your bones have become too thin or your kidneys are not working well.
Although hyperparathyroidism can't be prevented, there are a few things you can do to look after yourself and prevent harm to your kidneys.
- Drink plenty of fluid (6–8 cups) every day to avoid dehydration and the chance of getting kidney stones.
- Make sure you're eating a balanced diet with enough calcium and vitamin D.
- Avoid any medicines that may further increase your calcium levels, such as diuretics or lithium. However, if you're already taking one of these medicines when hyperparathyroidism is diagnosed DO NOT stop taking it unless your healthcare provider tells you to.
- See a healthcare provider for a blood test if you have vomiting or diarrhoea as you may have a sudden increase in calcium levels.
Apps reviewed by Healthify
You may find it useful to look at some Nutrition, exercise and weight management apps and Osteoporosis apps.
The following links provide further information on hyperparathyroidism. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
Hyperparathyroidism(external link) HealthInfo, NZ
Hyperparathyroidism(external link) Patient Info, UK
Apps
Nutrition, exercise and weight management apps
Osteoporosis apps
References
- Hyperparathyroidism(external link) Patient Info, UK, 2020
- Hyperparathyroidism(external link) NHS, UK, 2021
- Taniegra ED. Hyperparathyroidism(external link) Am Fam Physician 2004;69(2):333-339
- Primary hyperparathyroidism(external link) NIH, US, 2019
Hyperparathyroidism and hypercalcaemia with lithium treatment(external link) Medsafe Prescriber Update, 2014
Hyperparathyroidism(external link) Am Fam Physician 2004:69:333-90
Apps
Nutrition, exercise and weight management apps
Osteoporosis apps
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Claire Salter, Pharmacist, Tauranga
Last reviewed:
Page last updated:





