If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Irritable bowel syndrome (IBS) | Mate tikotiko
Key points about irritable bowel syndrome
- IBS is a chronic (ongoing) gastrointestinal (gut) condition. It's not the same as inflammatory bowel disease (IBD).
- IBS can be uncomfortable but is usually harmless.
- Symptoms include bouts of abdominal (tummy) discomfort and pain, bloating and changeable bowel habits from diarrhoea (runny poo) to constipation (hard poo).
- There are simple dietary and lifestyle changes that can help improve your symptoms.
- If you have ongoing symptoms, talk to your healthcare provider about medicines to help.

Irritable bowel syndrome (IBS or mate tikotiko) is a chronic gastrointestinal condition meaning it affects your gut. Symptoms include recurring episodes of tummy discomfort or pain, bloating and varying bowel patterns.
You may also get other symptoms such as:
- fatigue
- nausea
- back pain
- headache
- pain during sex
- indigestion
- urinary frequency
- anxiety or depression.
It can seriously affect your quality of life.
It’s more commonly experienced by women and people under the age of 50 years.
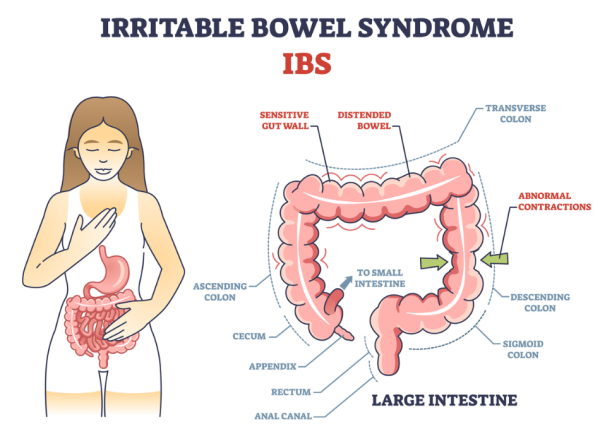
Image credit: Depositphotos
Video: What is irritable bowel syndrome?
(NHS, UK, 2022)
The exact cause of IBS isn’t known. However, there is emerging evidence that changes in your gut bacteria and inflammation of your immune system may play a role in its development.
Factors that contribute to IBS are thought to be:
- Past experiences – such as childhood stresses.
- Food sensitivities – some people have problems digesting certain foods (see below).
- Sensitivity – you may have a more sensitive gut (sometimes called ‘visceral sensitivity’).
- Digestion speed – the contents of your gut may move unusually quickly or slowly (sometimes called ‘altered gut motility’).
- Bacteria – you may have an imbalance of ‘good’ and ‘bad’ bacteria in your gut (sometimes called ‘dysbiosis’ or ‘altered faecal microbiota’).
- Leaky gut – your gut may be slightly inflamed or 'leaky' which means it may have small cracks or openings that allow partially digested food, toxins and bugs to get through the gut barrier.
- Infection – you may have had an infection, such as gastroenteritis, that trigged the IBS.
The most common symptoms of IBS
These are abdominal (belly) pain or discomfort, often reported as cramping, along with changes in bowel habits.
Usually, the pain or discomfort will be associated with at least 2 of the following 3 symptoms:
- Feeling better after having a bowel movement.
- Having bowel movements more or less often than usual.
- Having diarrhoea or constipation as defined below:
-
- diarrhoea – having loose, watery stools (poo) 3 or more times a day and feeling urgency to have a bowel movement
- constipation – having fewer than 3 bowel movements a week. Stools can be hard, dry and small, making them difficult to pass. You may find it painful and feel the need to strain to have a bowel movement. Read more about constipation and what can help.
For a diagnosis of IBS, these symptoms must occur at least 3 times a month.
Other symptoms of IBS
These may include:
- feeling that a bowel movement is not completely finished
- passing mucus – a clear liquid made by your gut that coats and protects its tissues
- urinary incontinence (not able to control your bladder)
- faecal incontinence (not able to control your bowel)
- feeling bloated.
IBS can be triggered by diet and lifestyle, especially stress and anxiety.
Mood and stress
There’s a connection between your gut and your brain known as the gut-brain axis (GBA). This includes your central nervous system and your gut sending messages backwards and forwards. Stress signals from your brain can affect your gut (for example when you get nervous before a performance or a sports event and need to rush to a toilet) and your gut can send signals back to your brain. Gut microbes are thought to play a key role in this process. Read more about the gut-brain axis(external link).
Food
Most people with IBS notice that food triggers symptoms. Common trigger foods include:
- dairy
- fatty foods
- spicy foods
- fizzy drinks
- caffeine
- artificial sweeteners.
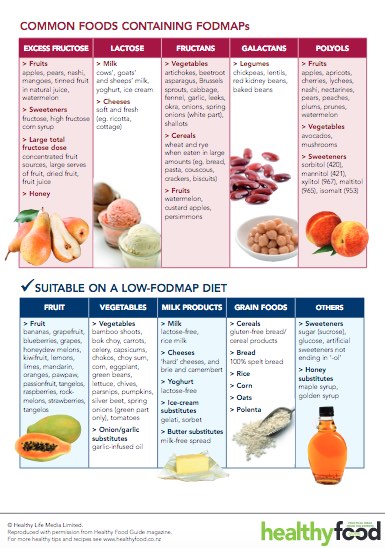
Additionally a group of short-chain carbohydrates called FODMAPs(external link) (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) are known to trigger symptoms for some people. Learn more about FODMAPS and the associated diet.(external link)
If you have the symptoms above, see your healthcare provider for a check-up.
See them immediately if have any of the following symptoms:
- unintentional or unexplained weight loss
- rectal bleeding (from your bottom) that's not due to haemorrhoids (piles)
- waking from sleep with pain or the need to empty your bowel (poo)
- symptoms first beginning when you are over 50 years of age
- a family history of gastrointestinal cancer, inflammatory bowel disease or coeliac disease
- an abdominal lump or mass
- iron deficiency anaemia.
There’s no specific test or examination for diagnosis of IBS. A diagnosis is likely to be made based on your symptoms and the length of time you’ve had them, and by ruling out other possible explanations.
Because the symptoms of IBS are similar to those of more serious conditions, you may have 1 or more of the following tests to rule them out:
- A blood test.
- Faecal (poo) testing.
- A pelvic ultrasound.
- A colonoscopy (not usually done).
It’s likely you have IBS if other possible causes of your symptoms have been ruled out and:
- you have ongoing (more than 6 months) abdominal pain at least 1 day a week that’s related to going to the toilet in the last 3 months, and
- other changes in your toilet habits (diarrhoea/constipation) and the appearance of your stool (poo).
The following approaches help a lot of people to manage their symptoms.
Make an appointment with a dietitian
A dietitian can help by looking at what you’re eating and how your diet might be affecting your symptoms. They can help with and food intolerances (such as wheat or lactose) and with trying a low FODMAP diet. Read more about common foods containing FODMAPs(external link) and the FODMAP diet and how to try it(external link).
There is also an app developed by Monash University to help you follow this diet. It's important that after a period of 4 to 6 weeks of a low FODMAP diet you start to reintroduce foods that contain FODMAPs so that you don’t have a lifetime of restricted eating and can enjoy a variety of foods.
It's strongly recommended that you get support from a dietitian throughout this process, as it's important to follow the diet correctly and to may sure you're still getting a balanced diet.
Keep a food, mood and symptom diary
Keep a diary of your symptoms and what you have changed (food or lifestyle). It will help you to see when you’re feeling better and when you’re feeling worse. Take note of how you felt emotionally as well – feelings such as stress and anxiety can affect your symptoms. Identifying what sorts of feelings or emotions trigger bouts of IBS for you can be very helpful. For example, lots of people have some mild anxiety prior to jet travel, leaving home, or sitting exams. This is not to say that IBS is a psychological problem, as the problems are in your gut. Symptoms are simply a reflection of the normal gut-brain axis that occurs at a subconscious level. If you can manage any emotional triggers, the symptoms usually settle down.
Eat mindfully and regularly
- The gut loves regularity so eating meals at regular times throughout the day (and not skipping meals!) will help your digestion. This may mean 3 main meals or 3 smaller meals with snacks in between. Intermittent fasting is not useful for people with IBS as skipping meals can slow down your digestion.
- Make sure you chew your food and eat slowly to support your digestion.
- Eat to your level of hunger. It's easy to eat out of habit so, before eating, ask yourself how hungry you are. If you’re not very hungry, have a smaller meal or snack. Stop eating when you're full or comfortable. This will also help you eat more regular meals.
Choose nourishing foods
Eat a variety of foods from the 4 food groups. Learn more about the 4 food groups and healthy eating.
Food swaps for specific symptoms
Certain foods are known to make symptoms worse.
For diarrhoea:
- Replace fluids by drinking 8 to 10 cups of water per day.
- Limit aggravating foods such as fatty foods, spicy foods, caffeine and alcohol.
- Have a break from artificial sweeteners, usually found in chewing gums and sugar free drinks.
- Slightly reduce insoluble fibre intake and slowly eat more soluble fibre. Learn more about fibre and IBS(external link).
- Try a dairy free diet for 2 weeks. Try lactose free milk, soy, oat or almond milk. Hard and semi hard cheeses such as Edam and tasty contain little or no lactose, so you can still eat these. After 2 weeks, if it makes no difference, re-introduce dairy back in.
For constipation:
- Try to slowly increase your fibre intake with whole grains, fruits, vegetables, legumes, nuts and seeds.
- Try eating porridge oats.
- Try green kiwifruit (1 to 2 per day) or prunes (1 to 4 per day).
- Drink at least 8 glasses of fluid each day.
- Try whole or ground linseed – start with 1 teaspoon per day and increase every few days to a maximum of 3 teaspoons. Make sure you have 50 mL of fluid with each teaspoon of ground linseed.
- Try psyllium husk, which is available on prescription from your healthcare provider. Start slow increasing from 10 g to 30 g over 2 to 4 doses throughout the day. Try it for 3 months.
For reflux/indigestion:
- Eat small, frequent meals.
- Sit upright after eating; leaning back or lying down will make reflux worse. Avoid eating within 1 to 2 hours of sleep.
- Avoid fizzy drinks, alcohol and caffeine.
- Reduce spicy foods and fatty foods.
Drink plenty – but choose wisely
- Try to have at least 8 cups (250 mL) of water a day.
- Caffeine can irritate your gut. Try not to have more than 3 caffeine drinks (tea, coffee, cola) each day. Reducing your coffee intake may improve your symptoms.
- Fizzy drinks may make bloating or reflux worse. Try not to have fizzy drinks.
- Alcohol irritates and speeds up the gut, so try a period of reduced alcohol.
Managing stress
Researchers have also found that reducing your stress can help to ease your symptoms. Read more about stress and how to manage it.
Physical activity
There is evidence that being more active can help with:
- stress levels
- keeping your bowels regular
- reducing your IBS symptoms.
This may be because it helps digested food move through your gut, reducing gas and bloating.
Cognitive behavioural therapy (CBT)
Because of the connection between the brain and the gut (the gut-brain axis), talking therapy such as CBT, has been found to help with managing IBS symptoms.
Gut directed hypnotherapy
There is strong evidence to suggest that gut-directed hypnotherapy improves symptoms in people with IBS by 70 to 80%. This is as effective as the low FODMAP diet and there are no restrictive diets to follow. There are clinics that offer this in person, however a lower cost option is an app such as Nerva, a 6 week programme developed by a gastroenterologist at Monash University.
Apps reviewed by Healthify
You may find it useful to look at some irritable bowel syndrome apps and nutrition, exercise and weight management apps.
Probiotics are live, beneficial bacteria found in fermented foods like yoghurt, kefir and tempeh or in pill form. The evidence to support the use of probiotics in IBS is inconclusive, there is some evidence behind certain strains so it’s best to speak to a dietitian.
Probiotics may be beneficial for some people, but in others they may increase wind and bloating.
If you want to trial a probiotic, it’s recommended you start slowly and try for a minimum of 4 weeks. If you don’t notice a change, or have an increase in your symptoms, stop taking them.
If you have tried all of the above tips and your symptoms don’t improve, it is recommended that you see a dietitian to follow a short-term low-FODMAP diet followed by a reintroduction phase.
There are medicines that can help with some symptoms of IBS such as pain, constipation or diarrhoea. Medicines can help to control the severity of the symptoms but they don't reverse or cure the condition.
Each person with IBS will have different symptoms and medicines are aimed at easing your worst
Ask your doctor, nurse or a dietitian for dietary advice. Many people with IBS find that certain foods such as FODMAPS can trigger symptoms and following a low-FODMAP diet can be beneficial.
Abdominal pain and bloating medicines
Anti-spasmodics
Medicines that relax the stomach (tummy) muscles can be used to used to relieve tummy cramps or spasm-type pain that can occur with IBS. They can also help to ease bloating. These medicines are called anti-spasmodics.
Examples of anti-spasmodics include hyoscine tablets (Buscopan® or Buscopan Forte®) and mebeverine (Colofac®).
Your healthcare provider may recommend a 1 week trial of taking these regularly. If they work, then you may be advised to use them as required, when the symptoms arise. Read more about hyoscine tablets and mebeverine.
Peppermint oil
There is some evidence that peppermint oil may be useful for bloating, wind and bowel cramps. However, for some people, peppermint oil can cause or worsen reflux (indigestion).
In Aotearoa New Zealand, peppermint oil is available as capsules (Mintec® and Colpermin®).
Your healthcare provider may recommend a trial of 1 capsule taken 3 times daily 30 to 60 minutes before meals for 2 weeks. If it's helpful, you can continue taking these, but reduce the amount you're taking to the lowest effective dose. Ask your pharmacist for advice on how to take peppermint oil capsules.
Constipation medicines
If your main symptom is constipation, laxatives may help. There are a variety of different laxatives which work in different ways. Some laxatives can cause bloating, flatulence and discomfort, which can make your IBS worse. Your healthcare provider or pharmacist can advise on the best laxative for you. You may need to try a few laxatives before you find the right one. Read more about laxatives.
Diarrhoea medicines
If diarrhoea (runny poo) is your main problem, medicines such as loperamide may be helpful to increase stool firmness, decrease stool frequency and reduce urgency. This can be used in combination with an anti-spasmodic such as mebeverine.
Loperamide works by slowing the movement of your gut, and in this way reduces the number of bowel motions and firms up runny poos.
Your prescriber will start you on a low dose and, depending on your symptoms, may increase your dose gradually. Don't take more than 8 tablets in 24 hours.
An approach that has been suggested for people who are fearful of the sudden and urgent need to defaecate (poo) that can occur with IBS, is for them to take 2 to 4 mg of loperamide approximately 45 minutes before leaving their house. This is particularly helpful if access to a toilet is limited, such as when shopping or exercising.
Note: Additional doses need to be carefully managed to avoid constipation later in the day. Discuss the best options with your doctor or pharmacist.
Another medicine that may be used for diarrhoea associated with IBS is mebeverine. Read more about loperamide and mebeverine.
Other medicines
Antidepressants
Some people may be started on a trial of antidepressants such as amitriptyline or nortriptyline. These are used to relieve pain and slow the movement of your gut, rather than to treat psychological symptoms.
You'll be started on a low dose and, if needed, your dose will be increased but only after 3 to 4 weeks. Amitriptyline or nortriptyline may not be suitable if you also have constipation. Read more about amitriptyline and nortriptyline.
Probiotics
There is some evidence to support the use of probiotics for irritable bowel syndrome. A 4-week trial of probiotics in the form of yoghurts or other fermented milk products can be considered. However, some of these products also contain ingredients that may make IBS symptoms worse, such as fructans, fructose or lactose. If there's no improvement after 4 weeks, stop. A probiotic containing bifidobacterium infantis 35624 has the most evidence for its use. Read more about probiotics.
IBS Central(external link) Monash University, Australia
IBS resources(external link) Monash University, Australia
A Little Bit Yummy(external link) FODMAP made easy (paid membership)
Starting the low-FODMAP diet(external link) Monash University, Australia
Brochures
Trouble going to the loo? [PDF, 1.1 MB] Healthify He Puna Waiora, NZ
Common foods containing FODMAPs(external link) Healthy Life Media, NZ
Monash University low FODMAP diet guide(external link) Monash University, Australia
Apps
Irritable bowel syndrome apps
Nutrition, exercise and weight management apps
References
- Irritable bowel syndrome in adults – not just a gut feeling(external link) BPAC, NZ, 2014
- Irritable bowel syndrome(external link) Auckland Regional HealthPathways, NZ, 2020
- Irritable bowel syndrome(external link) Crohn’s & Colitis, NZ
- Gut brain axis (GBA)(external link) Physiopedia, UK, 2021
- Low FODMAP diet efficacy in IBS patients – what is the evidence and what else do we need to know?(external link) NZ Medical Journal, 2016
- Johannesson E, Ringström G, Abrahamsson H, et al. Intervention to increase physical activity in irritable bowel syndrome shows long-term positive effects(external link) World J Gastroenterol. 2015;21(2):600–608
- Qin H-Y, Cheng C-W, Dong Tang X-D, Bian Z-X. Impact of psychological stress on irritable bowel syndrome (external link)World J Gastroenterol. 2014;20(39):14126–14131
- Kinsinger SW. Cognitive-behavioral therapy for patients with irritable bowel syndrome – current insights(external link) Psychol Res Behav Manag. 2017;10:231–237
- How effective is gut-directed hypnotherapy in people with IBS?(external link) Monash University, Australia
Clinical pathways and guidelines
Telehealth clinical module – abdominal assessment(external link) ProCare, NZ, 2022
Irritable bowel syndrome – full guidelines and other resources(external link) National Institute for Health & Clinical Excellence UK, Updated 2017
Resources
- Kortlever T, Hebblethwaite C, Leeper J, et al. Low FODMAP diet efficacy in IBS patients – what is the evidence and what else do we need to know?(external link) NZMJ 2016;129(1442):75–83
- But I am not depressed – antidepressants for irritable bowel syndrome(external link) Tools for Practice, US, 2020
- Irritable bowel syndrome in adults – not just a gut feeling(external link) BPAC, NZ, 2014
- Irritable bowel syndrome in adults – not just a gut feeling – peer group discussion(external link) BPAC, NZ, 2014
- Kortlever TL, Huinink STB, Offereins M. Low‐FODMAP diet is associated with improved quality of life in IBS patients – a prospective observational study(external link) Nutr Clin Pract. 2019, 34(4): 623–630.
- Treatment of irritable bowel syndrome in adults(external link) UpToDate, 2018
- Qin H-Y, Cheng C-W, Dong Tang X-D, Bian Z-X. Impact of psychological stress on irritable bowel syndrome(external link) World J Gastroenterol. 2014 Oct 21; 20(39): 14126–14131
- Schaper SJ, Stengel A. Emotional stress responsivity of patients with IBS - a systematic review(external link) J Psychosom Res. 2022 Feb;153:110694
- Mayer EA, Ryu HJ, Bhatt RR. The neurobiology of irritable bowel syndrome(external link) Mol Psychiatry. 2023 Apr;28(4):1451–1465
- Johannesson E, Ringström G, Abrahamsson H, Sadik R. Intervention to increase physical activity in irritable bowel syndrome shows long-term positive effects(external link) World J Gastroenterol. 2015 Jan 14; 21(2): 600–608
- Wang XJ, Thakur e, Shapiro, J. Non-pharmaceutical treatments for irritable bowel syndrome(external link) BMJ 2024;387:e075777
Continuing professional development
Simplifying IBS – targeted management that isn’t just FODMAPS(external link) Goodfellow Unit Webinar, NZ, 2020
Irritable bowel syndrome by Dr Adele Melton(external link) The Goodfellow Unit, NZ, 2018
Low FODMAP online training(external link) Monash University, Australia
Irritable bowel syndrome in adults(external link) BMJ Learning, UK, 2024
Wilson H, et al. Te Kete – diagnosis and explanations for patients with 'persistent somatic symptoms' and chronic pain(external link) NZ, 2024
Brochures
Healthy Life Media, NZ
Monash University, Australia
Healthify He Puna Waiora and Mediboard, 2023
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Derek JY Luo, MBChB (Otago) FRACP, Consultant Gastroenterologist
Last reviewed:
Page last updated:





