You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Recurrent urinary tract infections (UTIs)
Key points about recurrent urinary tract infections
- A urinary tract infection (UTI) is an infection in any part of the urinary system. They are more common in females but males can also get them. They can also happen at any age.
- UTIs can be more frequent at certain times such as pregnancy, with sexual intercourse, ageing, having a urinary catheter, around your menstrual period, or having atypical anatomy (eg, after surgery).
- Recurrent UTIS are when you get at least 3 in a year, or 2 in 6 months.
- Find out how they're managed and things you can do to prevent them.

A urinary tract infection or UTI is an infection in any part of the urinary system – kidneys, ureter (tube between your kidneys and your bladder), bladder and urethra (tube from your bladder to the outside). UTIs are common, about half of all females have at least 1 during their lifetime and about a quarter of these will have at least 1 more. If you have at least 3 in a year or have had 2 in the last 6 months, they’re described as recurrent UTIs.
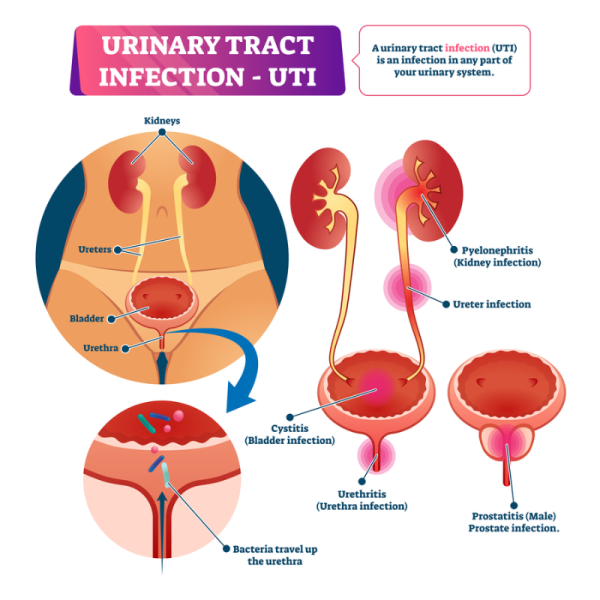
Image credit: Depositphotos
Different things can cause recurrent UTIs, some relate to getting older.
If you haven’t reached menopause (when your periods stop) they can be due to:
- having a UTI caused by an atypical or antibiotic-resistant bacteria or a fungus
- having underlying kidney stones
- your anatomy
- having sexual intercourse
- using spermicide
- being pregnant
- having a new sexual partner
- having a mother who had UTIs
- having UTIs as a child
- weak muscles around your bladder and walls of your vagina (cystocele)
- not being able to empty your bladder properly when you pee
- having a urinary catheter (a tube in place to drain your bladder)
- having urinary incontinence (bladder control problems).
If you’ve reached menopause, and your periods have stopped, the causes include:
- having a history of UTIs before you reached menopause
- genitourinary syndrome of menopause (changes to your vagina, bladder and sexual feelings because of menopause).
Symptoms of a UTI can include:
- pain or burning during or immediately after peeing (dysuria)
- feeling the need to pee more often
- needing to pee without much notice
- needing to pee more often than usual during the night (nocturia)
- pain in your lower tummy (abdomen)
- suprapubic pain (pain just above your pubic bone)
- urine (pee) that smells bad or looks cloudy or reddish.
However, older women may have different symptoms such as feeling generally unwell, being confused, feeling sleepy or losing bladder control (incontinence).
UTIs may also be difficult to recognise in young children because the symptoms and signs may be vague and unclear. Sometimes the only symptom may be a fever with no clear cause. Read more about UTIs in children.
The diagnosis of a UTI is based on a discussion with a healthcare provider about your symptoms, and an examination. You may be asked to provide a urine sample to identify the type of bacteria causing it.
Recurrent UTIs are when you have more than 2 in 6 months, or have at least 3 in a year. If you’re having repeated UTIs, you may need further tests, such as:
- swabs for sexually transmitted infections (if appropriate) or other bacterial or fungal infections.
- a blood test to check your blood glucose levels.
- an ultrasound scan to look at your urinary system in case you have a problem such as a kidney stone.
One of the best ways to manage recurrent UTIs is to do what you can to prevent them coming back – see the prevention section below. However if these things don’t work, and you keep getting them, you may be put on a low dose of antibiotic for weeks or even months to try and get rid of the bacteria and prevent it coming back. Taking antibiotics for a long time isn’t appropriate for everyone (eg, if you’re pregnant/hapū) and can add to the antibiotic resistance problem. Read more about antibiotic resistance.
If you have recurrent UTIs that are linked to a known trigger (eg, sexual intercourse or menstruation), a single or short dose of antibiotics may be prescribed for you to take at specific times. Your healthcare provider will advise you on when to take it.
An alternative is a medicine called Hiprex which makes your urine more acidic and discourages the growth of bacteria. It may work as well as low dose antibiotics for preventing UTIs. In Aotearoa New Zealand it’s available with a prescription from your healthcare provider or from your pharmacy after you’ve talked to a pharmacist. It’s not suitable if you're taking some types of antibiotic as it can make you more likely to form kidney stones.
If your UTIs are hard to manage, you may be referred to a urologist (doctor who specialises in urinary problems).
Vaccination
A vaccine called Uromune (MV140) is available in Aotearoa New Zealand but it’s not currently approved or funded, which means you’d have to pay for it yourself. Read more about unapproved medicines. Uromune can be prescribed by your healthcare provider and is given as a spray under your tongue once a day for 3 months. A number of small studies have shown it can work to prevent (or limit) recurrent UTIs for up to a year, but it may not work for everyone. Talk to your healthcare provider if it’s something you’d like to try.
There are things you can do to help prevent UTIs coming back.
- Look after yourself and stay as healthy as you can. This means managing any health conditions (eg, diabetes), eating and drinking sensibly, being physically active and getting plenty of rest.
- Drink plenty of water (aim for 2 litres a day if possible) to stay hydrated. This is especially important if you’re an older person.
- Try to avoid getting constipated (hard poo that’s hard to pass). Being constipated can put pressure on your bladder and stop it emptying fully when you pee. Drinking plenty of water and eating foods high in fibre, such as fruit and vegetables and wholegrain breads and cereals, will help with this. Read more about constipation.
- Urinate (pee) when you need to, don’t ‘hold on’.
- Try to empty your bladder fully. Once you think you’ve finished peeing, wait a few seconds then try again.
- If you use tampons, change them after a bowel movement (poo).
- Urinate (pee) before and after having sex.
- Avoid contamination of bacteria from poo. Wipe your bottom from front to back after going to the toilet.
- Change your underwear daily and if it gets soiled.
- Wash underwear at a high enough temperature to kill bacteria and fungi.
- Use a lubricant when having sexual intercourse.
- Avoid using spermicides, spermicide-coated condoms and diaphragms.
- If you no longer have periods, vaginal oestrogens may help, talk to your healthcare provider about a prescription.
- Take any antibiotics you’ve been prescribed and make sure you finish the course.
- Don't let perfumed products, including soaps, come in contact with your genital area.
- Do pelvic floor exercises to help control symptoms. You might find it helpful to work with a pelvic floor physiotherapist. Find a physio by searching for 'pelvic health – women's' or 'pelvic health – men's' on the find a physio(external link) website.
See the section below for information about other possible approaches to treating and preventing recurrent UTIs you may want to talk to your healthcare provider about.
A few alternative treatments may help with repeated UTIs, but there’s not enough evidence for them so they’re not routinely recommended.
D-mannose
Your cells produce a sugar called mannose which covers the lining of your urinary tract. When you have a UTI, the bacteria stick to the mannose on the inner walls of your bladder with little finger-like projections (fimbria) and can move up into your ureter.
D-mannose is another type of sugar that’s naturally created by your body and is also found in foods such as apples, grapes, watermelon and cranberries. It sticks to the bacteria and stops them from attaching themselves to the inside of your urinary tract. This makes them easier to flush out when you pee.
A review of research into using D-mannose for treating or preventing UTIs found there wasn’t enough evidence to say whether it helped or not. However, it wasn’t found to be harmful – the main side effects are likely to be diarrhoea (runny poo) and vaginal burning. Until more is known, it’s not clear how much to take and whether it interacts with other medicines you may be taking.
Probiotics
Probiotics are live bacteria and yeasts that can help your digestive system. Probiotics containing lactobaccilus may be helpful for urinary and vaginal health as they help to change the level of acidity in your vagina. This makes it harder for bacteria to grow and then travel into your urinary system. Again, there’s not enough research evidence to know if they’re useful, but they may be worth trying if they’re safe for you to take.
It’s important you talk to your healthcare provider first because some people with immune system problems or serious health conditions shouldn’t take them. Some people get mild side effects including an upset stomach, bloating and diarrhoea (runny poo) for a few days. They may trigger an allergic reaction as well. Stop taking them if you have any problems and talk to your healthcare provider. Read more about probiotics.
Cranberries
There’s evidence to suggest consuming cranberries (juice, tablets or capsules) can reduce the number of recurrent UTIs experienced. However, how much you should have or for how long isn’t clear. It’s likely that products containing a higher concentration of cranberry will work better. Drinking too much cranberry juice may upset your tummy or gut and may not be good if you’re limiting your daily intake of sugar. Note that there’s not enough evidence to recommend cranberry products for older or pregnant people.
References
- Recurrent UTIs in women(external link) Auckland Community HealthPathways, NZ, 2021 (updated 2024)
- Urinary tract infection in children(external link) Auckland Community HealthPathways, NZ, 2023
- Urinary tract infections (UTIs) – an overview of lower UTI management in adults(external link) BPAC, NZ, 2025
- What is D-mannose?(external link) MedicalNewsToday, US, 2024
- Prevention of recurrent urinary tract infections(external link) Urology Care Wellington, NZ
- UTI treatment(external link) Chronic UTI Australia Inc.
- Urinary tract infection (UTI)(external link) Sexual Wellbeing Aotearoa, NZ
- Preventing lower urinary tract infections(external link) NHS, UK, 2020
- Cooper TE, Teng C, Howell M, et al. D-mannose for preventing and treating urinary tract infections(external link) Cochrane Database Syst Rev. 2022;8:CD013608
- What are probiotics?(external link) WebMD, US, 2024
- William G, Hahn D, Stephens JH, et al. Cranberries for preventing urinary tract infections(external link) Cochrane Database Syst Rev. 2023;4:CD001321
- What doctors wish patients knew about UTI prevention(external link) American Medical Association, US, 2025
See the UTIs section on the urinary topics for healthcare providers page.
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Lottie Wilson, General Practitioner, Queenstown
Last reviewed:





