You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Kidney stones | Kōwhatu tākihi
Also known as renal calculi
Key points about kidney stones (kōwhatu tākihi)
- Kidney stones are solid crystals that form from waste products in your urine (pee).
- They may be small, but they can cause a lot of pain, known as renal colic.
- Most stones will pass out of your body when you pee.
- If a stone doesn’t pass and blocks the flow of pee or causes bleeding or an infection, it may need to be removed.
- If you're at risk of kidney stones you can help prevent them by drinking more fluid and cutting back on salt in your diet.

Kidney stones (kōwhatu tākihi) are solid crystals that form from waste products in your urine (pee). They form in your kidneys and can move into the tubes that lead from your kidneys to your bladder, known as the ureters. They can be as small as a grain of sand or as big as a golf ball.
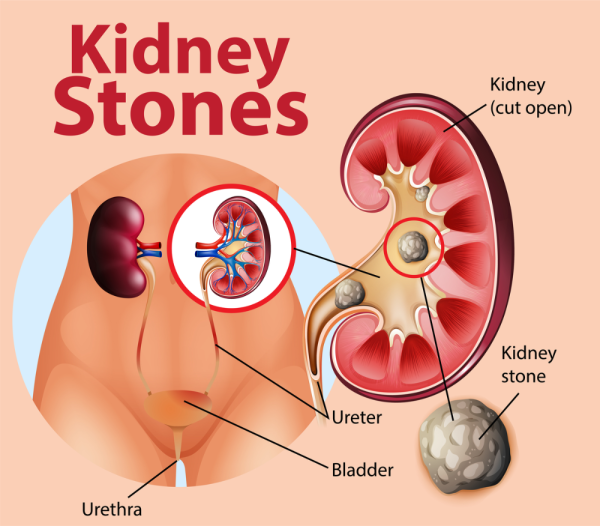
Image credit: Depositphotos
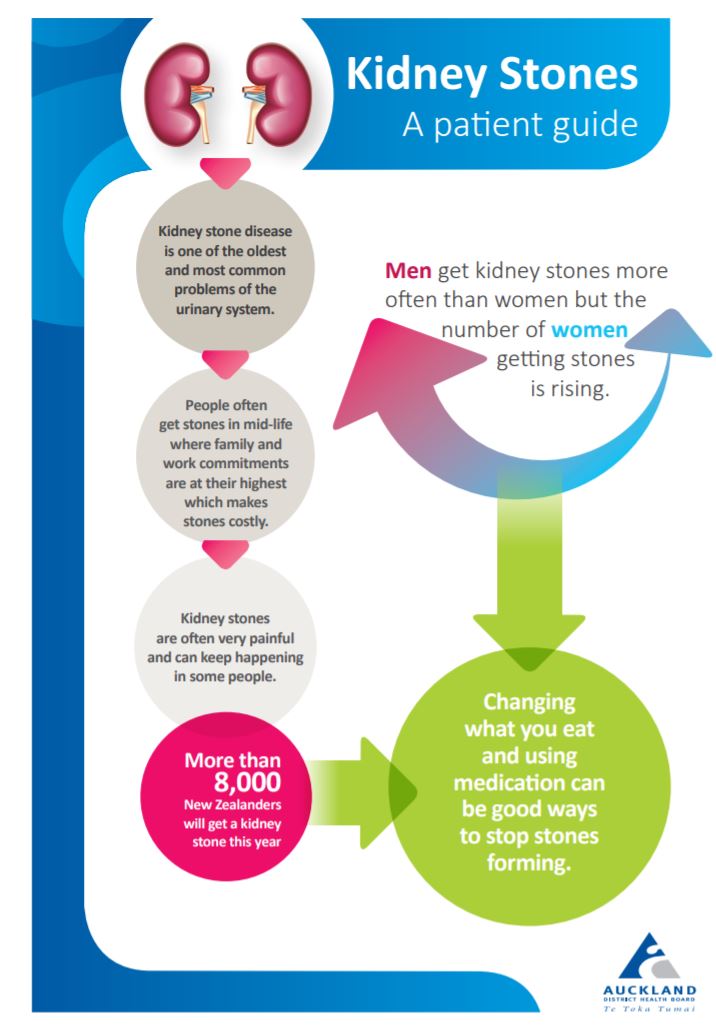
Kidney stones are more common in men than in women and can cause a lot of pain, known as renal colic.
Kidney stones can block the flow of pee and cause infection, kidney damage or even kidney failure. You can get one kidney stone or several at the same time. How they’re treated depends on what type of stone you have.
Most stones will pass out of your body when you pee. If a stone doesn’t pass and blocks the flow of pee or causes bleeding or an infection, it may need to be removed.
If you're at risk of kidney stones you can prevent them by drinking more fluid and cutting back on salt in your diet.
Video: What are kidney stones?
Click the image below to visit the website, scroll down to see the video 'what are kidney stones', then click play.  (external link)
(external link)
(NHS, UK, 2021)
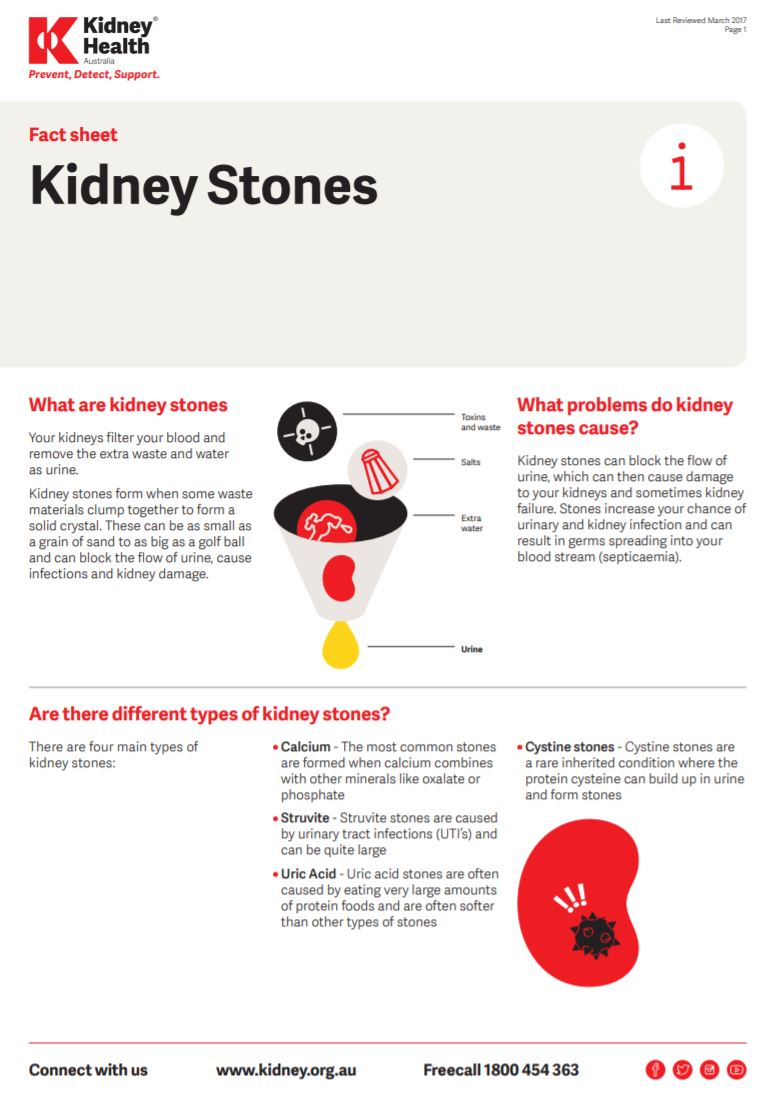
Calcium stones
Calcium stones are the most common type of kidney stone. There are 2 types of calcium stones – calcium oxalate and calcium phosphate. Calcium oxalate is by far the most common type of calcium stone.
Uric acid stones
Uric acid is a waste product that comes from chemical changes in your body. If your pee is too acidic, uric acid crystals don’t dissolve well and can form uric acid stones. About 1 in 10 stones is a uric acid stone.
Struvite stones
Struvite stones aren’t common. They’re usually caused by urinary tract infections (UTIs). Read more about UTIs in women and UTIs in men.
Cystine stones
Cystine is an amino acid that’s in certain foods and is one of the building blocks of protein. Cystinuria (too much cystine in your pee) is a rare, inherited metabolic disorder. This type of stone is very rare.
Your kidneys filter your blood and then waste products are removed in your urine (pee). Kidney stones form when there are high levels of certain minerals or salts in your pee as these waste products can form crystals that turn into stone-like lumps in your kidney over time.
There are some things that make it more likely for you to develop kidney stones.
- Dehydration (not making enough pee): This is the most common cause of kidney stones. It usually happens when your body loses too much water (eg through sweating) and you don’t drink enough, especially when doing hard exercise, or working or living in a hot place. When your pee volume is low, it’s concentrated and dark in colour. Concentrated pee means there’s less fluid to keep salts dissolved and they’re more likely to form stones.
- Diet: What you eat can also affect your chance of getting a kidney stone. For example, if you have lots of salt or animal protein in your diet you may be at higher risk of developing kidney stones. A healthy balanced dietary intake of calcium and diary products doesn't increase your risk of kidney stones.
- Family history: Having a parent or sibling who’s had a kidney stone increases your risk of getting kidney stones.
- Medicines and supplements: Medicines used for treating some conditions, such as kidney disease, cancer or HIV, can also increase your risk of developing kidney stones, as can aspirin and some antacids and antibiotics. Taking calcium or vitamin C supplements may also increase your risk of forming stones.
- Other health conditions: Health conditions such as kidney disease, obesity, chronic urinary tract infections, Crohn’s disease or ulcerative colitis, diabetes and gout can increase your risk of developing kidney stones.
Pain is usually the first sign of a kidney stone. Stones that stay in your kidney can cause mild to moderate pain just below your ribs on the side. You usually have the most severe pain, known as renal colic, when the stone moves from your kidney into your ureter (the tube that connects your kidney to your bladder). Some people have kidney stones without any symptoms.
Renal colic usually comes on suddenly, may come and go, and can be extremely painful. The pain usually starts in your back and spreads to your groin.
Other symptoms are:
- blood in your pee (your pee might look pink)
- cloudy or smelly pee (if you have a kidney infection)
- peeing frequently
- pain when peeing
- difficulty peeing
- severe back or side pain (this can include belly or groin pain)
- nausea (feeling sick) and vomiting (being sick)
- fever or chills (if an infection is present).
If you have some of these symptoms and also develop a fever or cold chills with shakes (rigors), you may have a serious infection and you should go to your healthcare provider, after hours clinic or emergency department straight away. |
Some kidney stones, called ‘silent’ kidney stones, cause no symptoms and are often found with an X-ray or ultrasound scan during a health check. Other people have their stones diagnosed when they get sudden pain while the stone is passing, and need medical attention.
Your healthcare provider will usually be able to diagnose kidney stones from your symptoms and medical history, especially if you’ve had kidney stones before.
If a stone passes out of your body in your pee, collect it (by peeing through a sieve) and take it to your healthcare provider. It can be tested to find out what kind of stone it is. This can help your healthcare provider decide on your future management. Urine and blood tests can also help to find the cause of your stone.
If you have blood in your pee or sudden abdominal or side pain, tests such as a CT scan may diagnose a stone. These tests tell your healthcare provider how big the stone is, where it is and whether you are likely to be able to pass it without intervention.
Most stones will pass out in your pee within 3 to 6 weeks without needing any treatment. During this time, you may experience renal colic (a gripping pain in your back, side or groin) that will generally be treated with strong pain relief and anti-nausea medicines from your prescriber or emergency clinic. You may also be prescribed a medicine (eg, doxazosin) to help the muscles of your ureter relax so the stone can pass through.
If the stone is too large to pass or doesn’t pass with time, you'll need treatment from a specialist doctor (urologist). The type of treatment will depend on things such as the size of the stone and where it is.
Treatments include:
- Lithotripsy – where a special machine is used that sends ‘shock waves’ through your body to break up the stone into tiny pieces> these pieces will later pass out in your pee.
- Ureteroscopy – where a small, narrow ‘telescope’ is passed up through your bladder to the stone so that the stone can be removed or broken up (sometimes with a laser).
- Percutaneous surgery (for larger stones that are still in your kidney) – where a thin telescope is passed through a small cut in your back into your kidney, to see and remove the stone.
After your treatment, you should see your healthcare provider, or go to an after hours clinic or the hospital emergency department if you:
- get severe pain that doesn’t get better with pain relief tablets
- vomit (throw up) or have a fever.
If you’ve had a kidney stone, you have an increased chance of getting another one. About 30 to 50% of people with a first kidney stone will get a second one within 5 years and then the risk reduces. However, some people keep getting stones their whole lives, including those who:
- eat a high-protein, low-fibre diet
- aren’t active or are bed-bound
- have a family history of kidney stones
- have had several kidney or urinary infections.
Here are some things you can do to reduce your risk of getting kidney stones.
Drink plenty of water
The most important thing you can do to prevent further kidney stones forming is to drink lots of fluid. Youi should drink enough to make at least 2.5 litres of pee every day. This usually means drinking about 3 litres of fluid a day.
Water is the best drink, but what matters most is getting enough fluid. Drink throughout the day and night if possible. It’s best to avoid fizzy drinks.
You’ll know if you’re drinking enough by the colour of your urine, which should be pale yellow to clear. Keeping your urine clear helps to stop waste products getting too concentrated and forming stones.
Make sure you drink plenty when it’s hot or when you’re exercising to replace fluids lost when you sweat.
Cut down on salt
Reduce your salt (sodium) intake by keeping salt in cooking to a minimum and not adding it to meals. Reducing salt lowers your risk of calcium-containing stones. Avoid processed foods and takeaway foods, and choose low or no-salt products..
Check whether you need to increase your calcium intake
If you produce calcium oxalate stones, it’s easy to think that you should reduce the calcium in your diet so there’s less calcium in your urine. However, there’s no evidence to suggest you should cut back on your calcium intake, and there is evidence to support having enough dietary calcium. This is because the calcium and oxalate bind together in your intestine and pass out of your body.
Reducing calcium in your diet might increase your risk of weak bones and osteoporosis. For adults, the recommended daily allowance is approximately 800 milligrams. You can meet this by eating 3 to 4 small-to-moderate servings of milk and dairy foods a day. One serve = a pottle of yoghurt or a glass of milk. Read more about foods containing calcium.
Ask about any other restrictions
Once you know what sort of stones you produce, your healthcare provider can tell you if you need to follow any other dietary restrictions, or they may refer you to a dietitian. For example, if you produce calcium oxalate stones you may be advised to avoid or limit certain foods containing oxalates, such as silverbeet and spinach, nuts, rhubarb, beets, tahini (sesame seeds) and soy products.
Eat healthily and maintain a health bodyweight
Keep active and maintain a healthy bodyweight. Being very overweight may change the acid levels in your pee, leading to stone formation.
Enjoy a variety of nutritious foods every day including:
- plenty of fruits and vegetables
- grain foods, mostly wholegrains
- some milk and milk products
- some legumes, nuts, fish, eggs, poultry, red meat.
Choose and prepare foods that are low in salt with little or no added sugar.
Ask about your medicines
Some medicines may increase your risk of kidney stones. However, don’t stop your medications without talking to your healthcare provider. If you're taking any prescription medicines or herbal, vitamin or dietary supplements, check with your prescriber or pharmacist whether these medicines increase your risk of forming kidney stones.
Brochures
Kidney stones fact sheet [PDF, 294 KB] Kidney Health, Australia, 2017
References
- Kidney stones fact sheet [PDF, 294 KB] Kidney Health, Australia, 2017
- Kidney stones – a patient guide [PDF, 649 KB] ADHB, NZ, 2015
- Kōwhatu tākihi Kidney stones(external link) Health New Zealand | Te Whatu Ora, NZ, 2024
- Kidney stones(external link) NHS, UK
- Renal colic and urinary tract stones(external link) Auckland HealthPathways, NZ, 2024
- Kidney stones – overview(external link) Johns Hopkins Medicine, US
- Foods high in oxalates(external link) WebMD, US, 2024
See the kidney stones section on the kidney topics for healthcare providers page.
Brochures
ADHB, NZ
Kidney Health, Australia, 2017
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Mr Giovanni Losco, Adult and Paediatric Urological Surgeon, Health New Zealand | Te Whatu Ora Canterbury
Last reviewed:





